Abstract
Background: Cervical insufficiency is a common condition in obstetrics and reproductive medicine. Cervical cerclage is widely used in clinical practice as a treatment for this condition and has improved the perinatal outcomes of singleton pregnancies to a certain extent. However, for twin pregnancies with in vitro fertilization and embryo transfer (IVF-ET) involving cervical insufficiency, whether and to what extent can they benefit from cervical cerclage remains unclear. This study tests the following hypothesis: IVF-ET twin pregnant women with cervical insufficiency may benefit from rescue McDonald cervical cerclage.
Methods: Study subjects involved patients undergoing emergency and rescue cervical cerclage. Specifically, these were patients admitted due to threatened abortion, with a dilated cervical os of more than 1 cm and visible protrusion of the amniotic sac into the cervical os upon examination. This included singleton and twin pregnancies. Maternal outcomes included gestational age at surgery, surgical indications, intraoperative blood loss, prolonged gestational age, gestational age at delivery, etc. Neonatal outcomes included neonatal birth weight, delivery method, Apgar score, neonatal survival rate, etc. Patients undergoing McDonald cervical cerclage received intraoperative and postoperative intravenous infusion of β-adrenergic agonists or atosiban acetate to inhibit uterine contractions.
Results: A total of 15 singleton pregnant women and 11 twin pregnant women after assisted reproduction were included in the study. The proportion of history-indicated cervical cerclage was higher in the singleton pregnancy group, while the proportion of ultrasound-indicated cervical cerclage was higher in the twin pregnancy group. There was no statistically significant difference in the gestational age at delivery between two groups. No statistically significant differences were observed between the two groups in the diagnosis-to-surgery interval, or in the cerclage-to-delivery interval. The 1-minute and 5-minute Apgar scores of newborns showed no statistically significant differences between the two groups. There was a statistically significant difference in birth weight between the two groups of newborns (P=0.045). Additionally, no statistically significant differences were found in the cesarean section rate or intrapartum blood loss between the two groups.
Conclusion: The efficacy of cervical cerclage in treating IVF-ET twin pregnant women with cervical insufficiency was similar to that in singleton pregnant women, suggesting that IVF-ET twin pregnant women with cervical insufficiency may benefit from cervical cerclage.
Keywords
cervical incompetence, in vitro fertilization and embryo transfer, McDonald cervical cerclage, premature birth, twin pregnancy, ultrasound
Introduction
Cervical insufficiency is a common condition in obstetrics and reproductive medicine. It refers to painless cervical dilatation in the second trimester of pregnancy and is one of the main causes of recurrent late miscarriages and preterm births [1,2]. Worldwide, approximately 15 million infants are born prematurely each year, and more than 1 million infants die from preterm birth-related causes [3]. Statistics show that patients with cervical insufficiency account for 8%–9% of all preterm births and 40%–50% of spontaneous preterm births [4,5]. Although the pathogenesis of cervical insufficiency remains unclear, cervical cerclage is widely used in clinical practice as a treatment for this condition and has improved the perinatal outcomes of singleton pregnancies to a certain extent [6-8].
For twin pregnancies complicated with cervical insufficiency, current literature does not support the performance of cervical cerclage based on cervical length. If cerclage is performed based on ultrasound findings of shortened cervix (<25 mm), it may increase the risk of preterm birth [9]. Prophylactic cervical cerclage provides no significant benefits for twin pregnant patients with a cervical length <25 mm; instead, it may increase the risk of preterm birth. For twin pregnant patients with cervical canal dilatation (>1 cm), emergency cervical cerclage should be considered if preterm birth occurs when the fetus is not yet viable. The potential benefits of different indications for cerclage in multiple pregnancies are inconsistent. Ultrasound-indicated and history-indicated cervical cerclage may be ineffective in treating cervical insufficiency in twin pregnancies [10-12], but physical examination-indicated cervical cerclage may benefit twin pregnant patients with cervical insufficiency [13].
