Abstract
Spinal Arachnoid Cyst (AC) and Primary spinal Hydatid Cyst (HC) both are considered as very rare conditions. Herein, we report a pediatric case 11-years-old female patient, who presented thoraco-radicular pain for 5-months ago associated to numbness and fatigue of the lower limbs. At admission the patient could not walk autonomously. Magnetic Resonance Imaging (MRI) of the spine revealed a cystic intra dural extra medullary lesion without enhancement, extended over 3 thoracic levels, highly compressive. Surgical extirpation of the supposed arachnoid cyst was done, but after cyst aspiration and easy dissection from the cord, the diagnosis of HC came back to our attention as the cyst wall became thick and whitish. The pathologic evaluation of the specimen was consisting with HC disease.
Keywords
arachnoid cyst; hydatid cyst; spine; intradural
Introduction
The HC is a zoonosis caused by adult or larval stages of tapeworms belonging to the genus Echinococcus granulosus [1]. HC is the most common cause of liver and lung hydatidosis. Primary spinal HC is extremely rare, usually situated in the thoracic region and generate medullary or radicular suffering [2-4]. Radiological diagnosis is mainly established by MRI. The differential diagnosis is quite difficult and the lesion can imitate different cystic lesions, like in our case the AC. It’s capital to distinguish the HC before, as its management is always surgery, and incorrect preoperative diagnosis can compromise management of these lesions or lead to complications related to cyst rupture intraoperatively.
Case report
An 11-years-girl presented with history of thoraco-intercostal radiculalgias, bilateral low limbs weakness concomitant to bladder and bowel disability. Neurological examination revealed severe paraparesis with power 3/5 in left side and 4/5 in right one, with loss of autonomic ambulation. Lower limbs tendon reflexes were exaggerated with bilateral Babinski reflexes. There was no sensory loss.
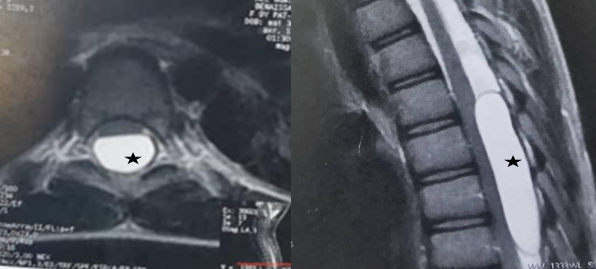
The MRI revealed an intradural extramedullary posterior cystic lesion at level of the thoracic spine, harmonious well-demarcated, that demonstrated low signal intensity on T1 and high signal intensity on T2 weighted images mimicking Cerebrospinal Fluid (CSF). The lesion appeared to be an AC (Figure 1) pushing forward the cord. There was no enhancement neither bony change.
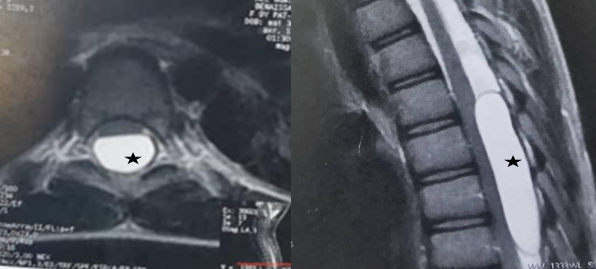
Figure 1. MRI of the thoracic spine shows a cystic lesion mimicking CSF signal (black star) compressing the spinal cord
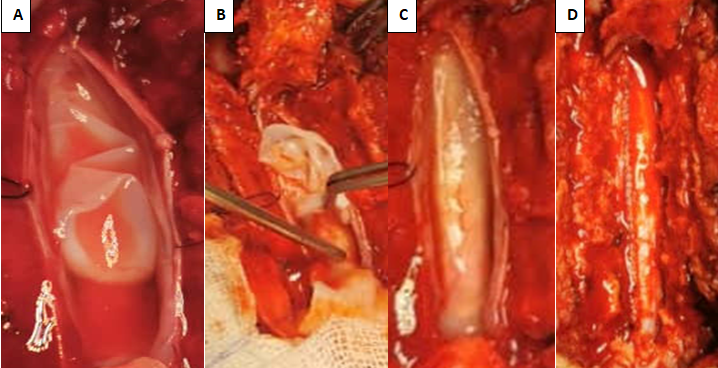
The patient underwent laminoplasty Th 4, 5 and 6 guided by fluoroscopy, the epidural space was free. After opening of the dura, a translucid cyst appeared underneath the arachnoid layer covering the posterior aspect of the cyst which is covering the cord. After peeling away the arachnoid, the 2 poles of the cyst were identified and a dissection was accomplished easily. The cyst was initially aspirated and clear fluid like CSF came out, surprisingly after that, the cyst wall became thick and whitish (Figure 2), fastly, reminded us the HC features, so we immediately considered as such; after removing it in one piece, which is very difficult in the AC. The surgical field was irrigated with 3% saline. After ensuring hemostasis, the dura was closed watertigthly and the laminas were fixed with vicryl suture (Figure 2).
