Introduction: The infection with SARS-CoV-2 that affects the entire world has been shown to be more severe in patients with comorbidities. The object of this study was to know the survival of renal transplant patients infected with this coronavirus.
Material and methods: Eligible were renal transplant patients with SARS-CoV-2 infection requiring hospitalization (moderate and severe degree) from the start of the pandemic to September 28, 2020. Survival analysis was performed with Kaplan-Meier tables in days, using statistical package SPSSw v25.
Results: Data was collected for 66 patients from 4 renal transplant facilities; the mean age was 39.5 years (IQR 30.0-49.5); global survival was 59.10%. Difference of 67.50% vs 46.15% was observed between receivers from living and dead donors respectively (without Log Rank significance of 0.068); 70.25% survival in patients with low immunological risk and 44.82% for high risk (Log Rank 0.034).
Conclusions: Comorbidities and immunosuppression greatly influence mortality in renal transplant patients immunological risk presents an important determinant of patient survival.
COVID-19, kidney disease, SARS-CoV-2, renal transplant, survival
Disease by coronavirus (COVID-19) is a disease with high transmission, and has represented a general problem in the world, with significant morbidity and mortality [1]. People with renal transplant, through their condition of immunosuppression, are more susceptible, show more progression to pneumonia, acute graft dysfunction, and a higher possibility of over infection and of presenting a higher number of comorbidities [2]. Pneumonia in transplanted patients is more severe, with worse results; clinical symptoms have been described with dyspnea in 70.8%, fever (62.5%), followed by cough in 45.8% and with findings in ground glass tomography in 95.8% of cases [3-5]. Even so, there are many questions concerning the behavior of transplanted patients that suffer with COVID-19 [6].
It is recommended that transplanted patients with mild cases be handled as outpatients, with the recommendation of quarantine and alarm systems to recognize a moderate or severe case [7]. In some studies reported cases, in these patients with immunosuppression, infection with coronavirus may be grave and require hospital admission, [8-9] and the majority of these patients reduced their immunosuppression and were treated with support therapy; which included the suspension of inhibitors of calcineurin or rapamycin in mammalian cells, or mTOR (mammalian Target of Rapamycin), in addition of anti-proliferative drugs, in this case azatioprin or mycophenolate mofetil [10-12].
The handling of immunosuppression in the transplanted patient infected with SARS-CoV-2 is varied in regards to symptomology, age, comorbidities and the severity of COVID-19, which determines the best strategy; mild cases without comorbidities, and youths should continue immunosuppression in the same way, and those with comorbidities should consider reducing azatioprin, mycophenolate or mTOR [13-14]. Moderate and severe cases should consider the suspension of immunosuppression, maintaining only endovenous steroids, mainly methylprednisolone, in addition to considering restarting previous immunosuppression, first calcineurin inhibitor, from 5 to 15 days after symptoms have disappeared [13].
Design
A prospective cohort of renal transplant patients from the Instituto Mexicano del Seguro Social (IMSS) belonging to 4 renal transplant units in Mexico were studied.
Patients
Eligible were patients insured by IMSS with kidney transplant infected with SARS-CoV-2 from the beginning of the pandemic to September 28, 2020, who required hospitalization for moderate or severe infection.
Obtaining data
The data of interest were: age, weight, gender, biochemical parameters, type of renal donor, comorbidities, induction used, immunological risk, days of hospitalization, days of medical care, onset of symptoms, acute graft dysfunction, need for renal replacement therapy (RRT), need for mechanical ventilator, and clinical outcome.
Statistics
Data are presented as mean and standard deviation for continuous variables, or as frequency or means and interquartile range for nominal variables or those with skewed distribution. The difference of means was established with chi squares or Student t. Analysis of survival was performed with Kaplan-Meier tables in days. Statistical significance was established with p <0.05. Analysis was performed with the statistical package SPSSw v25.
Data was collected from 66 patients with renal transplant that suffered infection with moderate or severe SARS-CoV-2 who required medical hospitalization. A general analysis was made of the general characteristics of the patients and biochemical parameters, as well as the difference between patients returned home due to improvement and those who died. 39 patients returned home due to improvement (59.10%), 27 patients died (40.90%). The mean age was 39.5 years, with interquartile range (IQR) of 30.0 to 49.5 years. Baseline creatinine previous to infection with coronavirus was 1.30 mg/dl as mean, with IQR of 1.10 to 1.70 mg/dl, which was also elevated upon entry of patients, with a mean of 1.67 mg/dl (IQR of 1.11-3.57 mg/dl), due to multiple factors that caused acute dysfunction in many of the patients from entry. See the biochemical parameters on Table 1.
