Dry mouth syndrome, alternatively known as Xerostomia, happens when there is inadequate saliva in the mouth. Compared with other medical issues, it can be more than an annoyance; this is because it makes eating less pleasant and causes difficulty in speech. For people with inadequate or no saliva, persistent Xerostomia is an uncomfortable and often serious condition which makes feeding and swallowing difficult, leads to bad breath, and can irritate the tissues of the mouth, which leaves them more susceptible to infection [1]. Dry mouth syndrome also boosts the risk for gum disease and tooth decay. Patients experiencing chronic symptoms associated with dry mouth are some of the most despondent, uncomfortable people who seek treatment in dental practices today.
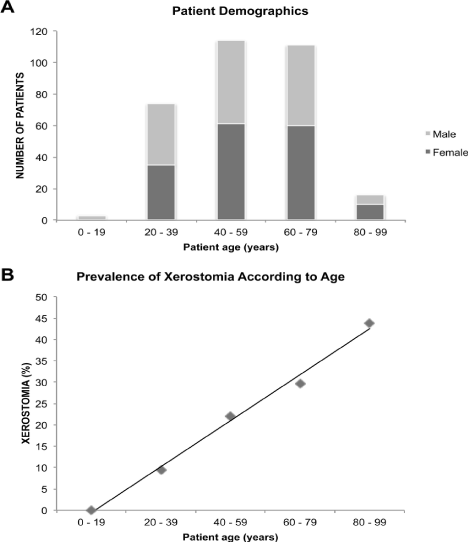
In the general population, a conservative estimation of prevalence is around 20% with higher prevalence in the elderly of up to 50% and 30% in females. The condition is common, and it affects about 5 people per 100,000 general populations. Most people with Dry mouth syndrome are more likely to be elderly or middle-aged, and females are twice more likely to experience it compared to men. It is reported in about 12-40% of women who seek medical treatment for symptoms of menopause, and it occurs in close to 14% of postmenopausal women. In rare cases, males and younger people of both sexes can sometimes be affected, and Caucasians have the highest chances of experiencing dry mouth syndrome [2] (Figure 1).
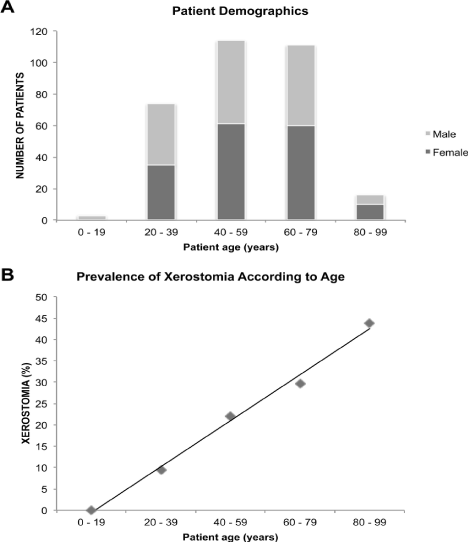
Figure 1. . This graph is an indication of the chances of experiencing dry mouth syndrome, based on gender and age.
The average, healthy individual produces around a quart of saliva every day. It is produced by salivary glands and is made up of 99% water while the remaining 1% consists of up to 60 substances, including enzymes, proteins, and electrolytes. Saliva is an important body fluid that preserves oral functions and guards the oral cavity. During dry mouth syndrome, the loss of electrolytes and salivary proteins accelerate the infection and caries process by boosting the number of detrimental microorganisms and lowering the buffering action [2].
The role of saliva is much more complex that enabling easier swallowing and moistening the food.
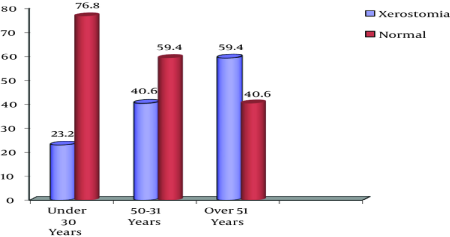
Firstly, it also had protective properties such as the promotion of mineralization through the phosphate and calcium found in saliva; lowered saliva flow, therefore, lowers mineral availability. Secondly, the proteins found in saliva produce lubricating mucins, antibacterial peptides, and protective Catherine, which prevent phosphate and calcium precipitation. Thirdly, it recycles and distributes fluoride. Fourthly, saliva protects soft and hard tooth structures from drying and fifthly, adequate saliva production discourages acidophilic bacteria from growing [3] (Figure 2).
