Abstract
A Prospective study to examine general trends of malpractice of antibiotics prescription in Gastroenteritis pediatrics patients in Southern Punjab (Multan) from Children Complex Hospital and Nishtar Hospital Multan survey. 500 children ≥15 years with inpatients were selected for non-probability purposive sampling, classified on the basis of diagnostic category: 1) Diarrhoea occur in all paeds patients, 2) 459 patients with complaints of vomiting, 3) 324 patients with complaints of abdominal cramps, 4) 421 with complaints of bloating and 5) fever occur in all paeds patients. Chi-square analysis and one-way ANOVA of antibiotics were performed by using SPSS software. Antibiotics prescription trends in: 1) 456 proportion of inpatients received antidiarrheal, 2) 387 proportion of inpatients received antiemetic, 3) 479 proportion of inpatients received antispasmodic,4) 289 proportion of inpatients received TPN and 5) all proportion of inpatients received antipyretics. All prescribed antibiotics (amoxicillin, clavulanic acid, cephradine, cefixime, ceftriaxone, clarithromycin, azithromycin) were statistically significant (p value >0.05). The chi-square value in all these antibiotics were in range from 8.674 to 5.457. During prospective study period, inpatients antibiotics were prescribed for diarrhoea, emesis, fever, abdominal cramps and bloating. 24% paeds patients received Augmentin, 9% paeds patients prescribed azithromycin, 14% received Cefixime, 19% received clarithromycin and 29% paeds patients received ceftriaxone.
key words
antibiotics, prospective study, chi-square analysis, anova, southern punjab region
Introduction
In present world, gastroenteritis (GE) is not a dangerous challenge to the developed countries with growing population of world. But in Pakistan from 1991-2011, the outburst of population is seen in 21st century, GE is becoming a challenge to be coped as its cases are increased a lot from 15% to 21% [1]. Gastroenteritis is actually the inflammation of stomach and intestines which includes infectious and noninfectious causes, presenting a sudden onset of diarrhea associated with or without vomiting [2]. Although GE is a self-limiting disease in the children but its course of illness is dramatically different in many children due to variety of factors such as side effects of medication, aperient use, chronic diseases that have diarrhea or vomiting as a symptom, fecal incontinence and food intolerance, unsanitary conditions of food and water in the community and epidemic of GE in that specific community area [3-5]. In different primary and secondary care hospitals, the control of infections is challenging due to improper health care facilities and unavailability of staff and medications [6,7]. In 2006-2007, huge outbreaks of GE were reported in all the zones of Pakistan exceeding 150% than the previous years due to poor hygienic conditions and unavailability of quality medicines [8]. The consequences of foodborne disease in these facilities were followed by other severe outbreaks of foodborne diseases in different zones of Pakistan. The burden of gastroenteritis is of significant importance both from the community perspective and in terms of use of healthcare resources [9].
In Pakistan current management and therapeutic guidelines for the management of acute GE is not properly working resulting in ineffective cure rates and increased cases of hospital admissions due to recurrent GE attacks or episodes requiring further research in this field to evaluate the causing factors as well as cost effective treatment according to the guidelines which will work properly in the scenario of Pakistan [10]. Guidelines must be the bridge between evidence-based knowledge and clinical practice and aim to reduce inappropriate variation in practice, improve the quality of care, increasing the efficiency in use of health care resources, as well as recommend novel treatments of proven efficacy[11]. The treatment regimens and guidelines for acute GE are continually changing and latest developed countries guidelines such as of National Institute for Health and Clinical Excellence [NICE] must be adopted which were published in 2009 to inform both clinicians and the public [12,13]. The clinical guideline for pediatric GE was also developed by a team of 13 healthcare workers and 2 lady members in Nishtar hospital Multan, Pakistan. Health economics was considered when recommending treatments so as to ensure a cost-effective use of resources by the team of health care workers still needing a lot to do in the perspective of managing the problem of acute GE in primary and secondary as well as tertiary care hospitals. The primary care hospitals are only dealing with the minor symptoms of GE and they provide initial basic line treatment. The secondary and tertiary health care units are responsible for providing detailed treatment of gastroenteritis including supportive treatment.
