Abstract
Objective: This study evaluates utilization trends for procedural treatment modalities for uterine fibroids including hysterectomy, myomectomy, endometrial ablation, and uterine fibroid embolization (UFE).
Study design: Data from the Merative MarketScan Commercial Claims and Encounters Databases were analyzed from 2009 to 2022 for patients who were diagnosed with uterine fibroids. Patients were Identified by ICD-9/ICD-10 codes and categorized by procedure based on CPT codes. Utilization rates were calculated per 10,000 patients with fibroid diagnoses. A repeated measure ANOVA was conducted (p < 0.0001) for each year followed by Tukey's HSD tests with Bonferonni correction.
Results: There were a total of 407,487 unique patients who had a diagnosis of uterine fibroids and had a procedure of interest between January 2009 through June 2022 in both the inpatient and outpatient settings before applying exclusion factors. Querying patients with an ICD9/10 code of symptomatic fibroids, there was an average of 27,278 patients who carried a fibroid diagnosis per month. The study cohort consisted of 407,487 unique patients with a mean patient age of 44.93 (±7.13) who underwent a total of 494,108 procedures. Hysterectomy had the highest utilization rate overall followed by endometrial ablation, myomectomy, then UFE. From 2009 through 2020, yearly post-hoc Tukey's HSD tests consistently revealed significant differences in utilization rates when com paring hysterectomy against endometrial ablation, myomectomy, and UFE. In order of most to least number of procedures performed, hysterectomy was first, which accounted for 367,914 procedures, followed by endometrial ablation (n=45,634), myomectomy (n=56,816), and uterine fibroid embolization (n=23,744). During the study period, there was a steady increase utilization in hysterectomy (R=0.63, R2=0.4) and of life as the hysterectomy patient myomectomy (R=0.47, R2=0.22). There was no significant trend in the utilization rates of UFE, and endometrial ablation shows a moderately negative association (R=0.59, R2=0. 35).
Conclusion: The study highlights the relative prevalence of hysterectomy as the prominent non-women with symptomatic fibroids may pharmacological treatment for fibroids. UFE, a less invasive option is less utilized, suggesting a gap in patient and/or provider education.
Keywords
uterine fibroids, uterine fibroid embolization, hysterectomy, myomectomy, endometrial ablation, MarketScan database
Introduction
Background and rationale
Uterine fibroids are a common gynecological tumor that affects up to 80% of reproductive age females. While most remain asymptomatic, the influence of hormonal fluctuations of estrogen and progesterone play a role in affecting size [1]. Approximately 30% of women experience symptoms, such as abdominal pain and pressure, heavy or prolonged menstrual bleeding, or reproductive dysfunction, which may alter a patient's quality of life and prompt treatment [2].
Current treatment options for uterine fibroids range from conservative medical to surgical or interventional options. Due to their low cost and widespread availability, NSAIDs remain the first line pharmacological management and are largely used to minimize pain [3]. Other medications are more effective for reducing bleeding and shrinking the size of fibroids, including tranexamic acid, combined estrogen-progestin hormonal contraceptives, progestins, aromatase inhibitors, and GnRH analogs, which may be used alone or in combination (i.e Myfembreeo®) [4]. Medical therapies, however, may be insufficient to alleviate all symptoms and can cause adverse effects when used long-term or result in rebounding symptoms if discontinued. There are a variety of invasive options including myomectomy, uterine fibroid embolization (UFE), magnetic resonance-guided focused ultrasound surgery (MRgFUS), ultrasound-guided radiofrequency ablation (RFA), endometrial ablation, and hysterectomy [2].