Table 1. Baseline characteristics. Transplant patients with moderate or severe COVID-19
| |
Total (66 px) |
Returned home (39 px) |
Died (27 px) |
Variable |
Mean |
IQR |
Mean |
IQR |
Mean |
IQR |
p (*) |
Age (years) |
39.5 |
30-49.5 |
36 |
28-48 |
40 |
33-54 |
0.471 |
Weight (kilograms) |
65 |
55.75-74.00 |
64 |
55-71 |
65 |
59-78 |
0.208 |
Height (meters) |
1.6 |
1.55-1.67 |
1.6 |
1.54-1.67 |
1.58 |
1.55-1.68 |
0.739 |
Days transplanted (days) |
1941 |
583-3785 |
2554 |
1294-4239 |
1125 |
340-3358 |
0.119 |
Baseline creatinine |
1.3 |
1.1-1.7 |
1.3 |
1.2-1.5 |
1.3 |
1.1-1.8 |
0.739 |
Days of hospitalization |
8 |
5-14.25 |
8 |
5.0-17.0 |
8 |
3.0-12.0 |
0.240 |
Days between symptoms and medical care |
5 |
2-7 |
4 |
1.0-10.0 |
7 |
4.0-10.0 |
0.296 |
Glucose (mg/dL) |
112 |
89-168 |
104.5 |
75-140 |
111.75 |
92-365 |
0.013 |
Urea (mg/dL) |
50 |
26.5-122 |
20.25 |
13.5-39 |
150.5 |
51-215 |
0.008 |
Creatinine (mg/dL) |
1.67 |
1.11-3.57 |
1.37 |
1.04-1.56 |
4.46 |
1.27-10.39 |
0.008 |
Sodium (mEq/L) |
135 |
130-139 |
137 |
135-139 |
129.5 |
126-131 |
0.235 |
Potassium (mEq/L) |
4.5 |
3.85-5.4 |
4.15 |
4.10-4.32 |
5.5 |
3.37-7.47 |
0.139 |
Albumin (g/dL) |
3.6 |
3.2-3.8 |
3.45 |
2.6-3.9 |
3.2 |
2.87-3.82 |
0.158 |
Uric acid (mg/dL) |
5.2 |
5.1-6.7 |
5.2 |
5.1-5.3 |
7.75 |
5.2-11.27 |
0.100 |
Leukocytes (103 /uL) |
7500 |
5100-12300 |
7800 |
5350-11900 |
6915 |
4500-13840 |
0.678 |
Hemoglobin (g/dL) |
12.5 |
11.0-14.6 |
13.3 |
11.6-14.65 |
11.75 |
10.2-14.52 |
0.249 |
Neutrophils (103 /uL) |
6350 |
3770-10000 |
6760 |
3747-9565 |
5645 |
3582-11602 |
0.922 |
Fibrinogen (g/L) |
692 |
589.5-920 |
790 |
530-985 |
682 |
618-858 |
0.918 |
D dimer (ng/mL) |
182 |
3.08-615.5 |
231 |
3.48-596 |
182 |
2.4-696 |
0.495 |
C reactive protein (mg/L) |
151 |
21-253 |
29.4 |
11.1-44 |
191 |
66.45-313.35 |
0.244 |
Ferritin (ng/mL) |
741.7 |
316.9-1512.7 |
869 |
337-1073 |
614 |
250-2317 |
0.678 |
(*) expressed in Student t |
|
|
|
|
|
|
|
COVID-19: coronavirus disease; px: patients; IQR: interquartile range |
Statistically significant differences were found between the two groups, returned home compared with died, in glucose levels, urea and creatinine (Table 1).
Of the total, 41 were male (62.10%), the most frequent comorbidity was hypertension (HT) in 51 patients (77.30%), diabetes was second in 18 renal receivers (27.30%), followed by obesity with 16 persons (24.20%). By type of donor, the majority were from living donors, 40 cases (60.60%), 26 from deceased donors (39.40%). Current induction and immunosuppression is observed in Table 2.