The present study was aimed at prospective study from Children Complex Hospital and Nishtar Hospital Multan survey to examine the general trends of malpractice of antibiotics prescription in Gastroenteritis pediatrics patients. Children of gastro-enteritis having ranges from 0 to 15 years are included in study while children suffering from other disease are not included in the study. During prospective study period, inpatients antibiotics were prescribed for diarrhoea, emesis, fever, abdominal cramps and bloating. 24% paeds patients received Augmentin, 9% paeds patients prescribed azithromycin, 14% received Cefixime, 19% received clarithromycin and 29% paeds patients received ceftriaxone. Study period consists of six months including sampling and collection of data.
Methods
Data sources
500 patients of Gestro-enteritis > 15 are included in the study 300 from children hospital and 200 from Nishtar Hospital Multan. Children suffering from other diseases along with Gestro-enteritis are not included in the study. Performa was developed for the collection of required information from Children as well as from the Patients. Bio data of Children Hospital, admission history and any history of surgical procedures were performed, history of tooth brushing and various other tests perform during stay in the hospitals.
Classification of patients’ visit
According to their ages, the patients were categorized into six groups: 1) Group 1 was ranged from 0 to 6 months, 2) Group 2 was ranged from 6 to 12 months, 3) Group 3 having ages ranged from 1 to 3 years, 4) Group 4 was ranged from 3 to 6 years, 5) group 5 ranged from 6 to 12 years and 6) Group 6 was < 12 years but > 15 years.
Antibiotics prescribed for gastro-entitis
Augmentin, Cepharadine, Cefixime, Ceftriaxone, Clarithromycin and Azithromycin.
Hospital indicators
Hospital indicators for prescribing patterns include various laboratory tests, previous history of patient regarding medicines, current complaints, patient physical condition, etc. Prescribing indicator, hospital indicator, patient care and supplemental indicators and prescribing pattern are closely related to each other. Mostly indicators are the various laboratory tests performed in hospital especially cultural sensitivity test for antibiotics. Other includes the previous medication history, patient lifestyle, duration of illness, patient complaints and present physical condition and appearance.
Analysis by questionnaire
Following provisions of informed consent, participants were administered a structured questionnaire that is designed to collect information on socio-demographic characteristics; Patient name, age and sex, Socio-economic status, History of Blood transfusion, History of admission to hospital (previous), Surgical procedure history, Family history of GE, History of drinking vehicles, History of dental surgery, Sharing of tooth brush, History of any complaints (Diarrhoea, Vomiting, Fever and Abdominal Cramps).
All surveys were questioner controlled utilizing PCs with Questionnaire Design System (QDS) Version 2.6.1 programming (Nova Research Company, Bethesda, MD, USA). Meetings kept going a middle of roughly 35 min (go: 17– 90 min).
Measures
Antibiotics prescription trends in: 1) 456 proportion of inpatients received antidiarrheal, 2) 387 proportion of inpatients received antiemetic, 3) 479 proportion of inpatients received antispasmodic,4) 289 proportion of inpatients received TPN and 5) all proportion of inpatients received antipyretics.
Statistical Analysis
The obtained data was analyzed by different statistical procedures. SPSS [14,15] was used to obtained the chi-square value and p value. Descriptive statistics and one-way ANOVA was used to obtained the data statistically significant at p vale (>0.05) [16].
Results
Patient data analysis
500 cases of children having gastroenteritis were selected for the study. 300 patients were selected from children hospital Multan and 200 patients from Nishtar hospital Multan, Pakistan.