Among all treatment options, definitive treatment can onIy be achieved via hysterectomy. However, a hysterectomy may not be in line with a patient's future fertility goals or their wish to retain their uterus. While myomectomy is a uterus-sparing procedure, several reports have noted fibroid recurrence rates ranging from 10-27% [5-10]. Alternatively, minimally-invasive treatments (i.e U FE, MRgFUS, RFA, endometrial ablation) remain as effective options for patients who decline surgery or are poor surgical candidates. According to the FEMME trial, no significant difference in post-operative pregnancy rates or bleeding reduction were found between myomectomy and UFE [11], whereas the latter was found to be more expensive [12]. However, with the added benefit of shorter hospital stay, fewer complications, and faster recovery with UFE, the procedure may be the better option in lower resource settings [13,14]. Results from the EMMY trial showed that with achieving similar improvements in quality of life, 65% of patients who underwent UFE did not require secondary hysterectomy. Like UFE, endometrial ablation offers similar improvement to quality of life, lower costs, and deferral of hysterectomy.
Objectives
While the current recommendations and guidelines have been adjusted in concordance with the results of the aforementioned studies, data regarding the prevalence of treatment modalities utilized to treat fibroids is still lacking. Thus, the aim of this study is to evaluate the trends in the utilization of invasive fibroid treatment modalities and compare it to the utilization of UFE.
Materials and methods
Study design and selling
A retrospective cohort study was performed using the MerativeTM MarketScan Commercial Claims and Encounters Database (Merative, Ann Arbor, MI, USA), which was licensed by and accessed via our institution for data collection and analysis. This database contains insurance claims and cost information from a range of employer-sponsred insurance providers across the US. Inpatient and outpatient data between January 2009 through June 2022 were queried for this study (Table 1 and 2). This study was exempt from further review by our Institutional Review Board as MarketScan’s data is completely de-identified.
Participants and study size
The Ninth and Tenth Revisions of International Classification of Diseases (ICD -9/10) and Current Procedural Terminology (CPT) coding systems were used to find patients with a fibroid diagnosis and identify the corresponding treatment procedure. Patients were then excluded from the cohort if there was no information related to their unique enrollee ID and service date. To filter out duplicate entries, patient encounters with the same enrollee ID, service date, and procedure CPT code were filtered out, meaning that only the first unique patient encounter was included. Patients were subsequently filtered and grouped by uterine fibroid treatment modality (myomectomy, hysterectomy, endometrial ablation, or UFE) using the corresponding CPT codes (Table 2, Figure 1). Being a retros pective cohort study, sample size was not pre-determined and was a result of the described data extracti on process and application of exclusion criteria.
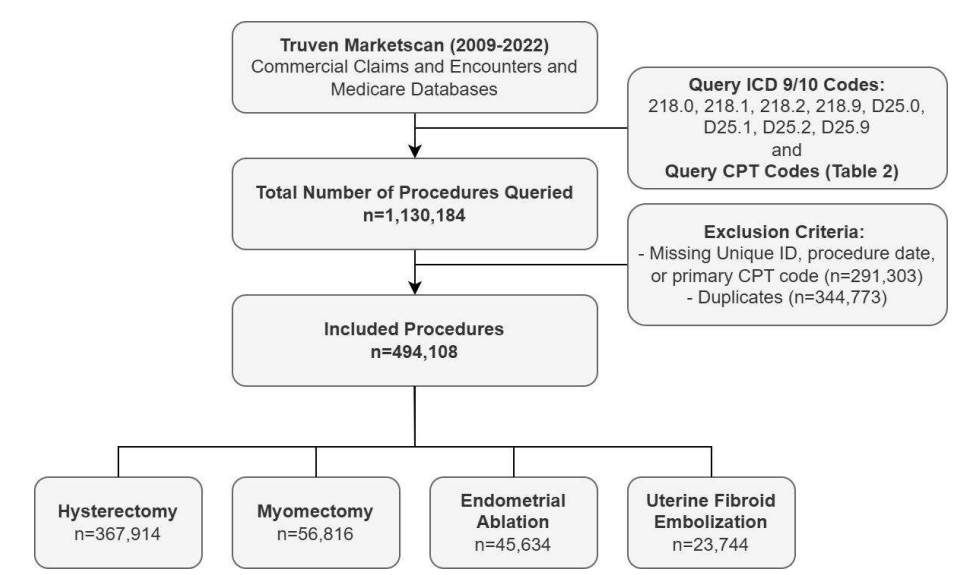
Figure 1. MarketScan database extraction including the exclusion criteria at each study point
Bias
Using claims-based data introduces selection bias to the study; however, robust inclusion and exclusion criteria allowed for a relevant cohort to answer the objectives. All information i n the database is deidentified. Statistical analyses were planned prior to data collection, preventing selective reporting.