Table 2. Comorbidities, peri-transplant characteristics, outcomes
| |
|
Total (66 px) |
Returned home |
Died (27 px) |
|
Variable |
Frequency |
% |
Frequency |
Frequency |
p (*) |
Sex |
|
|
|
|
0.690 |
| |
Male |
41 |
62.1 |
25 |
16 |
|
| |
Female |
25 |
37.9 |
14 |
11 |
|
Hypertension |
51 |
77.3 |
26 |
25 |
0.013 |
Diabetes mellitus |
18 |
27.3 |
9 |
9 |
0.358 |
Obesity |
16 |
24.2 |
7 |
9 |
0.152 |
Pulmonary disease |
2 |
3.0 |
0 |
0 |
0.084 |
Type of donor |
|
|
|
|
0.085 |
| |
Living |
40 |
60.6 |
27 |
13 |
|
| |
Deceased |
26 |
39.4 |
12 |
14 |
|
Induction |
|
|
|
|
0.127 |
| |
Basiliximab |
31 |
47.0 |
22 |
9 |
|
| |
Thymoglobulin |
29 |
43.9 |
16 |
13 |
|
| |
Without induction |
6 |
9.1 |
4 |
2 |
|
Immunosuppression |
|
|
|
|
0.569 |
| |
Tacrolimus-MMF-PDN |
36 |
54.6 |
21 |
15 |
|
| |
Tacrolimus-AZA-PDN |
7 |
10.6 |
5 |
2 |
|
| |
Sirolimus-MMF-PDN |
13 |
19.7 |
10 |
3 |
|
| |
Sirolimus-AZA-PDN |
1 |
1.5 |
1 |
0 |
|
| |
Cyclosporin-MMF-PDN |
9 |
13.6 |
3 |
6 |
|
Acute graft dysfunction |
39 |
59.1 |
19 |
20 |
0.039 |
Need for RRT |
10 |
15.2 |
2 |
8 |
0.005 |
Mechanical ventilation |
27 |
40.9 |
4 |
23 |
0.001 |
Returned home due to improvement |
39 |
59.1 |
39 |
0 |
0.001 |
(*): expressed in chi squared |
px: patients; MMF: mycophenolate mofetil; PDN: prednisone; RRT: renal replacement therapy |
|
The differences between groups were observed in the presence of hypertension only among the comorbidities; in the case of outcomes this difference was observed in acute graft dysfunction, the need for renal substitution therapy, mechanical ventilation and those who returned home due to improvement (Table 2).
The main complications, in addition to the respiratory ones expected due to the severity of the infectious disease, were acute graft dysfunction, which was presented in 39 transplants (59.10%), and the need for renal replacement therapy in 10 cases (15.20% of the total of all cases, while among those with acute dysfunction corresponded to 25.64%). Mechanical ventilation was needed in 27 patients (40.90%), of whom 4 managed to survive (6.06% of the total and 22.22% of those that required ventilation).
The symptoms most associated were: fever in 50 patients (75.80%), dyspnea in 47 (71.20%), cough in 44 (66.70%), the rest of the associated signs and symptoms in the transplants are seen in Table 3.
Table 3. Signs and symptoms associated to infection by COVID-19 in transplant patients
| |
Total (66 px) |
Returned home (39 px) |
Died (27 px) |
|
Variable |
Frequency |
% |
Frequency |
Frequency |
p (*) |
Fever |
50 |
75.8 |
28 |
22 |
0.367 |
Dyspnea |
47 |
71.2 |
23 |
24 |
0.008 |
Cough |
44 |
66.7 |
25 |
19 |
0.595 |
Arthralgias |
28 |
42.4 |
16 |
12 |
0.782 |
Myalgias |
27 |
40.9 |
16 |
11 |
0.982 |
Headache |
23 |
34.8 |
10 |
13 |
0.059 |
Diarrhea |
15 |
22.7 |
8 |
7 |
0.266 |
Odynophagia |
13 |
19.7 |
5 |
8 |
0.091 |
Thorax pain |
9 |
13.6 |
4 |
5 |
0.336 |
Conjuntivitis |
4 |
6.1 |
2 |
2 |
0.703 |
Dysuria |
4 |
6.1 |
2 |
2 |
0.703 |
Nausea |
4 |
6.1 |
1 |
3 |
0.152 |
Vomit |
4 |
6.1 |
1 |
3 |
0.152 |
Abdominal pain |
3 |
4.3 |
2 |
1 |
0.702 |
Rhinorrhea |
2 |
3.0 |
0 |
2 |
0.084 |
(*): expressed in chi squared; COVID-19: coronavirus disease; px: patients |
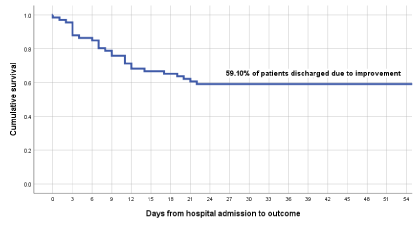
Survival analysis by Kaplan-Meier was 59.10% that were observed for up to 52 days, longer stay in one of the patients; of the deaths presented from the day of entry, the first of them was 3 hours after entry, and from there until day 22 of the hospital stay as the patient with the most time with hospital stay before dying (Figure 1).