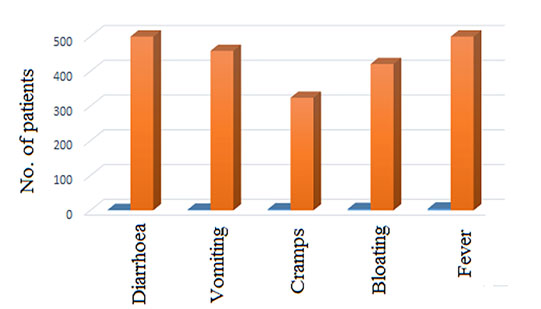
Symptoms of gastroenteritis in paeds
Gastroenteritis paeds patients present various symptoms like diarrhoea, vomiting, bloating, abdominal discomfort and fever. In case of improper treatment, a complication i.e. irritable bowel syndrome occurs in paeds that is characterized by irregular bowel habits and abdominal discomforts. Among 500 patients as in figure 1, diarrhoea and fever occur in all paeds patients while 459 patients present the complaints of vomiting, 324 patients showed abdominal cramps and bloating occur in 421 paeds patients.
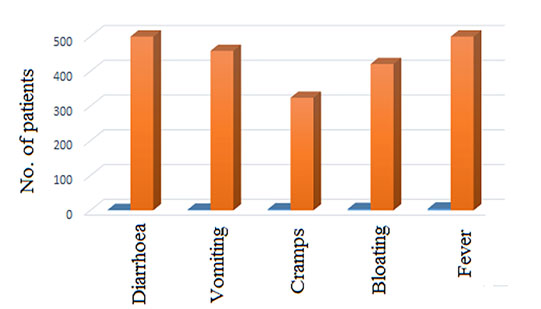
Figure 1. Symptoms of gastroenteritis occur in paeds patients.
Antibiotics prescribed for gastro-entitis
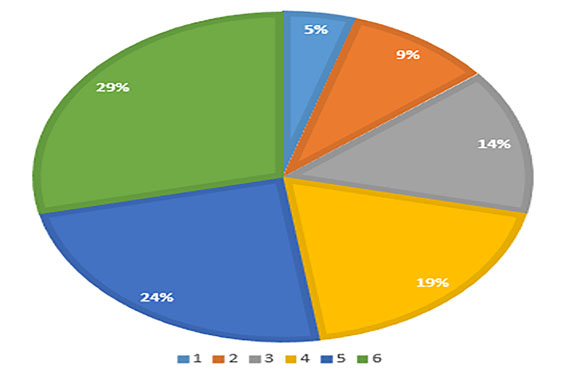
Augmentin was prescribed to the 134 paeds patients, 23 children received Cephradine while 89 patients received Cefixime, 139 patients prescribed ceftriaxone, 101 patients were prescribed to clarithromycin and 16 paeds received azithromycin. The frequency of prescription of Ceftriaxone was more as compared to other prescribed antibiotics and azithromycin was prescribed to the less number of paeds patients. In figure 2, 24% paeds patients received Augmentin, 9% paeds patients prescribed azithromycin, 14% received Cefixime, 19% received clarithromycin and 29% paeds patients received ceftriaxone. Maximum paeds patients received antibiotics from cephalosporins group such as ceftriaxone due to good spectra against many microorganisms. The high acceptability of cephalosporins is due to less side effects. Azithromycin was prescribed to less paeds patients; this is due to more side effects on paeds patients.
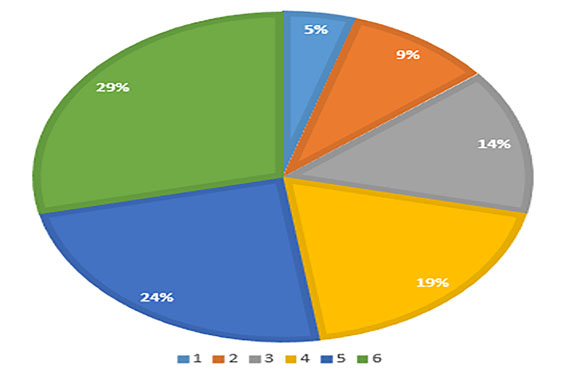
Figure 2. Percentages of patients receiving different antibiotics 1. Amoxicillin and clavulanic acid, 2. Cephradine, 3. Cefixime, 4. Ceftriaxone, 5. Clarithromycin and 6. Azithromycin.