The incidence of twin pregnancies involving in vitro fertilization and embryo transfer (IVF-ET) is much higher than that in natural pregnancies. High estrogen exposure during IVF-ET is an important predisposing factor for cervical insufficiency in pregnant women who undergo assisted reproductive technology. Therefore, whether and to what extent IVF-ET twin pregnant women with cervical insufficiency can benefit from cervical cerclage remains unclear, and this is an urgent clinical problem to be solved. Thus, this study tests the following hypothesis: IVF-ET twin pregnant women with cervical insufficiency may benefit from cervical cerclage.
Materials and methods
Study subjects
Pregnant women with cervical insufficiency via IVF-ET in the Reproductive Endocrinology Department of Hangzhou Women’s Hospital from January 2022 to December 2024 were screened and included in the study.
Inclusion criteria
i) Patients undergoing emergency and rescue cervical cerclage indicated by physical examination. Specifically, these are patients admitted due to threatened abortion, with a dilated cervical os of more than 1 cm and visible protrusion of the amniotic sac into the cervical os upon examination. Patients indicated by ultrasound and medical history have a closed cervical os. This includes singleton and twin pregnancies (triplet and higher pregnancies have undergone routine fetal reduction). All included pregnant women have signed the informed consent form.
ii) Pregnant women with a gestational age of 14–28 weeks who can tolerate the surgery.
Exclusion criteria
i) Patients with a cervical os dilated more than 5 cm, where abortion is inevitable.
ii) Patients in the active phase of genital, urinary, or systemic infections, or with obvious signs of intrauterine infection before receiving tocolytic treatment. The diagnostic criteria for intrauterine infection are as follows: maternal body temperature ≥ 38.0 ℃; maternal heart rate ≥ 100 beats/min; uterine tenderness; maternal peripheral blood leukocyte count ≥ 15.0×109/L and neutrophil ratio ≥ 95%; fetal heart rate ≥ 160 beats/min; positive culture of cervical secretions; positive culture of secretions from the neonatal oropharynx and external auditory canal; placental pathological examination indicating infection. Clinical intrauterine infection is diagnosed when two or more of the above criteria are met.
iii) Ruptured fetal membranes, placental abruption, severe congenital fetal malformations, intrauterine fetal death, or fetal malformations.
iv) Pregnant women with severe medical or surgical comorbidities requiring pregnancy termination, or patients with preterm labor due to medical indications.
v) Patients after fetal reduction for multiple pregnancies with a gestational age exceeding 14 weeks.
vi) Monochorionic monoamniotic twin pregnancies.
vii) Patients lost to follow-up or those who requested withdrawal from the study.
The research protocol was approved by the Institutional Review Board of Hangzhou Women’s Hospital on November 15, 2021. Approval number: (2021) Medical Ethics Review A No. 7-11.
Diagnostic methods
Medical history
Patients have a clear history of cervical injury or a history of recurrent spontaneous abortion in the second trimester (more than two times). Abortions usually occur at the same gestational age, without obvious abdominal pain or uterine contractions, and the labor process progresses rapidly, accompanied by significant shortening of the cervical canal and cervical dilatation. Before the onset of symptoms, patients often only feel pelvic pressure or increased mucus secretion.