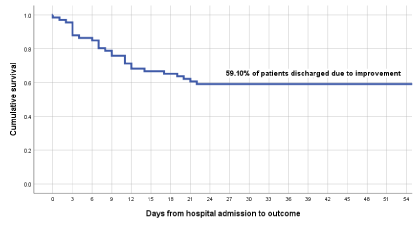
Figure 1. Survival of kidney transplant patients with moderate and severe COVID-19
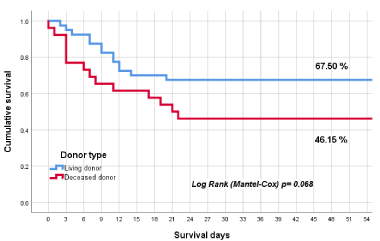
In the difference in survival by type of donor, a difference was found, with 67.50% for patients that received renal graft from a living donor against 46.16% of those from a deceased donor, although without statistically significant evidence, with a Log Rank (Mantel-Cox) of 0.068 (Figure 2).
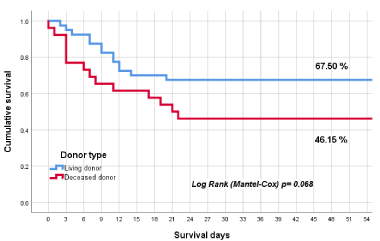
Figure 2. Survival of the kidney transplant patient with COVID-19, in relation to the type of donor
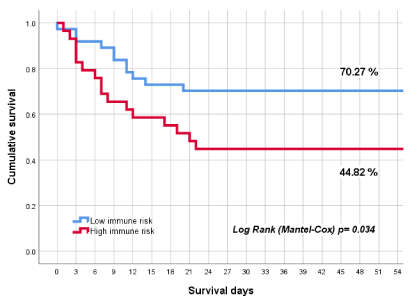
There was also a difference regarding immunological classification as low or high risk, where the difference in survival was observed with 70.27% for those classified as low immunological risk against 44.82% of those with high risk, with a statistically significant difference in a Log Rank (Mantel-Cox) of 0.034 (Figure 3).
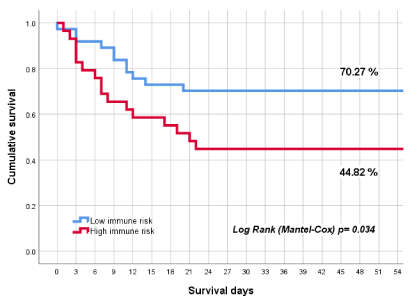
Figure 3. Survival of the kidney transplant patients with COVID-19, in relation to immunological risk
Data was collected for 66 renal transplant patients in Mexico infected with SARS-CoV-2 diagnosed as moderate or severe from the start of the pandemic to September 28, 2020, one of the largest studies reported in this group of patients in the world (66 patients).
In Mexico, a register was begun through the Centro Nacional de Transplants (CENATRA, National Transplant Center) of all transplant patients infected with coronavirus, so that by September 28, 170 persons were confirmed, of whom 46 had died (27.05%), [15-16] the difference with our cohort being that we only included moderate and severe cases, excluding asymptomatic and mild cases managed as outpatients; making only 4 units of renal transplant, where we could observe a mortality of 40.9%; representing a difference of 13.85% among the moderate and severe cases in out series. Of all the patients in Mexico by CENATRA, [15-16] 29 patients were handled as outpatients (17.05%).