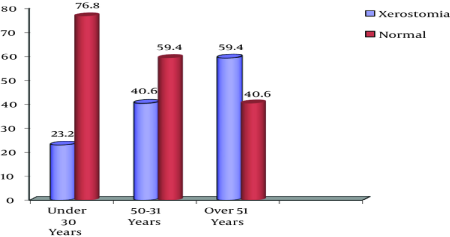
Figure 2. It indicates normal saliva secretion compared to Xerostomia, with a lower production of saliva with an increase in age.
Compromised salivary production will lead to sticky, viscous saliva, a burning or dry feeling in the throat, lips, and mouth, cracked commissures and lips, a biofilm- laden, fissured, and rough tongue, mouth sores, and severe halitosis [4]. These symptoms can cause difficulties such as swallowing dry foods especially without a fluid, mastication, impaired taste, digestion and speaking. Additionally, a dry mouth may intensify dental caries, enable abrasion of prosthetics, initiate thrush infections, unwanted loss of weight, and altering dietary preferences. Because of the multiple probable side effects, dry mouth syndrome can affect a person’s nutritional status, causing insufficiencies in calories, minerals and vitamins [5].
Dry mouth was once considered an unavoidable phase of the ageing process; however, today it is associated with numerous medications and tons of nonpharmacologic conditions, including several cancer treatment regimens. The increasing number of patients experience this condition because of the longer lifespan, plus the medications and diseases that normally-accompany living for several decades. The most affected people are the elderly since they have an increased incidence of using medication and compromised health as a result of disease [6]. Other causes of dry mouth include radiation therapy directed at the neck and head, which can destroy salivary glands, diabetes, stroke depending on severity and type, nerve damage because of surgery. Besides, dry mouth can be caused by trauma or injury, a yeast infection of the mouth known as Oral Thrush, Alzheimer’s Disease, Sjögren’s Syndrome, an autoimmune disease causing excessive eye and mouth dryness, HIV/AIDS and its prescribed medications, excessive alcohol use, and using alcohol-based mouthwashes, and recreational drugs such as marijuana [7].
Dry mouth syndrome is a common side effect of many nonprescription and prescription medications for high blood pressure(diuretics), anxiety, depression, colds including decongestants and antihistamines, allergies, pain including pain relievers and muscle relaxants, epilepsy, acne, obesity, epilepsy, urinary incontinence, psychotic disorders, nausea, diarrhea, Parkinson’s disease, and asthma (specific bronchodilators). Dry mouth syndrome can also be a side effect of sedatives and chemotherapy drugs, which alter the nature and amount of saliva produced. This side effect may be permanent or temporary [8].
After a healthcare practitioner assesses a patient, he should try to identify the probable cause(s) of the dry mouth and educate his patient about this/her condition. He can then offer viable treatment options. Any dental treatment, in the meantime, should be non-invasive. First, it is advisable to change the drugs causing the syndrome and sip melting ice or water. Viable alternatives include regular prophylaxis, diet counseling, steps for rigorous biofilm control, changing home humidity, oral self-examination done daily, avoiding caffeine, acidic drinks, alcohol and tobacco, and applying sealants to fissures and pits and chlorhexidine-thymol blended varnish on root surfaces [9].
Patients can get very uncomfortable, that they prefer electrical stimulation of their salivary glands and acupuncture, in the case where the modalities of the suggested treatments prove unsatisfactory. Definite studies have established that acupuncture alleviates symptoms in several patients who experience dry mouth as a result of radiation. Numerous endorsements and products are available to temporarily substitute for saliva functions, counteract the damage, and compensate for favorable oral environs [10]. Over-the-Counter dry mouth products including mouth rinses, gums, toothpastes, gels, and adhesive tablets contain various agents including lubricants that may aid in treatment of the dry mouth. Alternatively, blockages such as stones in the salivary gland can be treated with surgery; antifungal drugs and antibiotics can treat any infection; and any other treatment, for an underlying conduction such as diabetes and Sjogren's syndrome, require appropriate medical treatment [11].