Medicines prescribed for gastro-entitis
Antibiotics were administered to 500 paeds patients, 456 patients received antidiarrheal, 387 patients received antiemetic, 479 patients received antispasmodic, TPN was administered as supportive therapy to 289 patients and antipyretics were administered to all paeds patients that was selected for the prospective study. The most frequently used antipyretic was paracetamol and ibuprofen because these both effectively reduce the pyrexia in paeds patients. Dimenhydrinate was prescribed to control emesis and Buscopan brand was used to control abdominal cramps.
Statistical analysis
Analysis for symptoms of GE
Chi-square analysis of symptoms of GE was performed by using SPSS software. The chi-square values of diarrhoea, vomiting, abdominal cramps, bloating and fever were 9.876, 7.180, 8.346, 9.569 and 9.876 respectively that are statistical significant at p value >0.05. The descriptive statistics were performed on the symptoms of GE paeds patients as shown in table 1.
Table 1. Descriptive analysis of symptoms of GE in paeds patients.
S. No. | Parameters | Results |
Diarrhoea | Vomiting | Abdominal cramps | Fever |
1 | Mean | 0.575 | 0.786 | 0.456 | 0.432 |
2 | Standard deviation | 0.0913 | 0.0974 | 0.675 | 0.543 |
3 | Median | 0.5 | 0.6 | 0.4 | 0.4 |
4 | Mode | 0.5 | 0.6 | 0.4 | 0.4 |
5 | Skewness | 2.749 | 2.965 | 2.543 | 2.324 |
6 | Range | 2.6 | 3.4 | 1.9 | 1.8 |
7 | Minimum | 0.3 | 2.1 | 0.2 | 0.2 |
8 | Maximum | 2.3 | 4.0 | 1.0 | 0.9 |
Analysis for antibiotics
Chi-square analysis of antibiotics was performed by using SPSS software. The chi-square value of Augmentin, Cephradine, Cefixime, Ceftriaxone, Clarithromycin and Azithromycin were 7.456, 6.456, 8.674, 8.452, 5.457 and 6.435 respectively. All are statistically significant (p-value >0.05) except Azithromycin (p-value <0.05). The descriptive statistics were performed on the use of antibiotics in GE paeds patients as shown in table 2.
Table 2. Descriptive analysis of antibiotics used for the treatment of GE.
S. No. | Parameters | Results |
Penicillin’s | Cephalosporins | Macrolides | Others |
1 | Mean | 0.565 | 0.746 | 0.446 | 0.422 |
2 | Standard deviation | 0.0933 | 0.0904 | 0.685 | 0.503 |
3 | Median | 0.5 | 0.5 | 0.5 | 0.4 |
4 | Mode | 0.5 | 0.6 | 0.4 | 0.5 |
5 | Skewness | 2.709 | 2.945 | 2.533 | 2.304 |
6 | Range | 2.5 | 3.8 | 1.7 | 1.7 |
7 | Minimum | 0.2 | 2.2 | 0.1 | 0.3 |
8 | Maximum | 2.1 | 4.2 | 1.3 | 0.8 |
Analysis of prescribed medicines other than antibiotics
Chi-square analysis of anti-emetics, anti-motility and anti-protozole was performed by using SPSS software. The chi-square values of bismuth sub-salicylate, Loperamide, Dimenhydrinate, Metoclopramide, Domperidone, Metronidazole, Tinidazole and Diloxanide furoate were 9.076, 7.480, 8.246, 9.769, 9.576, 8.352, 5.257 and 6.235 respectively. All are statistically significant at p-value >0.05.
Discussion
One-way ANOVA was applied on the data obtained from two hospitals (Children complex hospital and Nishter hospital), Multan, Punjab, Pakistan in order to confirm the significance of data. In ANOVA, the P-value was less than 0.05 which indicate the significance of data.