There are few studies that speak of the lethalness of infection with SARS-CoV-2 in the transplanted patient. Demir, et al. [17] studied 40 receptors of renal transplant with moderate (33 cases) and severe (7 cases) pneumonia, study highly comparative to ours, with a mean age of 44.9 years (our mean was 5.4 years younger); they had a distribution by gender of 50% each, while our study included more males with 62.1% of cases (41/66). Hypertension was the most common comorbidity in both (65% for the study by Demir and 77.3% in ours), followed for them by cardiac and pulmonary disease, where there was a difference in our Mexican population, where it was diabetes and obesity, with 27.3 and 24.2, respectively, diseases that greatly contribute to mortality in our patients, even though the difference between patients that survived against those that died was significant for hypertension, with a tendency towards significance in the variable of obesity, since the mortality in the Demir study was 12.5% vs 40.9% in our population. It is important to mention that Mexico is among the first places in incidence and prevalence of these three comorbidities, which outside the context of immunosuppression (in this case, renal transplant), are the 3 comorbidities related with death in patients with COVID-19 in the world, so they are independent factors that increase the risk of death, as also observed in our study.
There was an important relation between patients with severe pneumonia and the use of polyclonal drugs [17] used in patients with habitual high immunological risk, although the outcome was different as in our case we could observe a condition similar to the relation with the type of induction (for low and high immunological risk), which in the case of the present study was related with survival, finding in the Kaplan-Meier curves of mortality only 29.73% for those receptors categorized as low immunological risk against 55.18% for those categorized as high immunological risk.
Symptoms also had peculiarities and differences, where in some studies [17] cough was the main symptom (75%), followed by fever (62.5%), dyspnea (52.5%), and diarrhea (25%), unlike the present where the four main ones were fever (75.8%), dyspnea in 71.2% of the cases, cough in 66.7% and arthralgias as the fourth symptom in 42.4%, while diarrhea was located as the seventh symptom in decreasing order, with 22.7%.
Demir also evaluated creatinine upon entry, with very similar measurements; in the case of theirs it was 1.6 (IQR 1.2-2.2), and ours showed a mean of 1.67, with the difference lying in the broader interquartile range of 1.11 to 3.57, possibly reflecting the difference in graft dysfunction, where there was a difference of 24.1%, due to the fact that their study showed an alteration in renal graft functionality of 35% contra 59.1% in the present study. Finally, there were also differences observed between patients that requires ventilation, with 25% in the case of Demir [17] compared with the present study with 40.9% requiring mechanical ventilation, condition of severity in which only 4 of 27 patients survived.
Early mortality in receptors of renal transplant is very variable, with ranges from 6% up to 25% [17-21] in various studies, unnerving against the fact that in our patients it was 40.9%, stressing that in the present study this mortality was only in moderate and severe patients; however, the national statistics in Mexico [15-16] show the data of death associated with infection by SARS-CoV-2 in 27.05%, similar to the figures in these references, possibly explained by the comorbidities peculiar to Mexico, with greater incidence and prevalence of diabetes, obesity and hypertension.
Global survival was 59.10 %, with comorbidities such as hypertension, diabetes mellitus and obesity; association with immunosuppression influenced mortality in transplanted renal patients; immunological risk presented an important factor in patient survival with 70.25% survival in those with low immunological risk and 44.82% for those with high risk. The type of donor had a difference of proportions, considering 67.50% vs 46.15% between living and deceased donors, respectively, although that may be due to the small sample size.
Authors thank the renal transplant units, all the staff and personnel related with health care that were and are on the front against this pandemic in Mexico and the world.
The authors state no conflicts of interest.
By being an observational study, there is no mention of the impact of treatment offered the patients.