Data sources/measurement and variables
Diagnosis and procedure information were available in both the inpatient and outpatient data tables in the MarketScan database. The number of procedural encounters within the year was divided by the number of patients who carried a diagnostic code of fibroids for that year. Measurements of monthly utilization rates were based on observation counts found by CPT codes. To calculate the utilization rate, the number of procedures per month was divided by the number of patients with fibroid diagnosis per month and later multiplied by 10,000.
Statistical methods
This study utilized a complete case analysis. Descriptive statistics were conducted, which included number counts for categorical variables and the medians and means for continuo us variables. To evaluate differences in treatment modality, an analysis of variance (ANOVA) was conducted. Repeated measures ANOVA was chosen over one-way ANOVA, which relies on independent variables, due to the correlation between observations. Normality of the data was tested by visualizing quantile-quantile (Q-Q) plots and performing a Shapiro-Wilkstest each year using the calculated monthly utilization rates. Q-Q plots were also visualized for each procedure over the entire study period. Post-hoc Tukey's honest significant difference (HSD) tests were performed to compare specific procedures' utilization rates each month during the study period. Alpha values were adjusted through a Bonferroni correction. All analyses were performed with Python using JupyterLab, version 4.0.6 (Project Jupyter, New York, New York).
Results
Descriptive data: Uterine fibroid prevalence
There were a total of 407,486 unique patients who had a diagnosis of uterine fibroid and had a procedure of interest between January 2009 through June 2022 in both the inpatient and outpatient settings before applying exclusion factors and who underwent a total of 494,108 procedures. Querying patients with an ICD9/10 code of symptomatic fibroids, there was an average of 27,278 patients who carried a fibroid diagnosis per month. However, approximately halfway through 2015 there was a change in the number of fibroid diagnoses. The average number of patients with a fibroid diagnosis from January 2009 to December 2014 was 37,798 while from January 2015 until June 2022, the average monthly number of fibroid diagnoses was 18,862, most likely due to the changes in ICD coding that occurred in 2015.
Descriptive data: Characteristics of fibroid treatment modalities
The average age with respective standard deviations of patients with hysterectomy, myomectomy, endometrial ablation, and UFE was 46.05 (±6.75), 37.95 (±7.24), 45.01 (±5.53), 44.11 (±5.48), respectively, with the mean age of the study cohort being 44.93 (±7.13) as summarized in Table 3. There were varying amounts of males assigned at birth in our study with our definition of male as “sex assigned at birth. The procedures with the highest percentage of males are hysterectomy, with a total of 319 male patients. Males assigned at birth represented 0.08% of the total study population across all treatment modalities.