Physical examination
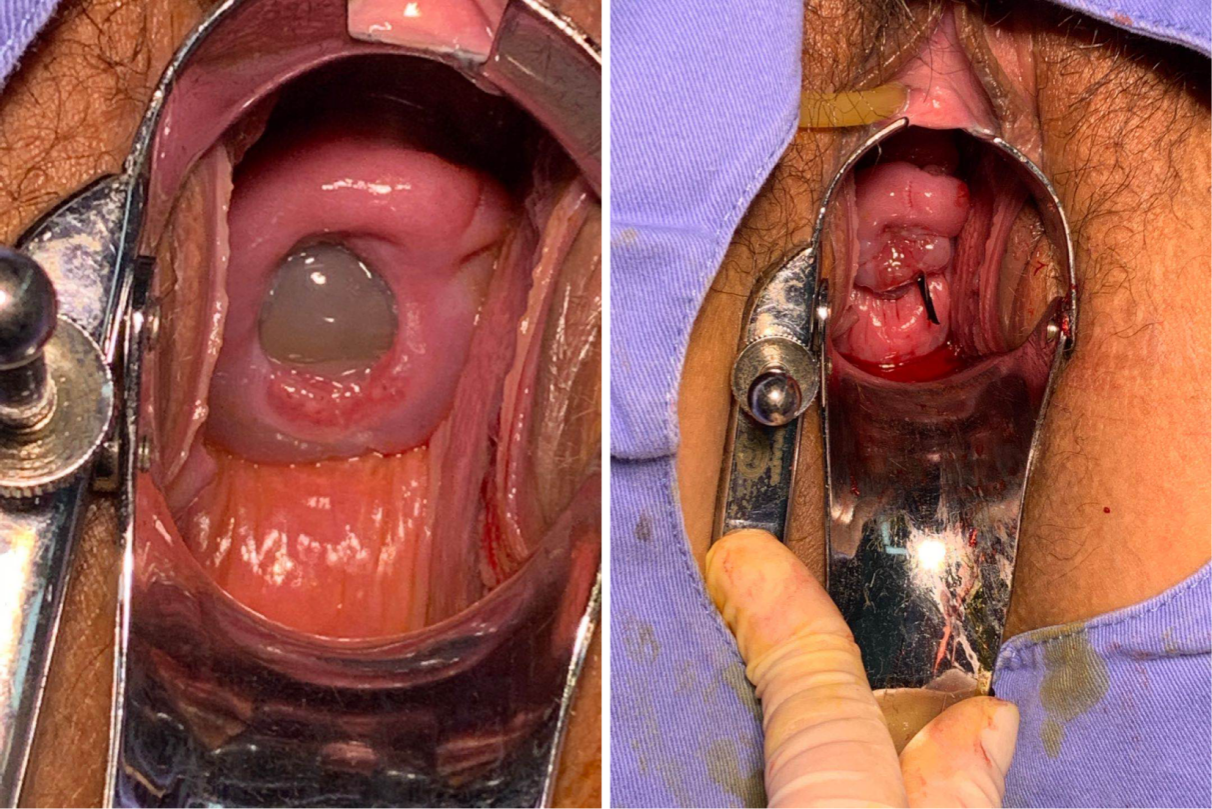
In the second trimester, there is no obvious abdominal pain, but the internal cervical os is dilated more than 1 cm, and the cervical canal is shortened and softened—with softening being particularly important. Sometimes, the amniotic sac has protruded outside the cervical os (Figure 1 A).
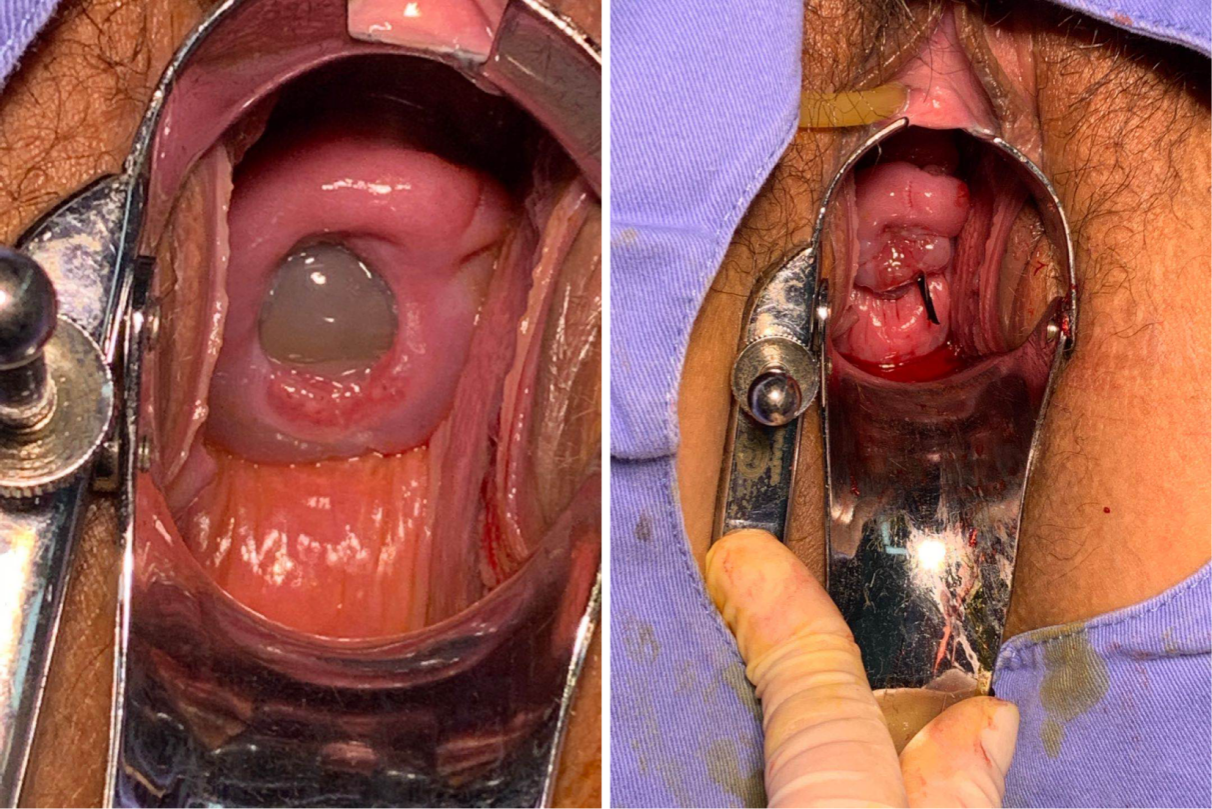
Figure 1. (A) Protrusion of the amniotic sac through the cervical os before cervical cerclage in a patient with cervical insufficiency. (B) Cervical condition after McDonald cervical cerclage
Main outcome measures
General information
Patient medical history, past pregnancy history, age, body mass index (BMI), number of pregnancies, number of deliveries, history of early abortion and spontaneous abortion in the second trimester, history of preterm delivery and term delivery, preoperative ultrasound-measured cervical length and internal cervical os width, etc.
Clinical outcomes
Maternal outcomes include gestational age at surgery, surgical indications, intraoperative blood loss, prolonged gestational age, gestational age at delivery, etc. Neonatal outcomes include neonatal birth weight, delivery method, Apgar score, neonatal survival rate, etc.
Surgical methods
Definition of emergency cervical cerclage and rescue cervical cerclage
When the cervical os is already dilated, and the amniotic sac, or even fetal limbs have entered the vagina, this situation is classified as emergent cervical cerclage. When the external cervical os is closed but the internal os is open in a U-shape, and the amniotic sac remains inside the cervical canal without protruding, this is referred to as rescue cervical cerclage.
Cervical cerclage techniques
