Abstract
Background: The wettability of the oral cavity reduces the symptoms of obstructive sleep apnea (OSA).
Objective: The modification of OSA symptoms in adults using an artificial saliva (AS).
Methods: Open registry study on 60 males suffering from a mild form of OSA.The cases followed a Standard Managenent (SM) consisting mainly of diet and exercise, freely chosing between 2.5 g gel of artificial saliva (SM+AS) or water gel (SM+WG) given twice/day for a period of 4 weeks. One week of run in was requested before any treatment to train subjects and housepartners to measure xerostomia at night and snoring (main variables) together with other OSA symptoms (falling asleep during the day, fatigue, awakness with breath holding, gasping/choking, total OSA score) using ordinal scales.
Results: SM+AS reduced xerostomia at night, snoring and the total OSA score in the respective percentages of 80, 63, 60 %, whereas with SM+WG the reduction was limited to 8, 39, 11 % (p< 0.05 for every symptom). Body weight was minimally modified in both groups.
Conclusion: In patients with mild OSA, SM+AS reduces many symptoms, particularly, xerostomia at night, snoring and the total OSA score.
Key words
standard management obstructive sleep apnea, xerostomia, snoring, OSA symptoms, artificial saliva, Aldiamed®
Introduction
Obstructive sleep apnea (OSA) is classified as 780-53 according to ICD-9-CM as part of the sleep-related breathing disorders (SRBD) which are essentially a disease continuum ranging from primary snoring (PS) at one end to obstructive sleep apnea (OSA) [1,2,3]. OSA is a syndrome which is basically due to a respiratory control instability causing a reduction of upper airways dilator muscles and by a propensity to arouse from sleep due to the increase of CO2 concentration in blood; however, the real pathophysiological reasons for these modifications is not well defined [2].
Among the OSA symptoms, xerostomia -following arousal from sleep- and snoring are costant features.Xerostomia is a consequence of snoring which has to be considered the real trigger.
Snoring is characterized by loud upper-airways breathing sounds produced in the nasopharynx during sleep. Abitual snoring is a common and early symptom of OSA caused by the flutter of soft tissue of the nasopharynx - particularly the soft palate- and depends upon interating factors related to the muscular relaxation. If pharyngeal dilators cannot keep the airway open in response to the negative intraluminal pressure induced by inspiration, the upper way narrows, increasing local airflow velocity. The increased flow modify the intraluminal pressure thus enhancing the flutter and snoring as it may happen frequently in overweight people - were the fat it deposited within the tongue- which colud impaire function of genioglosse muscle [4].
Accoring to different authors, snoring may range from 57 % of man and of women 40 [2,5] down to the 33 % of the general population [6] and the presence of OSA in these subjects should be suspected, and determined by polysomnographic monitoring.
One of the tentative treatments of OSA can be a Standard Management (SM) consisting of physical exercise and a regular low calorie diet. The exercise training was found effective on OSA [7] either as such or in relation to the reduction of the energy intake [8], even without the need of using the continuous positive air pressure (CPAP) [9]. The body weight (BW) reduction can also improve the OSA symptoms, even though it is very difficult to keep the patients on a diet for long period of time.
SM is based on a diet program which is not imposed to the patients and is freely discussed and agreed upon with them.
In this way the limitation of food intake (-10 % of daily calorie intake) together with the increase of physical activity (9 MET-h/week) seems to be affordable at long term since in one year it was possible to obtain an average BW reduction of about 0.6 Kg/month (8 kg/year) [10].
A part of diet and exercise, the SM suggests also to improve the oral hygiene. This last aspect, particularly the moisturing of the oral cavity surpisingly was limiting the OSA symptoms in children [11].
An artificial saliva (AS; aldiamed® mouth gel) containing Aloe vera was found very effective in vitro considering the wetting and permanence on materials similar to the oral tissue [12], and also for the activity against the Candida albicans [13]. The product is a medical device of common use.