500 cases of children having gastroenteritis were selected for the study. 300 patients were selected from children hospital Multan and 200 patients from Nishtar hospital Multan, Pakistan. According to their ages the patients that are participated in the study were categorized into six groups. The age of group 1 was ranged from 0 to 6 months, group 2 was ranged from 6 to 12 months, group 3 having ages ranged from 1 to 3 years, group 4 was ranged from 3 to 6 years, patients of group 5 ranged from 6 to 12 years and age of patients of group 6 was greater than 12 years but less than 15. Multan and its surrounding areas are more contaminated due to less focus on hygienic conditions, due to this poor hygienic conditions many diseases are spreading day by day. Paeds having age in between 0 to 6 months are more suffered to disease as compared to the other age groups, this is because of less development of immune system. Gastroenteritis paeds patients presents various symptoms such as diarrhea, vomiting, bloating, abdominal discomfort and fever. In case of improper treatment, a complication i.e. irritable bowel syndrome occurs in paeds. The irritable bowel syndrome is characterized by irregular bowel habits and abdominal discomforts as reported previsoluy [17-19]. Antibiotics were administered to 500 paeds patients, 456 patients received antidiarrheal, antiemetic was given to 387 patients, 479 patients received antispasmodic, TPN was administered to 289 patients and for the control of fever antipyretics was administered to all paeds patients that was selected for the study. Similar findings already previously published [20,21].
Augmentin was prescribed to the 134 paeds patients. From cephalosporin group 23 children received Cephradine while 89 patients received Cefixime and 139 patients prescribed ceftriaxone. 101 patients were prescribed to the macrolide group clarithromycin and 16 paeds received azithromycin. 24% paeds patients received Augmentin, 9% paeds patients prescribed azithromycin, 14% received Cefixime, Clarithromycin was prescribed to the 19% paeds and 29% paeds patients received ceftriaxone. These findings are supported by reported previously[22,23]. Maximum paeds patients received antibiotics from cephalosporins group such as ceftriaxone due to good spectra against many microorganisms. It was observed from the prescription and diagnostic test the antibiotics was prescribed by two ways. 198 children from children hospital and 39 from Nishtar hospital Multan received antibiotics after performing culture sensitivity test but remaining children received antibiotics without performing culture sensitivity test. 40% paeds patients from children hospital received antibiotics after culture sensitivity test and 10% from Nishtar hospital Multan. 20% from Children hospital and 30% from Nishtar hospital Multan received antibiotics without performing culture sensitivity test. The supportive therapy was also provided the paeds GE patients in order to prevent from dehydration. During GE diarrhea and vomiting are frequently occurring, this cause dehydration. Total parenteral nutrition (TPN) and oral rehydration salt (ORS) are most commonly used in paeds patients. 123 paeds patients received TPN while 323 patients received ORS for the prevention of dehydration. All these findings supported by reported previously [24,25].
Conclusion
During prospective study period, inpatients antibiotics were prescribed for diarrhoea, emesis, fever, abdominal cramps and bloating. 24% paeds patients received Augmentin, 9% paeds patients prescribed azithromycin, 14% received Cefixime, 19% received clarithromycin and 29% paeds patients received ceftriaxone.
Acknowledgement
The all authors hereby have acknowledged to staff members of Nishter Hospital and Childern Complex Hospital, Multan.
Compliance with ethcal statements
Informed consent
Authors declared, the permission has taken from hospitals for this survey.