Outcome data and main results: Frequency of symptomatic fibroid treatment procedures
Between January 2009 to June 2022, a total of 407,486 unique treatment was performed for the treatment of symptomatic fibroids across the modalities of hysterectomy, myomectomy, endometrial ablation, and uterine fibroid embolization, resulting in an overall utilization rate of approximately 1253 procedures per every 10,000 patients per month with a fibroid diagnosis on Marketscan with the assumption that being symptomatic comes with the receipt of a procedure. Due to the changes in sample size per year in the MarketScan database, utilization rates were calculated as the number of procedures per every patient who carried a fibroid diagnosis in a given month, including patients who were not treated with a procedure. Of the four modalities, hysterectomy was the most common with utilization rate of 952 procedures per every 10,000 patients with a fibroid diagnosis while myomectomy was the second most performed with a utilization rate of 140 procedures per 10,000 patients per month. Endometrial ablation followed with a utilization rate of 104 procedures per 10,000 patients with a fibroid diagnosis. UFE was performed the least, accounting for a utilization rate of 57 procedures per 10,000 patients with a fibroid diagnosis. In order of most to least number of procedures performed, hysterectomy was first, which accounted for 367,914 procedures, followed by endometrial ablation (n=45,634), myomectomy (n=56,816), and uterine fibroid embolization (n=23,744). Over the course of the study period, there was a steady increase utilization in hysterectomy (R=0.63, R2=0.4) and myomectomy (R=0.47, R2=0.22). There was no significant trend in the utilization rates of UFE, and endometrial ablation shows a moderately negative association (R=0.59, R2=0.35). Figure 2 demonstrates the different trends in utilization rates for each treatment modality.
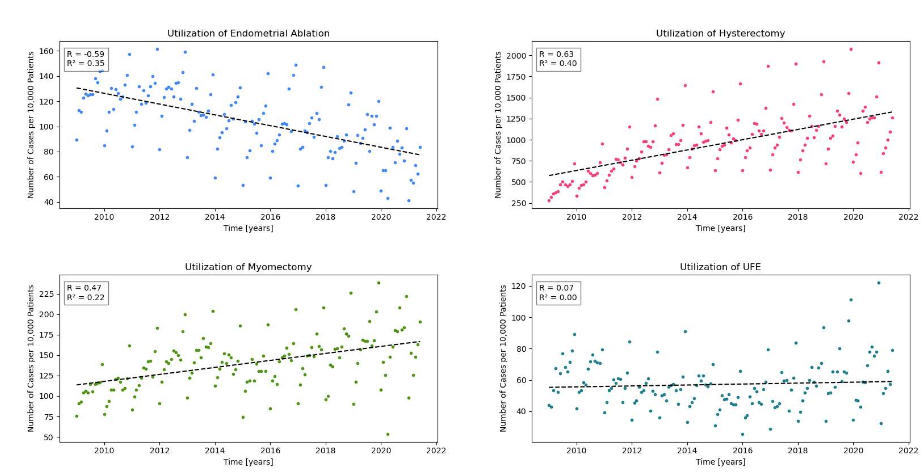
Figure 2. Utilization of each treatment modality had variable associations across time with hysterectomy as the strongest positive correlation
Main results: Differences in treatment modality utilization
To evaluate differences in utilization rates across treatment modalities, a repeated measure ANOVA was conducted for each year. The assumption of normality was satisfied after visualizing Q-Q plots and performing Shapiro-Wilks tests. ANOVA demonstrated a significant difference among the treatment modalities over the study period (p<0.0001). From 2009 through 2020, yearly post-hoc Tukey’s HSD tests consistently revealed significant differences in utilization rates when comparing hysterectomy with the other three procedures. Overall, hysterectomy was consistently the highest utilized procedure throughout the study period with the strongest positive correlation over time, followed by myomectomy. UFE demonstrated no correlation with respect to utilization rates over time, suggesting that its usage has not changed drastically over the study period (Figure 3 and 4).