Patients undergoing McDonald cervical cerclage receive intraoperative and postoperative intravenous infusion of β-adrenergic agonists or atosiban acetate to inhibit uterine contractions. Patients are anesthetized with single spinal anesthesia, epidural anesthesia, or combined spinal-epidural anesthesia. They are placed in the lithotomy position, with the buttocks at the edge of the operating table, and the left and right hips flexed so that both thighs form a 90° angle with the operating table surface and are abducted as much as possible. Routine disinfection of the vulva, vagina, and cervix is performed. Vaginal retractors are used to fully expose the cervix, and the length, width, and tightness of the internal cervical os are examined to determine the location and height for cerclage suturing. Subsequently, cervical forceps are used to clamp the anterior and posterior lips of the cervix and pull them slightly downward. Slightly below the transverse vesical sulcus, at the level of the internal cervical os near the vaginal fornix, a large round needle with double-stranded 10 # silk thread is used. We insert the needle at the 11 o'clock position of the cervix and penetrate it into the submucosal layer of the cervix for cerclage. The first suture is placed between the 11 o'clock and 10 o'clock positions. The needle and thread continue counterclockwise to place sutures at the 8–7 o'clock, 5–4 o'clock, and 2–1 o'clock positions of the cervix. Both needle insertion and removal are performed within the cervical tissue without penetrating the cervical mucosa. Finally, the needle is removed at the 12 o'clock position, and the suture is tightened to a degree that allows the passage of a 4 # cervical dilator. Generally, the diameter of the cervical canal is reduced to 0.5–1 cm. The suture is tied tightly at the anterior vaginal fornix, with a 2–3 cm length of thread left at the end for future removal (Figure 1 B). For patients with the amniotic sac protruding into the cervical canal, the patient is placed in a hip-elevated position. When tying the knot, the index finger is inserted into the cervical canal to gently reposition the amniotic sac. After tightened the suture, the cervical suture site is checked for bleeding. For patients with active bleeding, iodophor gauze is used for compression to stop the bleeding.