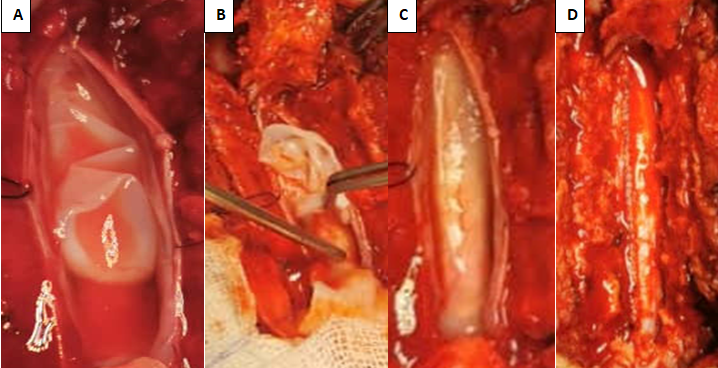
Figure 2. Operative views: (A) Empty cyst after aspiration and irrigation of the surgical field. (B, C) Easy dissection. (D) Watertight dura closure
Postoperatively the patient did well; she had its pain immediately improved. Histopathology straightened out the diagnosis which was consistent with HC. In the histopathological examination, the cyst wall was noted to stain with Hematoxylin and Eosin. There were eosinophilic inflammatory cells in the cyst wall, which supported the presence of a heavy inflammatory reaction, as well as eosinophilic laminar membranous material located in granular eosinophilic debris, which supported a diagnosis of hydatid disease (Figure 3).
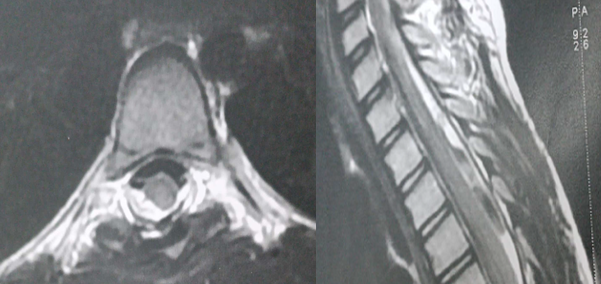
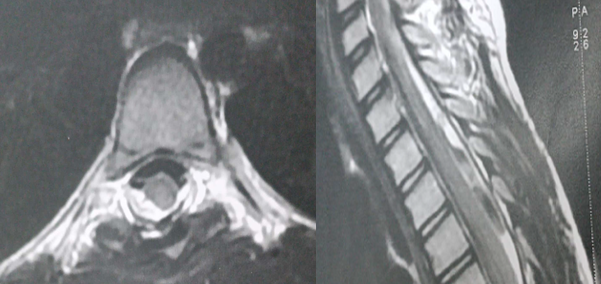
Figure 3. Fellow up MRI shows no evidence of HC
On work up lab: CBC, hydatid serology, craniovertebral MRI, thorax computerized tomography CT and abdominal ultrasound were within normal and no history of outbreak count. Six months after rehabilitation, she recovered totally from weakness, bladder and bowel disorders. The fellow up MR 8-months after surgery showed no evidence of cyst or new localization.
Results and discussion
Spinal AC are rare, benign, CSF filled sacs lined by an arachnoid membrane in the spinal canal. Our case highlights the differential diagnosis of a thoracic subdural extra medullary cystic lesion mimicking CSF appearance at MRI. In lack of evidence such epidemic or pathologic data history of HC; the first diagnosis likely to be evoked is AC; like in our case, as it’s unique and more common in subdural space with such features.
There was discrepancy between radiological diagnosis and intraoperative findings. Histology established the diagnosis of HC which was preoperatively thought to be AC. The error rate among radiologists reported in averages 3%–5%; the same study found that in 26% of cases, à major diagnosis was missed clinically [5].