The present study was an open observational Registry addressed to adults suffering from a mild form of OSA that were following a SM in combination with an artificial saliva (AS) or a water gel (WG). The experience was aimed to compare AS versus WG following a period of 4 weeks of treatment. The limited period of time was chosen to minimize the effect of BW reduction -which is expected during SM- and is known to improve the OSA symptoms.
Material and methods
The study was conducted at a single centre. It was designed and implemented according to UNI EN ISO 14155:2012 and to the STROBE checklist [Strobe statement Version 4 as published in Oct/Nov 2007] in conformity with the guidelines of the Declaration of Helsinki.
The type of experience was a supplement Registry study on SM, comparing an artificial saliva gel (Aldiamed®) and a water gel (Resource®orange taste) given for a period of 4 weeks.
Sixty males 35-55 years old followed for asyptomatic vascular diseases in a population screening progam were evaluated.
The observational experience was conducted between the months of September to December 2017.
Admission criteria. Subjects at the initial stage of OSA [1-3] presenting snoring and xerostomia at night leading to the desire of drinking water. For these subjects, symptoms were mild and the presence of severe form of OSA was previously excluded by a polysommnographic testing done not later than six months before the experience. As admission criteria the OSA severity was determined using ordinal scales and only patients with scores ≤ 3 (see Table 1) were entering the study.
Table 1. Ordinal scales; scoring details of some of the OSA variables
|
Scores
|
Symptoms
|
|
Falling asleep
during the day
|
Fatigue
|
Awakening with
breath holding
|
Gasping or
choking
|
|
0
|
No
|
No
|
No
|
No
|
|
0.5
|
1 time
|
Just a feeling sometimes
|
1 episode at night
|
1 episode at night
|
|
1
|
up to 2 times/day
|
Minimal, no need of rest
|
Up to 2 episodes
[during the night]
|
Up 2 episodes
[during the night or the day rest]
|
|
1.5
|
3-4 times/day
|
1 rest/day
|
Up to 3 episodes
[during any rest]
|
Up to 3 episodes
[during any rest]
|
|
2
|
5-6 times/day
|
2 rests/day]
|
4-5 episodes
[during any rest]
|
4-5 episodes
[during any rest]
|
|
2.5
|
7- 8 times/day
|
3-4 rests/day
|
6-7 episodes
[during any rest]
|
6-7 episodes
[during any rest]
|
|
3
|
9-10 times/day
|
5-6 rests/day
|
8-9 episodes
[during any rest]
|
8-9 episodes
[during any rest]
|
|
3.5
|
11-12 times/day
|
6-8 rest/day
|
10-12 episodes
[during any rest]
|
10-12 episodes
[during any rest]
|
|
4
|
˃ 12 times/day
|
˃ 12 rest/day
[with difficulties in
performing daily activities]
|
˃ 12 episodes
[during any rest]
|
˃ 12 episodes
[during any rest]
|
Patients had to be familiar with the Food Intake Questionnaire [10] because they were part of the screening program for the asymptomatic vascular disease [14] using FIA (for food intake control) and following a SM.
The participation of a partner collaborating with the patient was among the admission criteria.
Exclusion criteria
Patients with any symptom of OSA scoring > 3 were excluded.
Significant nasal septal deviation, rhinitis, micrognathia or retrognathia, enlarged tonsils, BMI > 35 kg/m2, use of drugs or supplements for body weight control, chronic disorders, any type cancer, aloholism, drug addiction, use of hypnotic, anxiolitics and antipsycothic drugs.
Timetable
The timetable consisted of three periods as follows:
run in (one week with measures recorded every day), baseline (one week with measures recorded in the last day of the week); after 4 weeks of treatment (one week with measures recorded in the last day of the week.
Variables
The main variables were xerostomia at night and snoring.
Xerostomia in particular was driving the entire experience since it was used to determine the sample size (see later). It was measured according to the dicotomy -yes or no- which was considered an extremely severe, much more than the simple reduction of the number of times of its manifestation during the night.
Snoring also was considered as a main variable due to its direct connection with xerostomia.