Postoperative antibiotics are administered orally or intravenously to prevent infection. Postoperative uterine contraction inhibition is performed routinely as follows:
i) Magnesium sulfate (for patients with a gestational age < 20 weeks).
ii) Ritodrine hydrochloride (for patients with a gestational age ≥ 20 weeks).
Suture removal techniques
For patients delivering vaginally, hospitalization is arranged at 36 weeks of gestation for removal of the cervical cerclage suture. For patients with indications for cesarean section, the cerclage suture is removed after the cesarean section. If clear signs of infection are detected during labor, the cervical suture is removed immediately. For patients with preterm labor and ruptured fetal membranes, the timing of suture removal is determined based on factors such as the presence of infection signs and gestational age. For patients with preterm labor accompanied by regular uterine contractions and abdominal pain, the suture is removed immediately if regular contractions persist with cervical dilatation of more than 3 cm despite the use of tocolytics.
Statistical methods
Statistical analysis of the data was performed using SPSS 21.0 software. Measurement data with a normal distribution were expressed as x ̅±s, and the Student's t test was used for comparison between groups. Measurement data with a non-normal distribution were expressed as Mean (25th and 75th percentile), and the Mann Whitney U test was used for comparison between the two groups. Count data were expressed as frequencies and percentages, and the χ2 test was used for comparison. A P value of less than 0.05 was considered statistically significant.
Results
A total of 15 singleton pregnant women and 11 twin pregnant women after assisted reproduction were included in the study, with their baseline data shown in Table 1. There was no statistically significant difference between the two groups in terms of maternal age and BMI. The proportions of previous preterm births and term births were not statistically different between the two groups of pregnant women. There was no difference in the fresh embryo transfer rate between the two groups. No pregnant women in the singleton pregnancy group had cervical dilation greater than 2 cm. The length of the closed cervical segment showed a statistically significant difference between the two groups (P=0.018). There was no statistically significant difference in the incidence of fetal membrane protrusion between the two groups. No statistically significant differences were found in the indications (medical history, physical examination, and ultrasound) between the two groups. The proportion of medical history-indicated cervical cerclage in the singleton pregnancy group was as high as 55.6%, while the proportion of ultrasound-indicated cervical cerclage in the twin pregnancy group reached 54.5%. There was no statistically significant difference in the gestational age at the time of cerclage between the two groups.
The cerclage outcomes of the two groups of pregnant women are recorded in Table 2. There was no statistically significant difference in the gestational age at delivery between the two groups. No statistically significant differences were observed between the two groups in the diagnosis-to-surgery interval, or in the cerclage-to-delivery interval. The 1-minute and 5-minute Apgar scores of newborns showed no statistically significant differences between the two groups. There was a statistically significant difference in birth weight between the two groups of newborns (P=0.045). Additionally, no statistically significant differences were found in the cesarean section rate or intrapartum blood loss between the two groups.
Detailed records of twin pregnancies are presented in Table 3. It can be seen that all cerclage procedures were performed using the McDonald technique, and 18.2% of the procedures (2 out of 11) were emergency operations. The cesarean section rate was 72.7% (8 out of 11), and the newborn survival rate was 81.8% (18 out of 22).
Discussion
Cervical cerclage can be performed through multiple approaches. Classified by surgical indications, it is divided into history-indicated cervical cerclage, ultrasound-indicated cervical cerclage, and physical examination-indicated cervical cerclage [14-17].
History-indicated cerclage is a prophylactic procedure, determined based on the patient’s typical medical history of cervical insufficiency. It is mainly used for patients with a history of unexplained mid-trimester fetal loss without having history of labor signs or placental abruption. Cerclage for typical history indications is generally performed between 14 and 16 weeks of gestation. Clinical randomized controlled trials (RCTs) have been reported to demonstrate the efficacy of history-indicated cerclage. One such trial conducted a randomized controlled study on 1,292 singleton pregnant women at risk of preterm birth. The results showed that the rate of preterm birth before 33 weeks of gestation was significantly lower in patients who underwent cervical cerclage compared with the patients who did not [3].
