Introduction: During the odontogenesis, structure abnormalities could occur within dental hard tissues. These primary or aqcuired structural malformations bring major therapeutic challenges, notably while performing adhesive dentistry.
Aim: Through the present systematic review, we intent to assess the adhesive interface, between abnormal dental structure and restoration materials, in order to identify the techniques that can improve its quality.
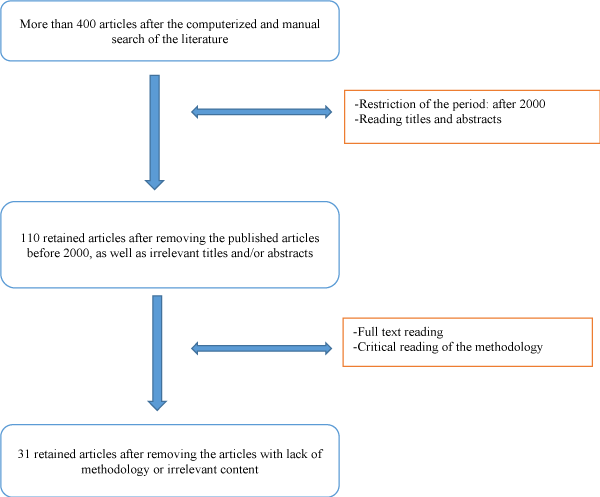
Methods: The systematic search was undergone in three electronic databases : PubMed, ScienceDirect and Google Scholar, using the following key words: teeth abnormalities, Dental enamel, Enamel defect, fluorosis, amelogenesis imperfecta, Acid etching, Bonding, ultrastructure. A manual search was performed based on the electronic search bilbiography. Published articles, after 2000, were identified by reading titles and abstracts. Their critical analysis was done based on the reading grid (Audet N. Ledère H, Pédagogie médicale) and the literature analysis guide (approved by the Agence Nationale d’accréditation et d’évaluation en santé ANAES/HAS).
Results: Among the 400 articles initially found, 110 were selected and 31 english articles were retained, after full reading. Prospective studies and systematic reviews have been conducted on four structural anomalies : amelogenesis imperfecta, fluorosis, Molar Incisor Hypomineralization and dentinogenesis imperfecta.
Discussion: According to the found data, and in comparison with healthy dental tissues, lower adhesive bonding of filling materials have been noticed, on teeth with structural abnormalities. To overcome this problem, various techniques have been suggested, such as the deproteinization using the sodium hypochlorite solution, the micro abrasion, the prolonged etching, or the use of adhesion promoters.
Conclusion: The quality of adhesive bonding to enamel and dentine is decreased in case of sutructural abnormalities, which is a real clinical challenge in dental practice. Phosphoric acid etching, without prolonged application, is recommended for damaged teeth with amelogenesis imperfecta. In the case of fluorosis, micro abrasion treatment, as well as prolonged etching, have been proven useful to the bonding protocol.
More clinical trials with long term follow-up are required, in order to improve the adhesion quality in presence of the several structural abnormalities.
teeth abnormalities, dental enamel, enamel defect, fluorosis, amelogenesis imperfecta, acid etching, bonding, ultrastructure
Patients aesthetic needs have increased in the era of minimally invasive and conservative dentistry. Consequently, the bonding process has become an essential procedure in dental practice, and a main focus for constant materials evolution. Respecting healthy dental structure, the adhesive bonding principles are currently well known : with regard to the healthy enamel, we obtain the classic facies, enabling the resin macro mechanical anchoring. Concerning the dentin surface, the mechanism remains more complex because of its intrinsic humidity. The acid etching removes the main smear layer and deminerlises the dentinal tubules. The collagen network becomes exposed and forms the hybrid layer, after adhesive resin infiltration.
In the presence of dental structural abnormalities, the enamel and/or the dentin composition and structure change. Thus, the bonding adhesive techniques become challenging. The literature reports a failure rate of 43% of the restorations designed on dental compromised structures.
In view of this significant low longevity, the issue that arises is: to what extent the compromised dental surface is able to provide a sufficient connection with the bonding materials (composites or ceramic).
The purpose of this article is to assess the adhesion quality on damaged structural teeth, and to identify the recommended techniques for their optimal bonding.
A literature computerized search was conducted in PubMed, Science Direct and Google Scholar, using the key words with the following boolean equations : bonding AND teeth abnormalities ; acid etching dental / method; dental enamel ultrastructure AND dental bonding ; enamel defect / dental bonding; amelogenesis imperfecta / therapy ; dental bonding / methods AND fluorosis ; dental bonding / methods AND amelogenesis imperfecta.