Other secondary variables were consistent with a mild OSA diagnosis and were the following: daytime sleepiness (determined by the partner); falling asleep during the day (determined by the partner); fatigue (determined by the patient); awakening with breath holding (determined by the patient and by the partner); gasping or choking (determined by the partner); total OSA score; body weight, BMI. All the OSA symptoms were measured using scores based on ordinal scales.
The total OSA score consisted of the sum of the symptom scores.
Snoring was the only variable measured every day for 7-day periods. All the other variables were taken for 7 days during the run in only, whereas at baseline and after 4 weeks of treatment values were taken only in the last day of the week.
Snoring ordinal scale
The snoring was the most frequent measure since it was taken for 21 days: every day during the 7- day run in, for 7 days in the baseline evaluation, and finally for 7 days in the 4th week.
Snoring was determined by the partner according to the following ordinal scale based on the severity criteria reported by American Academy of Sleep Medicine [14]:
-Occasional; snoring occurring sometimes (maximum 2 times/week) and only in supine position.
-Mild; snoring occurring less than nightly (maximum 5 times/week) and only when the patient was in the supine position
-Moderate; snoring occurring nightly, occasionally disturbing others, and was usually abolished by change in body position
-Severe; snoring occurring nightly, disturbing others, and not altered by change in body position. Bedpartners may have to sleep in another room due to the loudness of the snoring.
Other OSA variables
The following symptoms of OSA were recorded: falling asleep during the day, fatigue, awakness with breath holding, gasping/choking, total score. They were taken during the day and/or night by the subject and/or the partners using an ordinal scale from 0 to 4. Four variables were measured as reported in Table 1, and the total OSA score was the sum of the symptoms score.
Run-in period
The run-in period consisted of seven days; each day the OSA symptoms were measured. This period was considered as a training for the patients and the partner to get them familiar with the ordinal scales. A clear explanation was given by the investigators to the participants on how to fill up the scales. In case some of the symptoms was not measured correctly, the patient was not enrolled, or the enrollment was postponed until the measures were taken properly. For every symptom, values up to 3 were arbitrarily considered as mild. The patient was not admitted to the trial In case of any symptom ˃ 3 (Table 1).
Standard Management (SM)
The details of the Standard Management for OSA are reported in the following Table 2.
Table 2. Standard Management of OSA: variables, measures and some detail
|
Variable
|
Measures
|
Details
|
|
Food intake
|
FIA (Food intake Assessment Questionnaire [9]
|
25 servings type; frequency during the week
|
|
Calorie intake
|
-10 %/day [9]
|
7-day questionnaire; no drastic modification of the diet
|
|
Food limitation
|
No coffe and soda beverages
|
No food in the 2 hours before night sleeping
|
|
Physical exercise
|
9 MET-h/week [9]
|
1 h of breasky walking/day : three 20 minutes periods
|
|
Sleeping time
|
-
|
No matter which time diuring the day, provided in the same hour of the day and evening
|
|
Sleeping position
|
-
|
Possibly avoid the supine position
|
|
Hydration
|
2 L/day
|
No matter about the time of the intake
|
|
Oral hygiene
|
|
Use of tooth paste and moisturing products twice/day
|
|
Pillow
|
standard
|
Given by the centre
|
One important point was the method to control food intake using FIA (Food Intake Assessment). The FIA consisted of 25 different type of servings composed by the most common 250 Italian foods [10]. Some suggestion was given to participants to prepare servings with reducing pasta and increasing vegetables or pulses, to use more eggs to reduce cheese and processed meat. Furthermore, indications were given to cut the 850 kcal of pizza (taking out the crust), to limit the chips, and substitute hard drinks with beverages with less alcoholic content (e.c.marsala, mirto, limoncello).
Subjects were suggested to increase physical activity of about 9 MET-h/week by brisky walking divided into periods of 20 min (Table 2).
The oral hygiene was considered very important with the aim to increase the wettability of the oral cavity and indirectly the oral cavity muscles performance.
A standard pillow (given by the centre) was used by all subjects and bed conditions and positions were revised with the subjects.