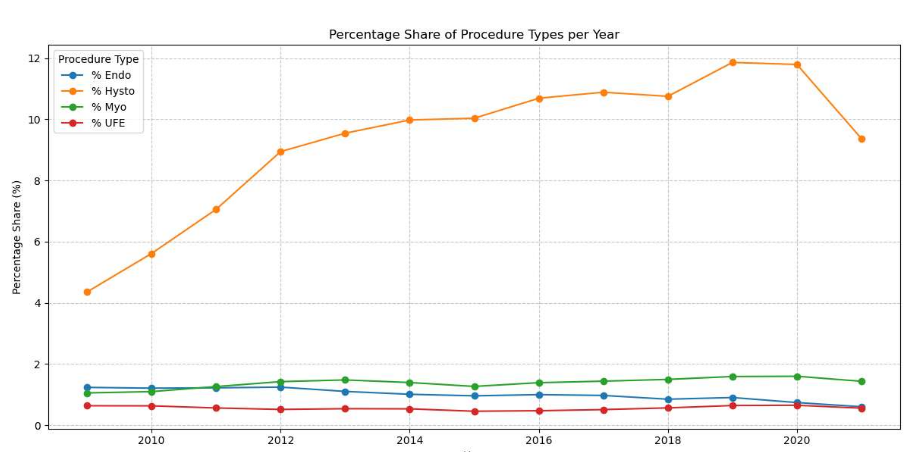
Figure 3. Percentage share represents the number of patients undergoing a specific treatment modality divided by the number of patients undergoing a procedure per month and then averaged per year

Figure 4. Procedure usage per year
Discussion
Generalizability
Due to the large sample size of our cohort, one strength of the study is the ability to approximate trends in the utilization of various treatment modalities for symptomatic fibroids with increased statistical power. In addition, a large variety of insurance companies are represented within the database.
Key results
Throughout the duration of our study, we saw a relative increase both hysterectomies and myomectomies, most likely due to increased diagnostic capabilities and detection of fibroids over time. Hysterectomy remains the most utilized procedure, which may be attributed to several factors, including patient preference for a definitive cure, a perceived lack of effective non-surgical or minimally invasive options, and a shift in the approach of Obstetricians and Gynecologists (OBGYN) towards more definitive interventions. There were also a notable number of male patients who received a hysterectomy, most likely to receive gender-affirming care.
Implications for practice and/or policy
Changes in guidelines have had a significant impact on utilization of techniques like UFE. For instance, landmark trials in the interventional radiology literature such as the EMMY trial have highlighted the safety and efficacy of UFE in the treatment of symptomatic fibroids. These landmark studies have shown that UFE patients had less pain during their hospital stay and returned significantly sooner to work and daily activity [15]. Additionally, the 10-year follow-up studies have shown that 2/3 UFE patients were able to avoid hysterectomy while retaining the same quality of life as the hysterectomy patient cohort [16].
Patient education about UFE is critical in ensuring that women are aware of all available treatment options and can make informed decisions about their care. Many women with symptomatic fibroids may not be aware of UFE as a treatment option and may not have access to accurate information about the procedure's risks and benefits. It is critical for all healthcare providers to take an active role in explaining all available options, including UFE. Many primary care providers may not be aware of the procedure's efficacy and may be more likely to recommend traditional surgical options even if UFE could be a viable and more appropriate alternative especially for women wanting uterine-sparing treatments. In a recent study, 112 OBGYN physicians were surveyed regarding their knowledge related to safety and patient outcomes of UFE, physicians reported lower confidence in the benefits of UFE. Education initiatives aimed at healthcare providers, particularly primary care and OBGYN physicians, can help increase awareness and understanding of UFE [17-20]. These trends might be changing as UFE is now recognized in the OBGYN and ACOG literature as a viable alternative to surgical treatments for symptomatic fibroids through its inclusion in the Practice Bulletin as early in 2021 [21].
In conclusion, the trends observed in our study cohort demonstrate a potential underutilization of minimally invasive alternatives for symptomatic fibroids such as UFE. There is a need for future studies that confirm more recent trends in fibroid treatment modality utilization because of changes in OBGYN guidelines and further research may help to identify and address barriers to access and utilization of various treatment options.