This work was limited to published articles after 2000 ; namely clinical studies, clinical trials and literature reviews. The case reports, experts opinion and studies with lack of methodology were excluded. A manual investigation was done using a bottom-up research, and based on the references previously identified in the bibliography.
Titles and abstracts reading followed by full reading did allow to retain the articles that meet the inclusion criteria cited above.
The articles critical analysis was undergone based on the reading grid (Audet N. Ledère H, Pédagogie médicale), and the literature analysis guide (approved by the Agence Nationale d’accréditation et d’évaluation en santé ANAES/HAS).
Among the 400 collected articles in the literaure search, 110 were identified after title and abstract reading. The full reading has allowed us to retain 31 articles, that meet the above named inlcusion criteria (Figure 1).
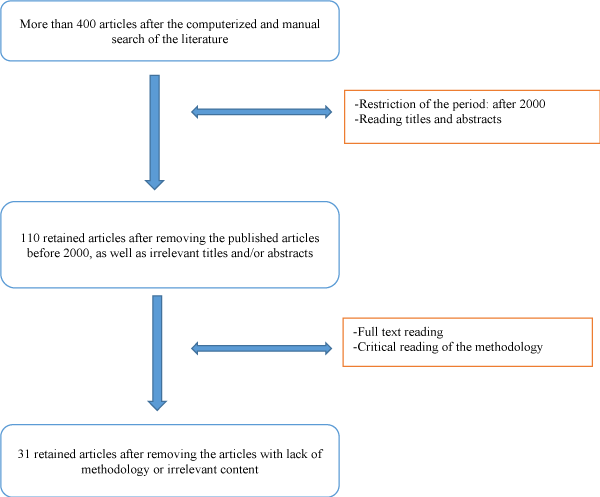
Figure 1. Flow Diagram.
The 31 retained references are anglophone, including prospective, retrospective and descriptive studies, randomized clinical trials, cohort studies, and literature reviews. All of them treating the adhesive bonding on four abnormalities : amelogenesis imperfecta (Table 1), fluorosis (Table 2), Molar Incisor Hypomineralisation (Table 3), and dentinogenesis imperfecta (Table 4).
Amelogenesis Imperfecta (AI)
The amelogenesis imperfecta (AI) is an inherited disorder related to enamel formation. Four main types can be identified : hypoplastic, hypomature, hypomineralized, and hypomature or hypoplastic associated with taurodontism. The structure alterations found within this abnormality may modify the enamel and dentin adhesiveness values [1,2].
The healthy enamel adhesiveness value is higher than the damaged enamel with an AI. The studies have shown that the three classic etching facies present on a healthy enamel are found within the hypomineralized and hypomature AI, even though these two are characterized with a defective mineralization. Consequently, their etching with 35% phosphoric acid is kept optimal.
Nevertheless, in the case of hypoplasia, the etching quality depends on the clinical form. The bonding remains suitable within pitted hypoplasia cases, but may be affected in other clinical forms (X-linked hypoplasia, smooth hypoplastic AI) [3-7].
The dentin adhesiveness value, in the case of AI, is lower than a normal dentin. It may be due to the structure similarity between an affected dentin with AI and sclerotic dentin. This last one has a lower bondability than a healthy dentin [8-10]. However, the bonding strength to the damaged dentin remains significantly higher than the damaged enamel [1,3].
In 2011, Pugach and co-workers have compared the adhesive systems effectiveness ; on damaged teeth with hypoplastic and hypomature AI. Higher adhesiveness values have been found with self-etching systems as compared to etch-and-rinse systems [11]. This can be explained by loosing the remaining enamel, leaving the dentin surface partly exposed by the etching, which allows the self-etching to be more efficient.
By contrast, Yaman and al, in 2014 didn’t found any significant difference between the two adhesive systems [12].
The lack of a standardized protocol within the two studies (the use of the same adhesive system, the sample size…) precludes a definitive conclusion.
To ensure a better adhesion, the researchers have conducted their studies following different chemical pathways:
The effect of prolonged etching was assessed by Hirasihi and al in 2008. They have demonstrated that doubling the acid etching time, from 15 to 30 seconds, reverses the adhesion values within a healthy dentin. Yet, it has no significant impact on a damaged dentin with AI [9].
The enamel deproteinization with sodium hypochlorite solution was suggested as an adhesion optimization strategy, by extruding the organic elements in the enamel structure, before the acid etching. This pretreatment has shown promising results, as it doubled the enamel etched surface from 48.8% to 94.47%, for Saroglu team in 2006 [5]. But, it has not been proven efficient among the adhesiveness values studies, neither before nor after the etching [3,13,14].