- Chenna A, Konala V, Gayam V, et al. (May 09, 2020) Coronavirus Disease 2019 (COVID-19) in a Renal Transplant Patient. Cureus 12: e8038. [Crossref]
- Fishman JA, Grossi PA (2020) Novel coronavius-19 (COVID-19) in the immunocompromised transplant recipient: #flatteningthecurve. Am J Transplant 20: 1765-1767. [Crossref]
- Abolghasemi S, Mardani M, Sali S, Honarvar N, aziboroun M, et al. (2020) COVID-19 and kidney transplant recipients, Transpl Infect Dis pp: e13413. [Crossref]
- Liang W, Guan W, Chen R, Wang W, Li J, et al. (2020) Cancer patients in SARSCoV-2 infection: a nationwide analysis in China. Lancet Oncol 21: 335-337. [Crossref]
- James M, Marguerite L, Tomasz Z, James B (2020) Pharmacologic treatments for coronavirus disease 2019 (COVID-19). JAMA 323: 1824-1836. [Crossref]
- Meena P, Bhargava V, Singh D (2020) COVID-19 and the kidney: A matter of concern. Current Medicine Research and Practice 10: 4.
- Coates P, Wong G, Druele T, Rovin B, Ronco P, et al. (2020) Early experience with COVID-19 in kidney transplantation. Kidney Int 97: 1074-1075. [Crossref]
- Banerjee D, Popoola J, Shah S, Ster IC, Quan V, et al. (2020) COVID-19 infection in kidney transplant recipients. Kidney Int 97: 1076-1082. [Crossref]
- Kumar D, Tellier R, Draker R, Levy G, Humar A, et al (2003) Severe Acute Respiratory Syndrome (SARS) in a liver transplant recipient and guidelines for donor SARS screening. Am J Transplant 3: 977-981. [Crossref]
- Zhu L, Xu X, Ma K, Yang J, Guan H, et al. (2020) Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant 20: 1859-1863. [Crossref]
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395: 1054-1062. [Crossref]
- Zhu L, Xu X, Ma K, Yang J, Guan H, et al. (2020) Successful recovery of COVID-19 pneumonia in a renal transplant recipient with longterm immunosuppression. Am J Transplant 20: 1859-1863. [Crossref]
- Maggiore U, Abramowicz D, Crespo M, Mariat C, Mjoen G, et al. (2020) How should I manage immunosuppression in a kidney transplant patient with COVID-19? An ERA-EDTA DESCARTES expert opinion. Nephrol Dial Transplant 35: 899-904 [Crossref]
- Akalin E, Azzi Y, Bartash R, Seethamraju H, Parides M, et al. (2020) Covid-19 and kidney transplantation. N Engl J Med 382: 2475-2477. [Crossref]
- https://www.gob.mx/cms/uploads/attachment/file/581111/Tabla_casos_COVID-19_280920.pdf
- https://www.gob.mx/cms/uploads/attachment/file/581108/Bolet_n_Informativo_Especial_28-09-20.pdf
- Demir E, Uyar M, Parmaksiz E, Sinangil A, Yelken B, et al. (2020) COVID-19 in kidney transplant recipients: A multicenter experience in Istanbul. Transpl Infect Dis 13: e13371. [Crossref]
- The Columbia University Kidney Transplant Program (2020) Early Description of Coronavirus 2019 Disease in Kidney Transplant Recipients in New York. J Am Soc Nephrol 31: 1150-1156. [Crossref]
- Alberici F, Delbarba E, Manenti C, Econimo L, Valerio F, et al. (2020) A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int 97: 1083-1088. [Crossref]
- Montagud-Marrahi E, Cofan F, Torregrosa JV (2020) Preliminary data on outcomes of SARS-CoV-2 infection in a Spanish single center cohort of kidney recipients. Am J Transplant 20: 2958-2959. [Crossref]
- Johnson KM, Belfer JJ, Peterson GR, Boelkins MR, Dumkow LE (2020) Managing COVID-19 in Renal Transplant Recipients: A Review of Recent Literature and Case Supporting Corticosteroid-sparing Immunosuppression. Pharmacotherapy 40: 517-524. [Crossref]
Editorial Information
Editor-in-Chief
Dr. Abdullah H. A. Almalki
Section Head of Nephrology, Department of Medicine, KAMC, Saudi Arabia
Article Type
Research Article
Publication history
Received date: November 04, 2020
Accepted date: November 23, 2020
Published date: November 26, 2020
Copyright
©2020 Pérez RE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Pérez RE, Arce AMT, Meléndez AR, Caballero MS, Santiago JC, et al. (2020) Survival of transplanted patients infected with moderate and severe COVID-19 in Mexico. Trends in Transplant 14(1): DOI: 10.15761/TiT.1000286