Limitations
Major limitations of our study include those intrinsic to database studies, namely billing, coding, and entry errors in the cu ration of the dataset. Retrospective studies rely on the quality and availability of accurate data and also introduce selection bias given the database is claims-based and includes individuals insured by employers. In addition, also related to limitations intrinsic to database studies, over half of the initial procedures queried were not included as they were duplicates. There is no control over data collection, resulting in a lack of fibroid incidence data and the reliance on monthly prevalence in the database to estimate utilization rates. Proper incidence data would allow more precise modeling of temporal trends. Potential confounders such as age, geographic location, and insurance type were not accounted for, potentially leading to biased results and conclusions on fibroid treatment usage. As discussed, UFE is a relatively new procedure, and there is less awareness of its availability and clinical benefits among patients and referring doctors. There may also be a slight skew in hysterectomy utilization rate as the procedure is commonly used for patients wanting to receive gender-affirming care. Given the large sample size present through the MarketScan database, however, we feel as though our method for data collection results in the most accurate and powered sample size. Testing normality for each year using the Shapiro-Wilks test in all cases but for one was satisfied, suggesting overall robustness of the results.
Conclusion
The study highlights the relative prevalence of hysterectomy as the prominent non-pharmacological treatment for fibroids. Utilization rates showed that hysterectomy and myomectomy had positive trends. There is a potential underutilization of minimally invasive alternatives for symptomatic fibroids such as UFE, suggesting a gap in patient and/or provider education.
Declarations
Abbreviations: The Ninth and Tenth Revisions of International Classification of Diseases (ICD-9110); Current Procedural Terminology (CPT); uterine fibroid embolization (UFE); magnetic resonance-guided focused ultrasound surgery (MRgFUS); ultrasound-guided radiofrequency ablation (RFA); analysis of variance (ANOVA) was conducted; quantile-quantile (Q-Q); honest significant difference (HSD)
Internal review board and ethics approval: This study was exempt from IRB approval.
Ethics approval and consent to participate
Not applicable. There is no personally identifiable data including biomedical, clinical, and biometric data. There is no research involving human participants, human material, or human data. This study has been granted an exemption from requiring ethics approval. There is no relevant reference number to cite. The need for consent to participate was waived by an Institutional Review Board (IRB).
Consent for publication
Our manuscript does not include details, images, or videos relating to an individual person. All images generated are those of the authors. Consent for publication of images is not applicable here.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to it being a private use database but are available from the corresponding author on reasonable request.
Conflicts of interest
The authors have no competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Funding
Funding Supported by the American College of Radiology, Harvey L Neiman Health Policy Institute Grant, and the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002378. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author contributions
-Deepak lyer, Hanssen Li, John Moon, ZB, Janice Newsome, Zachary Bercu: The conception OR design of the work
-Jenny Nguyen, Nathan Sim, Deepak lyer, Menelaos Konstantinidi: The acquisition, analysis, OR interpretation of data
-Jenny Nguyen, Deepak lyer, Anna Hu, Nathan Sim: Have drafted the work or substantively revised it All authors reviewed the manuscript and have approved the submitted version.
Acknowledgements
We would like to express our gratitude to the Emory Interventional Radiology Department and our attending physicians for their unwavering support, guidance, and encouragement throughout this project. Their expertise and dedication were invaluable in bringing this work to fruition.
References
- Stewart EA, Cookson CL, Gandolfo RA, Schulze‐Rath R (2017) Epidemiology of uterine fibroids: A systematic review. BJOG 124: 1501-1512. [Crossref]
- Giuliani E, As‐Sanie S, Marsh EE (2020) Epidemiology and management of uterine fibroids. Int J Gynecol Obstet 149: 3-9. [Crossref]
- Sohn GS, Cho S, Kim YM, Cho CH, Kim MR, et al. (2018) Current medical treatment of uterine fibroids. Obstet Gynecol Sci 61: 192. [Crossref]
- Al-Hendy A, Lukes AS, Poindexter III AN, Venturella R, Villarroel C, et al. (2022) Long-term relugolix combination therapy for symptomatic uterine leiomyomas. Obstet Gynecol 140: 920-930. [Crossref]
- Hutchins Jr FL (1995) Abdominal myomectomy as a treatment for symptomatic uterine fibroids. Obstet Gynecol Clin North Am 22: 781-789. [Crossref]
- Kotani Y, Tobiume T, Fujishima R, Shigeta M, Takaya H, et al. (2018) Recurrence of uterine myoma after myomectomy: Open myomectomy versus laparoscopic myomectomy. J Obstet Gynaecol Res 44: 298-302. [Crossref]
- Candiani G, Fedele L, Parazzini F, Villa L (1992) Risk of recurrence after myomectomy. Obstet Gynecol Survey 47: 45-46.