The conflicting findings drive to more studies, using the same protocol, before adopting the deproteinization as a therapeutical approach in the clinical practice.
Fluorosis
Dental fluorosis is a dental dysplasia due to a chronic ingestion of fluoride. It usually occurs on permanent teeth, and comes in the form of hypomineralization of the external enamel surface [15,16]. The management of these lesions takes place in the therapeutic gradient concept, from the less invasive techniques to the most invasive protocols. These last ones will be performed in moderate to severe cases, such as directe adhesive technique, or setting up a covering cosmetic element, namely a veneer or a ceramic crown. All these techniques will invovle a bonding procedure, where the adhesiveness value may be influenced by the presence of the abnormality.
The adhesion to the damaged enamel is lower than to the healthy one no matter how severe the fluorosis is [15-19]. The well-known performance of etch-and-rinse systems on normal enamel is also proven, regarding the fluorotic enamel, and remains significantly higher than the self-etching systems outcome [17,20,21].
The adhesion to flurotic dentin is under-investigated. In 2007, Waidyasekra’s team has confirmed the low adhesion to the damaged dentin. It has also demonstrated, unlike the enamel, that the adhesiveness value is influenced by the severity of the fluorosis ; the more severe the fluorosis, the lower the adhesiveness [22].
However, Ermis and co-workers, in 2003, have recorded that the difference between the healthy dentin adhesion and the damaged dentin adhesion is not significant, when it comes to the moderate forms. The adhesiveness values, on fluorotic dentin, obtained by the self-etching systems are higher than those given by the etch-and-rinse systems [23].
Two different approaches are used, in order to improve the adhesion to fluorotic damaged tooth :
Chemical approach : A marked adhesion improvement, to the moderate fluorotic enamel, has been demonstrated after increasing the etching time to 60 seconds, 90 seconds, and even 120 seconds [15,16]. To extend the primer application time is not a practicable treatment, as it doesn’t have a significant impact on the fluorotic enamel adhesion [24]. The application of 37% phosphoric acid, before using self-etching systems, improves significantly the enamel adhesion.
Micro-abrasion mechanical approach : Ermis and co-workers have shown that the adhesion is considerably improved while using a rotating instrument, to eleminate the external part of the hypermineralized enamel, to a thikness of 300µm. This finding is consistent with the studies of Jayasooriya and co-workers in 2002, and Silva and co-workers in 2013 [16,20,24].
Molar Incisor Hypomineralization
The Molar Incisor Hypomineralisation (MIH) is a qualitative defect of the enamel. Classified into mild, moderate to severe, MIH can affect one to all of the permanent molars, which is usually associated with the hypomineralization of the incisors [7,25-27].
The literature on the adhesion of teeth with MIH is still limited, compared to the one related to AI. This is due to the lack of extracted teeth that are hypomineralized and appropriate for testing in the meantime.
In 2006, William’s team has compared the adhesion of the healthy enamel with the hypomineralized one, using self-etching adhesive systems. They have found a lower adhesion within the damaged enamel, which has a porous structure with cracks, comparing to healthy enamel. The low adhesiveness is mainly related to the formation of resinous intratubular flanges. Moreover, the comparison between the various adhesive systems does not show any significant difference [28,29].
The enamel pretreatment with 5% sodium hypochlorite has been suggested, in order to improve the adhesion and remove the yellow dicsoloration. Yet, its efficiency has not been shown. The quality surface within the pretreated enamel and the control enamel were identical. There is also evidence, as it would be for healthy enamel, that applying 2% sodium fluoride for 4 minutes before the etching, has an opposite effect on the adhesion, by increasing the microleakage of the enamel-adhesive interface [30,31].
Despite the low adhesiveness recorded by the researchers, Lygdiakis and co-workers, in 2003, estimate that the long term sustainability remains satisfactory, when it comes to first hypomineralized permanent molars [32].
Dentinogenesis Imperfecta
The dentinogenesis imperfecta is a genetic condition, characterized by hypomineralized and fragile dentin. It is a qualitative defect that can be accompanied with a quantitaive defect, related to the structure of the dentin-pulp complex.
There are several articles treating the phenotypic variability of the damaged dentin, but rare are those studying its adhesion.