Hydatidosis of spine was first described by Chaussier in 1807 [6]. Hydatid disease is a zoonotic infection caused primarily by the tapeworm parasite, Echinococcus granulosus. It is considered an endemic disease in the Mediterranean region. In about 90% of cases, HC are found in the liver and lungs. Spine is one of the rare locations for echinococcosis with incidence varying from 0.2% to 1 % [2,7-9].
Any segment of the spine can be affected and most commonly involves the thoracic segment [10]. The majority of the spinal HC were extradural, and primary intradural HC is very rare [11]. Intradural extramedullary HC can be classified into two groups; primary, in which there is no other site for spreading of parasite to central nervous system. In this form, primary hematic dissemination is regarded as the most plausible mechanism. The secondary form is usually due to rupture of intracranial HC and spreading via subarachnoid space during surgery of spontaneously, or spreading from adjacent structures such as spine involvement [12].
With such low incidence and rarity even in endemic regions, the above disease is often missed out as a cause of cord compression. Differential diagnosis of intradural extramedullary cystic lesions includes, HC, hematoma, AC, and dermoid/epidermoid cyst [13].
The clinical presentations of spinal hydatidosis are not pathognomonic regardless of the etiology; compression of adjacent nerve structures can give rise to debilitating symptoms such as radicular pain, sensorimotor disturbances, balance problems and sphincter dysfunction [14]. Unfortunately, specific ELISA/Western blot serology decreases in extrahepatic disease and becomes less sensitive in the spine location, which makes the diagnosis even more challenging [2].
In MRI the lesions have a sausage-like shape (occasionally spherical) with two dome-shaped ends, thin and regular walls and no septations or debris in the lumen. The cyst content is usually similar to CSF. On T1 weighted images, the cyst wall may be isointense or give slightly lower signal than its contents, and T2 weighted images demonstrates a low intensity rim surrounding the homogeneous high-signal cyst content. The cyst wall demonstrates no or slight contrast enhancement. The low signal rim on T2-weighted images results from reactive fibrosis and degeneration around the parasitic membrane and correlates with the histopathological examination. MRI is also very helpful in early diagnosis of postoperative recurrence [15].
When the cysts do not show characteristic MRI features, the differential diagnosis is quite difficult and the lesion can imitate different cystic pathology, as in our case [16,17]. In a reported series of 503 cases of spinal cord compression, of which 2.6% were caused by HC, only one of these cases involved intradural HC (0.2% of spinal compression cases, 7.7% of all spinal hydatidosis [18]. The majority of cysts regardless hydatid or arachnoid are located in the thoracic spine, and AC at the opposite of HC are more common located in intra dural space [19-21]. Spinal intradural and extramedullary without bony and/or systemic involvement is rare; it can occur with direct portovertebral venous shunts. In both lesions, the mainstay management is surgical procedures for relieving the compression of neural elements.
Unlike the AC where the surgery is indicated when it is symptomatic, in the HC is indicated ASAP to prevent any complication like spreading and surinfection [22]. Treatment is mainly total removal without cyst rupture. Careful dissection and irrigation around the cyst is essential to avoid intraoperative cyst rupture, which leads to recurrence; Altinors reported intraoperative rupture of spinal HC in 44% of cases [22].
In our case, the lesion was diagnosed as an AC initially. We planned our surgical approach based on clinical and radiological signs of cord compression. Intraoperative appearance of the cyst, covered by arachnoid, easy dissection from this one and the posterior aspect of the cord was typical for HC, enabling us to avoid the cyst’s rupture. The surgical area should be irrigated with hypertonic saline.
Strict follow up is critical in the management of these patients, and regular MRI should be done to rule out any recurrences. Misdiagnosis of spinal HC as an AC will result in 2 potential sequels. The first one is inadequate follow up of the patient because of lack of evidence of cord compression and clinical signs indicative of AC. The second one is seeding of the organism during surgery and a high risk spreading the hydatid disease.
Prevention by controlling of the live cycle of contamination before affecting the human is far the best way to reduce its burden in endemic areas, of course associated to early diagnosis, proper care and follow-up of the affected patients [23].
Conclusion
Spinal HC is a rare condition, which may mimic any cyst when occurring in uncommon context and does not show typical imaging features, as arachnoid cyst in our case. So it should be considered in the differential diagnosis of cystic lesions of the spine especially in endemic countries such as: Algeria.
A high index of suspicion combined with good quality neuroimaging is important for early and correct diagnosis. Anyway, HC should be kept in mind when planning a surgical approach for any cystic spinal lesions. Total surgical removal of the cyst without rupture should be aimed for. The best treatment remains active nationwide prevention of the disease.