Modern practice demonstrates that at the caution of speech Pathologist patients experiencing symptoms of dysphagia, in association with dry mouth and saliva viscosity may be prescribed grape seed juice, pineapple juice or paw extract [12]. Pineapple contains bromelain, which aids in degrading the debris in the mouth, it also thins saliva and increases its flow in the mouth while paw extract contains papain which can aid in thinning the thick oral secretions affiliated with a dry mouth [13].
The study involved 100 participants, 60% women, and 40% of men, with 80% elderly and 20% middle-aged. Those with viscous saliva and dry mouth were allowed to participate. The saliva flow rate was measured by chewing paraffin and expectoration for five minutes, and it was calculated in millilitres per minute. These participants underwent a thorough before and after the quality of life survey including questions about the difficulties they are currently facing such as trouble speaking, eating, choking, digestion problems, and dietary changes. Objective dry mouth scores were checked including signs of the dry mouth such as mouth mirror stickiness, foamy or sticky appearance, failing to respond to parotid stimulation, labial dehydration, and loss of pooled saliva. The scores were calculated as numbers from five signs. A person with less than 2 signs was excluded [14].
The aims included investigating the impacts of papaya enzymes in patients who have dry mouth, to determine the affiliation of immunological and microbiological outcomes with the clinical data collected from the study participants. The study also aims to investigate the quality of life of the participants, identify the mental health wellbeing of the patients because of consuming papaya enzyme and introduce a product that supersedes the current options available in the market.
These participants have previously suffered from dry mouth as a result of prescribed and non-prescribed drugs, they have diseases such as diabetes, cancer, HIV/AIDS, and other conditions, have had a case of oral candidiasis, or have received medical therapies. The treatment period would last seven days utilise the papaya enzyme formula. As instructed, the formula was administered as a moisturising mouth spray under the supervision of trained healthcare professionals on their visits. The spray was sprayed by the participants in one jet directly into the mouth. The assigned treatment product was used at least two times and no more than five in a day [15].
The saliva flow rate for the participants was below 0.7 millilitres per minute for 77%of patients, while 10% had a thicker viscosity of fewer than 0.1 ml. Female patients had a higher percentage of the participants with less than 0.1 ml by 15%. As displayed by the cotton swabs, 62% of the participants suffered from coliforms (oral thrush), candida albumens as well as dry mouth. Finally, 100% of the patients admitted that their dry mouths lowered their quality of life with difficulties in chewing, swallowing, choking, speaking, and experienced less sense of taste, changed their diets which caused weight loss. 30% of participants experienced at least 5 of these difficulties with 65% experiencing four, and 5%experiencingless than four [16].
100% of participants reported a boosted quality of life, improved taste, and a marked improvement in terms of dry mouth quality and decreased thirst. Saliva flow rate heightened for 100% of the participants who experienced decreased saliva flow, with the rate being above 1.0 ml per minute 100% of cases. The mouth swabs results also showed an improvement through reduction of the number of coliforms and candida albicans found in the mouth within the seven days, as a result of the papaya enzyme spraying, therefore, lowering or eliminating the oral thrush [17]. In 87% of the participants, oral thrush was completely eradicated while the remaining 13% exhibited lower coliform and candida albumen results. 100% of participants agreed on the exception to a good boost in their happiness and general well-being and happiness, with 77%of patients feeling less thirsty, 82% reported that their speech and swallowing had dramatically improved, and 30% stated they no longer required water when swallowing food [18].
Participants admitted that they preferred Papaya Enzymes Formula compared to the mouth rinses, substitutes, and gels that they were previously using. After consuming a dose of the formula, most participants required an additional dose three hours later, suggesting that the formula can retain moistness in the mouth for close to three hours. 100% of the patients agreed that compared to the gels, saliva substitutes, antibiotics, adhesive tablets, oralube, biotenes, and lozenges that they previously consumed, the satisfaction of the formula was the highest [19]. The treatment was, therefore, more effective compared to all the other treatments they had previously used. Therefore, Papaya Enzymes Formula supersedes all the available products for treating this condition.