Ultrasound-indicated cerclage is typically used for patients in whom ultrasound detects shortened cervical length, with or without funneling [18]. These patients are usually asymptomatic, though some reports note that they may have non-specific symptoms of cervical insufficiency, including back pain, uterine contractions, vaginal bleeding, pelvic pressure, and increased vaginal mucus discharge. Transvaginal ultrasound for assessing cervical length has been widely used in clinical practice [19]. Recent researches show that for most singleton pregnant patients at risk of cervical insufficiency, serial transvaginal ultrasound monitoring during the second trimester is safe. Continuous monitoring should start at 16 weeks and end at 24 weeks of gestation, which can avoid more than half of unnecessary history-indicated cerclage procedures [20-22].
A meta-analysis of multi-center randomized trials compared patients who underwent cerclage and those who did not, based on mid-trimester ultrasound findings of a short cervix. The conclusions are as follows: i) For singleton pregnant women with a history of spontaneous preterm birth before 34 weeks and a shortened cervix (<25 mm) before 24 weeks of gestation, cervical cerclage is effective [23]. Cervical cerclage helps significantly reduce preterm birth outcomes and improve neonatal morbidity and mortality; it is worth considering for pregnant women with abnormal ultrasound findings combined with a positive medical history. ii) For patients without a history of spontaneous preterm birth but with a cervical length <25 mm between 16 and 24 weeks of gestation, cerclage cannot significantly reduce the occurrence of preterm birth [24].
Physical examination-indicated cervical cerclage is also known as emergency cervical cerclage or rescue cervical cerclage. The appropriate candidates for this procedure are patients with progressive cervical dilatation without obvious causes, after excluding factors such as labor signs and placental abruption [25]. Small-sample randomized controlled trials and some retrospective studies have found that cervical cerclage may be effective for patients who meet physical examination indications [26]. Therefore, if technically feasible, and after clinical examination rules out uterine contractions, intra-amniotic infection, or both, physical examination-indicated cerclage is beneficial for singleton pregnant patients with cervical internal os dilatation. Since there is a lack of large-sample clinical randomized controlled trials to provide further detailed clarification, pregnant women should be informed of the relevant risks of the procedure and information about perinatal morbidity before undergoing physical examination-indicated cervical cerclage [27].
For second trimester cervical cerclage, transvaginal cervical cerclage is generally used. Specific methods can be divided into the McDonald method and the Shirodkar method. Transvaginal cervical cerclage has low surgical risk and light burden on patients; the suture can be removed before delivery to allow vaginal delivery. Among transvaginal cervical cerclage procedures, the McDonald cervical cerclage is more widely used. It does not require incising cervical tissue and instead performs suturing at the cervicovaginal junction, making it widely used in clinical practice. Its main role is to reduce the load on the lower uterus and the tension of uterine muscle fibers, restoring the cervix to its normal shape, and ensuring the cervical internal os exert its normal restrictive function, thereby achieving the effect of maintaining pregnancy until term or extending the gestational age [28]. This surgical method does not require incising any tissue, therefore it causes minimal damage to the cervix. It is the first choice for patients with fetal membranes protruded through the cervical os into the vagina. Study shows that it has a certain preventive effect on high-risk groups; at the same time, some studies have found that when the amniotic sac protrudes through the external cervical os and prolapses into the vagina, the McDonald cerclage is the first choice [29]. If necessary, performing the McDonald cerclage again above the first knot one week later can achieve relatively satisfactory clinical results.
In our study cohort, the proportion of history-indicated cervical cerclage was higher in the singleton pregnancy group, while the proportion of ultrasound-indicated cervical cerclage was higher in the twin pregnancy group. This indicates that the twin pregnancy group had more cases of latent cervical dilatation—specifically, the internal cervical os showed a U-shaped dilatation while the external cervical os remained closed. The results of our study showed no statistically significant differences between the two groups of pregnant women in terms of gestational age at delivery, interval between cerclage and delivery, 1-minute and 5-minute neonatal Apgar scores, and neonatal birth weight.