Conflicts of interest
I declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Financial support and sponsoring
None
References
- McManus DP, Zhang W, Li J, Bartley PB (2003) Echinococcosis. Lancet 362: 1295-1304. [Crossref]
- Karadereler S, Orakdögen M, Kiliç K, Özdogan C (2002) Primary spinal extradural hydatid cyst in a child: Case report and review of the literature. Eur Spine J 11: 500-503. [Crossref]
- Pamir MN, Akalan N, Özgen T, Erbengi A (1984) Spinal hydatid cysts. Surg Neurol 21: 53-57. [Crossref]
- Prevo RL, Hageman G, Bruyn RP, Broere G, Van de Stadt J, et al. (1999) Extended extradural spinal arachnoid cyst: An unusual cause of progressive spastic paraparesis. Clin Neurol Neurosurg 101: 260-263. [Crossref]
- Berlin L (2007) Radiologic errors and malpractice: A blurry distinction. AJR Am J Roentgenol 189: 517-522. [Crossref]
- Reddy DR, Murthy JM (1986) Parasitic intracranial space-occupying lesions in children in India. Childs Nerv Syst 2: 244-247. [Crossref]
- Yazdani N, Basam A, Heidarali M, Kashani SS, Hasibi M, et al. (2010) Infratemporal hydatid cyst: A case presenting with blindness. J Laryngol Otol 124: 456-459. [Crossref]
- Lakhdar F, Arkha Y, Rifi L, Derraz S, El Ouahabi A, et al. (2009) Spinal intradural extramedullary hydatidosis: Report of three cases. Neurosurgery 65: 372-377. [Crossref]
- Arif SH, Zaheer S (2009) Intradural extramedullary primary hydatid cyst of the spine in a child: A very rare presentation. Eur Spine J 18: 179-182. [Crossref]
- Bhake A, Agrawal A (2010) Hydatid disease of the spine. J Neurosci Rural Pract 1: 61-62. [Crossref]
- Moharamzad Y, Kharazi HH, Shobeiri E, Farzanegan G, Hashemi F, et al. (2008) Disseminated intraspinal hydatid disease: Case report. J Neurosurg Spine 8: 490-493. [Crossref]
- Kaen A, Lagares A, Perez-Nunez A, Rivas JJ, Lobato RD, et al. (2009) Intradural extramedullary spinal hydatidosis: Case report. Neurocirugia 20: 282-287. [Crossref]
- Guzel A, Tatlı M, Yılmaz F, Bavbek M (2006) Unusual presentation of cervical spinal intramedullary arachnoid cyst in childhood: Case report and review of the literature. Pediatr Neurosurg 43: 50-53. [Crossref]
- Hamdan TA (2012) Hydatid disease of the spine: A report on nine patients. Int Orthop 36: 427-432. [Crossref]
- Berk C, Çiftçi ER, Erdoğan A (1998) MRI in primary intraspinal extradural hydatid disease: Case report. Neuroradiology 40: 390-392. [Crossref]
- Kahilogullari G, Tuna H, Aydin Z, Egemen N, Colpan E, et al. (2005) Primary intradural extramedullary hydatid cyst. Am J Med Sci 329: 202-204. [Crossref]
- Onbas O, Kantarci M, Alper F, Sekmenli N, Okur A, et al. (2004) Spinal widespread intradural extramedullary hydatidosis. Neuroradiology 46: 310-312. [Crossref]
- Işlekel S, Zileli M, Erşahin Y (1998) Intradural spinal hydatid cysts. Eur Spine J 7: 162-164. [Crossref]
- Kalsi P, Hejrati N, Charalampidis A, Wu PH, Schneider M, et al. (2022) Spinal arachnoid cysts: A case series & systematic review of the literature. Brain Spine 2: 100904. [Crossref]
- Prabhakar M, Acharya AJ, Modi DR, Jadav B (2005) Spinal hydatid disease: A case series. J Spinal Cord Med 28: 426-431. [Crossref]
- Braithwaite PA, Lees RF (1981) Vertebral hydatid disease: Radiological assessment. Radiology 140: 763-766. [Crossref]
- Altinors N, Bavbek M, Caner HH, Erdogan B (2000) Central nervous system hydatidosis in Turkey: A cooperative study and literature survey analysis of 458 cases. J Neurosurg 93: 1-8. [Crossref]
- Craig PS, Hegglin D, Lightowlers MW, Torgerson PR, Wang Q, et al. (2017) Echinococcosis: Control and prevention. Adv Parasitol 96: 55-158. [Crossref]