The bonding on these teeth seems to be less efficient than the other abnormalities. The scanning electron microscope of damaged teeth with dentinogenesis imperfecta, in Gallusi and co-workers study in 2006, has shown an abnormal hybrid layer. This outcome confirms the low adhesion quality. However, the bonding is not conraindicated.
Further sudies are needed to meet an optimal and specific adhesion technique for this kind of teeth [33,34].
The structure abnormalities interfere with the adhesive rehabilitation. The literature ressources concerning the adhesion to such substrates are limited.
The adhesiveness to damaged structure with AI is lower than the normal teeth. The use of 37% phosphoric acid remains the best method to surface treatment. The effect of its prolonged application is not proven yet. Self-etching systems performance, in comparison with etch-and-rinse systems, as well as the enamel deproteinization, require further studies, before being included in the therapeutic arsenal.
The adhesive interface quality is decreased within fluorotic enamel and fluorotic dentin. Bonding to fluorotic teeth is improved by the micro abrasion mechanical treatment ; enhancing the surface roughness, as well as the prolonged etching ; using self-etching systems associated with 37% phosphoric acid, prior etching.
The literature on MIH is limited. Neither the 5% hypochlorite sodium pretreatment, nor the application of 2% fluoride sodium gel for 4 minutes before the etching, have imporved the low damaged teeth adhesion. Yet the long-term prognosis of these teeth restorations remains satisfactory.
The adhesiveness to damaged teeth with dentinogenesis imperfecta is low, as it is impossible to find a normal hybrid layer. Nevertheless, further studies are required to develop secific techniques, ensuring optimal adhesion to the altered dental surfaces.
The authors declare that there is no conflict of interest regarding the publication of this article.
- Crawford PJ, Aldred M, Bloch-Zupan A (2007) Amelogenesis imperfecta. Orphanet J Rare Dis 2: 17. [Crossref]
- Pousette Lundgren G, Dahllöf G (2014) Outcome of restorative treatment in young patients with amelogenesis imperfecta. a cross-sectional, retrospective study. J Dent 42: 1382-1389. [Crossref]
- Faria-e-Silva AL, De Moraes RR, Menezes Mde S, Capanema RR, De Moura AS, et al. (2011) Hardness and microshear bond strength to enamel and dentin of permanent teeth with hypocalcified amelogenesis imperfecta. Int J Paediatr Dent 21: 314-320. [Crossref]
- Seow WK, Amaratunge A (1998) The effects of acid-etching on enamel from different clinical variants of amelogenesis imperfecta: an SEM study. Pediatr Dent 20: 37-42. [Crossref]
- SaroÄŸlu I, Aras S, OztaÅŸ D (2006) Effect of deproteinization on composite bond strength in hypocalcified amelogenesis imperfecta. Oral Dis 12: 305-308. [Crossref]
- Sánchez-Quevedo C, Ceballos G, Rodríguez IA, García JM, Alaminos M (2006) Acid-etching effects in hypomineralized amelogenesis imperfecta. A microscopic and microanalytical study. Med Oral Patol Oral Cir Bucal 11: E40-43. [Crossref]
- Willmott R, BRYAN AE, DUGGAL MS (2008) Molar incisor hypomineralization: a literature review
- European Archives of Paediatric Dentistry 9: 172-179. [Crossref]
- Sánchez-Quevedo MC, Ceballos G, García JM, Luna JD, Rodríguez IA, et al. (2004) Dentine structure and mineralization in hypocalcified amelogenesis imperfecta: a quantitative X-ray histochemical study. Oral Dis 10: 94-98. [Crossref]
- Hiraishi N, Yiu CK, King NM (2008) Effect of acid etching time on bond strength of an etch-and-rinse adhesive to primary tooth dentine affected by amelogenesis imperfecta. Int J Paediatr Dent 18: 224-230. [Crossref]
- Tay FR, Pashley DH (2004) Resin bonding to cervical sclerotic dentin: a review. J Dent 32: 173-196. [Crossref]
- Pugach MK, Ozer F, Li Y, Sheth K, Beasley R, et al. (2011) The use of mouse models to investigate shear bond strength in amelogenesis imperfecta. J Dent Res 90: 1352-1357. [Crossref]