Contribution of co-authors
Syed Nisar Hussain Shah: Research supervisor
Muhammad Yousaf: Doing research study
Hina Javed: Assist in research work
Imran Qureshi: Help in data collection
Naveed Nisar: Help in data collection
References
- Hall GV, Kirk MD, Ashbolt R, Stafford R, Lalor K (2006) Frequency of infectious gastrointestinal illness in Australia, 2002: regional, seasonal and demographic variation. Epidemiol Infect 134: 111-118. [Crossref]
- Ahmed SM, Hall AJ, Robinson AE, Verhoef L, Premkumar P, et al. (2014) Global prevalence of norovirus in cases of gastroenteritis: a systematic review and meta-analysis. Lancet Infect Dis 14: 725-730. [Crossref]
- Clark B, McKendrick M (2004) A review of viral gastroenteritis. Curr Opin Infect Dis 17: 461-469. [Crossref]
- Russo TA, Johnson JR (2003) Medical and economic impact of extraintestinal infections due to Escherichia coli: focus on an increasingly important endemic problem. Microbes Infect 5: 449-456. [Crossref]
- Khan S, Orenstein SR (2002) Eosinophilic gastroenteritis. Pediatric Drugs 4: 563-570. [Crossref]
- Curns AT, Steiner CA, Barrett M, Hunter K, Wilson E, et al. (2010) Reduction in acute gastroenteritis hospitalizations among US children after introduction of rotavirus vaccine: analysis of hospital discharge data from 18 US states. J Infect Dis 201: 1617-1624. [Crossref]
- Leshem E, Tate JE, Steiner CA, Curns AT, Lopman BA, et al. (2015) Acute gastroenteritis hospitalizations among US children following implementation of the rotavirus vaccine. JAMA 313: 2282-2284. [Crossref]
- Inouye S, Yamashita K, Yamadera S, Yoshikawa M, Kato N, et al. (2000) Surveillance of viral gastroenteritis in Japan: Pediatric cases and outbreak incidents. J Infect Dis 181: S270-S274. [Crossref]
- Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, et al. (2010) The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis 50: 882-889. [Crossref]
- King CK, Glass R, Bresee JS, Duggan C, (2003) Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep 52: 1-16. [Crossref]
- Paulke-Korinek M, Rendi-Wagner P, Kundi M, Kronik R, Kollaritsch H (2010) Universal mass vaccination against rotavirus gastroenteritis: impact on hospitalization rates in Austrian children. Pediatr Infect Dis J 29: 319-323. [Crossref]
- Cortese MM, Parashar UD (2009) Prevention of rotavirus gastroenteritis among infants and children: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 58: 1-25. [Crossref]
- Parashar, Alexander JP, Glass RI (2006) Prevention of rotavirus gastroenteritis among infants and children. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 55: 1-13. [Crossref]
- Allison PD (2002) Missing data: Quantitative applications in the social sciences. British Journal of Mathematical and Statistical Psychology 55: 193-196.
- Stevens JP (2012) Applied multivariate statistics for the social sciences. Routledge
- Peat J, Barton B (2008) Medical statistics: A guide to data analysis and critical appraisal. John Wiley & Sons
- Roslund G, Hepps TS, McQuillen KK (2008) The role of oral ondansetron in children with vomiting as a result of acute gastritis/gastroenteritis who have failed oral rehydration therapy: a randomized controlled trial. Ann Emerg Med 52: 22-29. [Crossref]
- Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR (1990) Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut 31: 54-58. [Crossref]
- Gonzalez-GalanVA, Sánchez-Fauqier, Obando I, Montero V, Fernandez M et al. (2011) High prevalence of community-acquired norovirus gastroenteritis among hospitalized children: a prospective study. Clinical Microbiology and Infection 17: 1895-1899.
- Jenkins HR, Ansari BM (1990) Management of gastroenteritis. Arch Dis Child 65: 939-941. [Crossref]
- Bhaveshaikh N, Sukumaran S, Vyas U (2017) Drug prescribing pattern in acute gastroenteritis in an in-patient setting in a private hospital. International Journal of Research in Medical Sciences 5: 1256-1259.
- Özmert EN1, Ince OT, Örün E, Yalçin S, Yurdakök K, et al. (2011) Clinical characteristics and antibiotic resistance of Shigella gastroenteritis in Ankara, Turkey between 2003 and 2009, and comparison with previous reports. Int J Infect Dis 15: 849- 853. [Crossref]
- Key J (2015) A novel approach to the rehydration of children with gastroenteritis in the emergency department. Auckland University of Technology.
- BoraAkoglu, Alexander Loytved, Hannah Nuiding, StefanZeuzem, DominikFaust (2015) Probiotic Lactobacillus casei Shirota improves kidney function, inflammation and bowel movements in hospitalized patients with acute gastroenteritis–A prospective study. Journal of Functional Foods 17: 305-313.
- Hung YT, Lay CJ, Wang CL, Koo M (2017) Characteristics of nontyphoidal Salmonella gastroenteritis in Taiwanese children: A 9-year period retrospective medical record review. J Infect Public Health 2017. [Crossref]