Conclusion
The efficacy of cervical cerclage in treating IVF-ET twin pregnant women with cervical insufficiency was similar to that in singleton pregnant women, suggesting that IVF-ET twin pregnant women with cervical insufficiency may benefit from cervical cerclage. This study is a single-center retrospective study with a small sample size, which prevented stratified analysis of the indications for cerclage (medical history, physical examination, and ultrasound). With a small sample size, there may be selection bias in the data. In future research, the sample size needs to be further expanded to clarify the efficacy of cervical cerclage in treating IVF-ET twin pregnant women with cervical insufficiency.
Conflicts of interest
The author declares no conflict of interest.
Acknowledgment
We acknowledge support provided by the Zhejiang Province Medical and Health Science and Technology Plan Project (grant number 2022KY1017).
Funding
This work was supported by the Zhejiang Province Medical and Health Science and Technology Plan Project (grant number 2022KY1017).
IRB approval
The research protocol was approved by the Institutional Review Board of Hangzhou Women’s Hospital on November 15, 2021. Approval number: (2021) Medical Ethics Review A No. 7-11.
Data availability statement
Data is available from the authors upon reasonable request.
References
- Rottenstreich A, Levin G, Kleinstern G, Zigron R, Rottenstreich M, et al. (2019) History‐indicated cervical cerclage in management of twin pregnancy. Ultrasound Obstet Gynecol 54: 517-523. [Crossref]
- Huang X, Saravelos SH, Li TC, Huang R, Xu R, et al. (2019) Cervical cerclage in twin pregnancy. Best Pract Res Clin Obstet Gynaecol 59: 89-97. [Crossref]
- D'Antonio F, Eltaweel N, Prasad S, Flacco ME, Manzoli L, et al. (2023) Cervical cerclage for prevention of preterm birth and adverse perinatal outcome in twin pregnancies with short cervical length or cervical dilatation: A systematic review and meta-analysis. PLoS Med 20: e1004266. [Crossref]
- Wierzchowska-Opoka M, Kimber-Trojnar Z, Leszczynska-Gorzelak B (2021) Emergency cervical cerclage. J Clin Med 10: 1270. [Crossref]
- Paily VP, Ramakrishnan S, Sidhik A, Girijadevi RR, Sudhamma A, et al. (2025) Cervical insufficiency management with elective transvaginal cervicoisthmic cerclage. J Obstet Gynaecol India 75: 142-147. [Crossref]
- Sung JH, Kang D, Hong SY, Park H, Lee YR, et al. (2025) Short- and long-term neonatal outcomes according to cerclage in nulliparous singleton women: A national cohort study over 15 years. J Korean Med Sci 40: e131. [Crossref]
- Jafarzade A, Aghayeva S, Mungan TM, Biri A, Jabiyev E, et al. (2024) Perinatal outcomes of emergency and elective cervical cerclages. Eur J Obstet Gynecol Reprod Biol X 21: 100276. [Crossref]
- Mullin J, O'Sullivan HR, Shennan AH, Suff N (2023) Outcomes following elective cerclage versus ultrasound surveillance in women with one prior preterm event. Eur J Obstet Gynecol Reprod Biol 290: 1-4. [Crossref]
- Ipek G, Tanacan A, Demet I, Agaoglu Z, Basaran E, et al. (2025) Efficiency of cervical cerclage and pessary in addition to vaginal progesterone to prevent preterm birth in twin pregnancies: A case-control study from a tertiary center. Turk J Med Sci 55: 271-276. [Crossref]
- Abbott D, To M, Shennan A (2012) Cervical cerclage: A review of current evidence. Aust N Z J Obstet Gynaecol 52: 220-223. [Crossref]
- Roman A, Rochelson B, Fox NS, Hoffman M, Berghella V, et al. (2015) Efficacy of ultrasound-indicated cerclage in twin pregnancies. Am J Obstet Gynecol 212: 788 e781-786. [Crossref]
- Saccone G, Rust O, Althuisius S, Roman A, Berghella V (2015) Cerclage for short cervix in twin pregnancies: Systematic review and meta-analysis of randomized trials using individual patient-level data. Acta Obstet Gynecol Scand 94: 352-358. [Crossref]