- Yoo EH, Lee PI, Huh CY, Kim DH, Lee BS, et al. (2007) Predictors of leiomyoma recurrence after laparoscopic myomectomy. J Minim Invasive Gynecol 14: 690-697. [Crossref]
- Nezhat FR, Roemisch M, Nezhat CH, Seidman DS, Nezhat CR, et al. (1998) Recurrence rate after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc 5: 237-240. [Crossref]
- Fedele L, Parazzini F, Luchini L, Mezzopane R, Tozzi L, et al. (1995) Recurrence of fibroids after myomectomy: A transvaginal ultrasonographic study. Hum Reprod 10: 1795-1796. [Crossref]
- Sirkeci F, Moss J, Belli AM, McPherson K, Daniels J, et al. (2023) Effects on heavy menstrual bleeding and pregnancy of uterine artery embolization (UAE) or myomectomy for women with uterine fibroids wishing to avoid hysterectomy: The FEMME randomized controlled trial. Int J Gynecol Obstet 160: 492-501. [Crossref]
- Rana D, Wu O, Cheed V, Middleton LJ, Moss J, et al. (2021) Uterine artery embolisation or myomectomy for women with uterine fibroids wishing to avoid hysterectomy: A cost–utility analysis of the FEMME trial. BJOG 128: 1793-1802. [Crossref]
- Goodwin SC, Bradley LD, Lipman JC, Stewart EA, Nosher JL, et al. (2006) Uterine artery embolization versus myomectomy: A multicenter comparative study. Fertility and sterility 85: 14-21. [Crossref]
- MK R (2003) Abdominal myomectomy versus uterine fibroid embolization in the treatment of symptomatic uterine leiomyomas. AJR Am J Roentgenol 180: 1571-1575.
- Hehenkamp WJ, Volkers NA, Birnie E, Reekers JA, Ankum WM, et al. (2006) Pain and return to daily activities after uterine artery embolization and hysterectomy in the treatment of symptomatic uterine fibroids: Results from the randomized EMMY trial. Cardiovasc Intervent Radiol 29: 179-187. [Crossref]
- de Bruijn AM, Ankum WM, Reekers JA, Birnie E, van der Kooij SM, et al. (2016) Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 10-year outcomes from the randomized EMMY trial. Am J Obstet Gynecol 215: 745.e1-745.e12. [Crossref]
- Baerlocher MO, Asch MR, Puri G, Vellahottam A, Myers A, et al. (2007) Awareness of interventional radiology among patients referred to the interventional radiology department: A survey of patients in a large Canadian community hospital. J Vasc Interv Radiol 18: 633-637. [Crossref]
- Heister D, Jackson S, Doherty-Simor M, Newton I (2018) An evaluation of trends in patient and public awareness of IR. J Vasc Interv Radiol 29: 661-668. [Crossref]
- Rodgers B, Rodgers KA, Chick JF, Makary MS (2023) Public awareness of interventional radiology: Population-based analysis of the current state of and pathways for improvement. J Vasc Interv Radiol 34: 960-967. [Crossref]
- Kubiszewski K, Maag B, Hunsaker P, Iwai T, Lim J, et al. (2023) Investigating the underutilization of uterine fibroid embolization by surveying practice preferences of Obstetricians/Gynecologists. J Vasc Interv Radiol 34: 1430-1434. [Crossref]
- American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Gynecology (2021) Man agementof symptomatic uterine leiomyomas: ACOG practice bulletin, number 228. Obstet Gynecol 137: e100-e115.