- American Dental Association Council on Scientific Affairs (2011) Non-fluoride caries preventive agents -- A systematic review and evidence-based recommendations. J Amer Dental Association 142: 78-82. [Crossref]
- Leal SC, Bittar J, Portugal A, Falcão DP, Faber J, et al. (2010) Medication in elderly people: its influence on salivary pattern, signs and symptoms of dry mouth. Gerodontology 27: 129-133. [Crossref]
- Sugai S, Takahashi H, Ohta S, Nishinarita M, Takei M, et al. (2009) Efficacy and safety of rebamipide for the treatment of dry mouth symptoms in patients with Sjögren’s syndrome: a double-blind placebo-controlled multicenter trial. Mod Rheumato 19: 114-124. [Crossref]
- Cornec D, Saraux A, Jousse-Joulin S, Pers JO, Boisramé-Gastrin S, et al. (2015) The differential diagnosis of dry eyes, dry mouth, and parotidomegaly: a comprehensive review. Clin Rev Allergy Immunol 49: 278-287. [Crossref]
- Agha-Hosseini F, Mirzaii-Dizgah I, Mirjalili N (2012) Relationship of stimulated whole saliva cortisol level with the severity of a feeling of dry mouth in menopausal women. Gerodontology 29: 43-47. [Crossref]
- Silvestre FJ, Minguez MP, Suñe-Negre JM (2009) Clinical evaluation of a new artificial saliva in spray form for patients with dry mouth. Med Oral Patol Oral Cir Bucal 14: E8-E11. [Crossref]
- Puntillo K, Arai SR, Cooper BA, Stotts NA, Nelson JE (2014) A randomized clinical trial of an intervention to relieve thirst and dry mouth in intensive care unit patients. Intensive Care Med 40: 1295-1302. [Crossref]
- Park MS, Ryu SA (2010) Degree of dry mouth and factors influencing oral health-related quality of life for community-dwelling elders. J Korean Acad Nurs 40: 747-755. [Crossref]
- Farsi NM (2007) Signs of oral dryness in relation to salivary flow rate, pH, buffering capacity and dry mouth complaints. BMC Oral Health 7: 15. [Crossref]
- Vitali CBSJ, Del Papa N (2016) Classification criteria for Sjögren’s syndrome. In Sjögren's Syndrome pp: 47-60.
- Furness S, Bryan G, McMillan R, Worthington HV (2013) Interventions for the management of dry mouth: non-pharmacological interventions. Cochrane Database Syst Rev p. 8. [Crossref]
- Napeñas JJ, Brennan MT, Fox PC (2009) Diagnosis and treatment of xerostomia (dry mouth). Odontology 97: 76-83. [Crossref]
- Furness S, Worthington HV, Bryan G, Birchenough S, McMillan R (2011) Interventions for the management of dry mouth: topical therapies. Cochrane Database Syst Rev 12: CD008934. [Crossref]
- Humphrey SP, Williamson RT (2001) A review of saliva: normal composition, flow, and function. J Prosthet Dent 85: 162-169. [Crossref]
- Wong RKW, Jones GW, Sagar SM, Babjak AF, Whelan T (2003) A phase I-II study in the use of acupuncture-like subcutaneous nerve stimulation in the treatment of radiation-induced xerostomia in head-and-neck cancer patients treated with radical radiotherapy. Int J Radiat Oncol Biol Phys 57: 472-480. [Crossref]
- Turner MD, Ship JA (2007) Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc 138: 15S-20S. [Crossref]
- Pedersen AM, Bardow A, Jensen SB, Nauntofte B (2002) Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis 8: 117-129. [Crossref]
- Hopcraft MS, Tan C (2010) Xerostomia: an update for clinicians. Aust Dent J 55: 238-244. [Crossref]
- Wilkins EM (2009) Clinical Practice of the Dental Hygienist. (10th Edn) Philadelphia, Wolters-Kluwer p. 391.