- Yaman BC, Ozer F, Cabukusta CS, Eren MM, Koray F, et al. (2014) Microtensile bond strength to enamel affected by hypoplastic amelogenesis imperfecta. J Adhes Dent 16: 7-14. [Crossref]
- Sönmez IS, Aras S, Tunç ES, Küçükeşmen C (2009) Clinical success of deproteinization in hypocalcified amelogenesis imperfecta. Quintessence Int 40: 113-118. [Crossref]
- Pugach MK, Ozer F, Mulmadgi R, Li Y, Suggs C, et al. (2014) Shear bond strength of dentin and deproteinized enamel of amelogenesis imperfecta mouse incisors. Pediatr Dent 36: 130-136. [Crossref]
- Ateyah N, Akpata E (2000) Factors affecting shear bond strength of composite resin to fluorosed human enamel. Oper Dent 25: 216-222. [Crossref]
- Silva-Benítez EL, Zavala-Alonso V, Martinez-Castanon GA, Loyola-Rodriguez JP, Patiño-Marin N, et al. (2013) Shear bond strength evaluation of bonded molar tubes on fluorotic molars. Angle Orthod 83: 152-157. [Crossref]
- Ertuğrul F, Türkün M, Türkün LS, Toman M, Cal E (2009) Bond strength of different dentin bonding systems to fluorotic enamel. J Adhes Dent 11: 299-303. [Crossref]
- Shida K, Kitasako Y, Burrow MF, Tagami J (2009) Micro-shear bond strengths and etching efficacy of a two-step self-etching adhesive system to fluorosed and non-fluorosed enamel. Eur J Oral Sci 117: 182-186. [Crossref]
- Weerasinghe DS, Nikaido T, Wettasinghe KA, Abayakoon JB, Tagami J (2005) Micro-shear bond strength and morphological analysis of a self-etching primer adhesive system to fluorosed enamel. J Dent 33: 419-426. [Crossref]
- Ermis RB, De Munck J, Cardoso MV, Coutinho E, Van Landuyt KL, et al. (2007) Bonding to ground versus unground enamel in fluorosed teeth. Dent Mater 23: 1250-1255. [Crossref]
- Isci D, Sahin Saglam AM, Alkis H, Elekdag-Turk S, Turk T (2011) Effects of fluorosis on the shear bond strength of orthodontic brackets bonded with a self-etching primer. Eur J Orthod 33: 161-166. [Crossref]
- Waidyasekera PG, Nikaido T, Weerasinghe DD, Tagami J (2007) Bonding of acid-etch and self-etch adhesives to human fluorosed dentine. J Dent 35: 915-922. [Crossref]
- ErmiÅŸ RB, Gokay N (2003) Effect of fluorosis on dentine shear bond strength of a self-etching bonding system. J Oral Rehabil 30: 1090-1094. [Crossref]
- Jayasooriyap, Wettasinghe K, Ogata M, Nikaido T, Tagami J (2002) Micro-tensile bond strength of a self-etching primer bonding system to fluorosed enamel. Int Chin J Dent 2: 107-115.
- Lygidakis NA (2010) Treatment modalities in children with teeth affected by molar-incisor enamel hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent 11: 65-74. [Crossref]
- Fayle SA (2003) Molar incisor hypomineralisation: restorative management. Eur J Paediatr Dent 4: 121-126. [Crossref]
- Weerheijm KL, Jälevik B, Alaluusua S (2001) Molar-incisor hypomineralisation. Caries Res 35: 390-391. [Crossref]
- Jälevik B, Dietz W, Norén JG (2005) Scanning electron micrograph analysis of hypomineralized enamel in permanent first molars. Int J Paediatr Dent 15: 233-240. [Crossref]
- William V, Burrow MF, Palamara JE, Messer LB (2006) Microshear bond strength of resin composite to teeth affected by molar hypomineralization using 2 adhesive systems. Pediatr Dent 28: 233-241. [Crossref]
- Gandhi S, Crawford P, Shellis P (2012) The use of a 'bleach-etch-seal' deproteinization technique on MIH affected enamel. Int J Paediatr Dent 22: 427-434. [Crossref]
- Moosavi H, Ahrari F, Mohamadipour H (2013) The effect of different surface treatments of demineralised enamel on microleakage under metal orthodontic brackets. Prog Orthod 14: 2196-1042. [Crossref]
- Lygidakis NA, Chaliasou A, Siounas G (2003) Evaluation of composite restorations in hypomineralised permanent molars: a four-year clinical study. Eur J Paediatr Dent 4: 143-148. [Crossref]
- Gallusi G, Libonati A, Campanella V (2006) SEM-morphology in dentinogenesis imperfecta type II: microscopic anatomy and efficacy of a dentine bonding system. Eur J Paediatr Dent 7: 9-17. [Crossref]
- Mathu-Muju K, Wright JT (2006) Diagnosis and treatment of molar incisor hypomineralization. Compend Contin Educ Dent 27: 604-610. [Crossref]