- Giouleka S, Boureka E, Tsakiridis I, Siargkas A, Mamopoulos A, et al. (2023) Cervical cerclage: A comprehensive review of major guidelines. Obstet Gynecol Surv 78: 544-553. [Crossref]
- Dang VQ, He YT, Pham HN, Trieu TT, Bui TQ, et al. (2020) Effectiveness of cervical pessary compared to cervical cerclage with or without vaginal progesterone for the prevention of preterm birth in women with twin pregnancies and a short cervix: Study protocol for a two-by-two factorial randomised clinical trial. BMJ Open 10: e036587. [Crossref]
- He YTN, Pham HNH, Nguyen TC, Bui TQ, Vuong NT, et al. (2025) Cervical cerclage versus cervical pessary with or without vaginal progesterone for preterm birth prevention in twin pregnancies and a short cervix: A two-by-two factorial randomised clinical trial. PLoS Med 22: e1004526. [Crossref]
- Wu FT, Chen YY, Chen CP, Sun FJ, Chen CY (2020) Outcomes of ultrasound-indicated cerclage in twin pregnancies with a short cervical length. Taiwan J Obstet Gynecol 59: 508-513. [Crossref]
- Suff N, Hall M, Shennan A, Chandiramani M (2020) The use of quantitative fetal fibronectin for the prediction of preterm birth in women with exposed fetal membranes undergoing emergency cervical cerclage. Eur J Obstet Gynecol Reprod Biol 246: 19-22. [Crossref]
- Rawashdeh H, Ramachandran A, Yang JM, Blain G, Hyett J (2024) Changing indications for cervical cerclage following the introduction of routine ultrasound surveillance of cervical length for prediction and prevention of preterm birth. Int J Womens Health 16: 1755-1764. [Crossref]
- Yao LP, Yang Q, Pei JD, Wu YL, Wan S, et al. (2022) Ultrasound-indicated cervical cerclage efficacy between 16 and 28 weeks of gestation in twin pregnancy: Retrospective cohort study. Int J Gen Med 15: 2377-2387. [Crossref]
- Brown JA, Pearson AW, Veillon EW, Rust OA, Chauhan SP, et al. (2011) History- or ultrasound-based cerclage placement and adverse perinatal outcomes. J Reprod Med 56: 385-392. [Crossref]
- Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM (2005) Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol 106: 181-189. [Crossref]
- Berghella V, Mackeen AD (2011) Cervical length screening with ultrasound-indicated cerclage compared with history-indicated cerclage for prevention of preterm birth: A meta-analysis. Obstet Gynecol 118: 148-155. [Crossref]
- Berghella V, Rafael TJ, Szychowski JM, Rust OA, Owen J (2011) Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: A meta-analysis. Obstet Gynecol 117: 663-671. [Crossref]
- Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA (2010) Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol 35: 468-473. [Crossref]
- Song JE, Park S, Ryu J (2023) Physical examination-indicated cerclage in singleton and twin pregnancies and risk factors for predicting preterm birth < 28 weeks. J Pers Med 14: 38. [Crossref]
- Althuisius SM, Dekker GA, Hummel P, Bekedam DJ, van Geijn HP (2001) Final results of the Cervical Incompetence Prevention Randomized Cerclage Trial (CIPRACT): Therapeutic cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol 185: 1106-1112. [Crossref]
- Yalinkaya A, Oglak SC, Gunduz R, Yilmaz EZ, Bolluk G, et al. (2025) Outcomes of emergency cervical cerclage after amnioreduction in twin pregnancies with a fully dilated cervix and amniotic membrane prolapse. J Turk Ger Gynecol Assoc 26: 26-33. [Crossref]
- Burger NB, Einarsson JI, De Leeuw RA, Huirne JA (2020) MAVRIC: A multicentre randomized controlled trial of transabdominal vs transvaginal cervical cerclage. Am J Obstet Gynecol 222: 516. [Crossref]
- Fichera A, Prefumo F, Mazzoni G, Molinaris V, Zanardini C, et al. (2019) The use of ultrasound-indicated cerclage or cervical pessary in asymptomatic twin pregnancies with a short cervix at midgestation. Acta Obstet Gynecol Scand 98: 487-493. [Crossref]