Products under testing
Together with SM two comparative products were proposed; an AS gel (aldiamed®) or WG (Resource®orange taste ) to be given twice/day at 2 pm and immediately before bed time, both in the amount of 2.5 g/administration (about a tea spoon) to be spread in to the mout using the finger or rolling the gel in the mouth with the tongue. After careful briefing and testing, subjects were deciding which of the product they were using. For most of the cases the choice was determined mainly by the taste. Each subject was given the product to use in the amount necessary for 4 weeks (two AS gel and four WG paks). The products were asked to be kept at 4Co.
Compliance
The compliance for the product was measured calculating the difference in the weight of the tubes of AS of the plastic glass of WG residuals after the 4-week treatment. For SM the compliance was not measured.
Other informations
Side effects were communicate by SMS, and all results of the evaluation were also comunicated via cell phone. The record forms were filled up by patient/partners and controlled by the one of the investigators that was not aware about the type of treatment (AS or GW)
Statistical analysis
Sample size: The sample size was calculated on the base of xerostomia, which usually is present in 100 % of the cases. The hypothesis was that AS could reduce the symptoms in > 50 % of the cases. Considering a 1-β = 90 and an α value of 0.05, the number of 20 cases/group will be sufficient to discriminate the different activity of the products.
Since there was no knowledge a priori about the compliance, the decision was to increase by 30 % the number of participants. On the whole 30 cases/group were enrolled for a total of 60 subjects.
Data analysis: Each variable was calculated as such (e.c. age, body weight) or using scores (ordinal scales, see later) and the frequency. The average OSA scores and the standard deviation were calculated; the values before and after the treatments were compared using the t test (independent data) or the Tukey test (interdependent data). For the frequencies the chi square with Yates correction was applied or the Fisher test (exact chi square) in case of low frequencies (between 0 to 5).
Total scores values of the two groups were analyzed using the t test for independent data.
Blindness: One of the investigators only was aware of the treatment and was not involved in the control of the record forms. The statistician was not aware of the treatments and received the data in an exel file were treatment were indicated only as A and B.
Results
Seventyfive subjects were interviewed, and 60 were included into te registry. Fifteen subjects were excluded because the run-in questionnaire was unreliable. These last subjects or the partners found the evaluation to complex (14 couples); one subject was excluded because the BMI was > 35 Kg/m2 (see Figure 1). Fiftyeight cases complete the 4-week registry period; no complains were reported about the therapies. Two case of the SM+WG group did not come to the final evaluation for working problems (Figure 1).
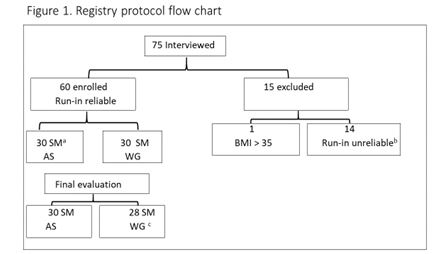
Figure1.Registry protocol flow chart.
a SM = Standard Management; b incomplete evaluation of the run in items; c lack of the final evaluation in two cases
AS = artificial saliva; WG = water gel
The compliance was excelent since the quantity of gel consumed for both treatments was almost identical to the theoretical measure.
The general characteristic of the patient are reported in Table 3 and no significant difference was found between the two groups (p > 0.05). The overweight subjects frequency (BMI > 25 Kg/m2< 35 Kg/m2 ) was almost identical in the two groups (Table 3). Snoring scores values are reported in Table 4.
Table 3. General characteristics of the subjects: Mean ± SD or frequency
|
Variables
|
MS+AS
|
MS+WG
|
t
test
|
Chi square
|
p
|
|
Age
|
47.8 ± 4.19
|
46.5 ± 3.47
|
0.22
|
-
|
> 0.05
|
|
Cases
|
30
|
28
|
|
-
|
|
|
BMI > 25 <30
|
22
|
20
|
|
0.0174
|
> 0.05
|
|
BMI > 30 < 35
|
8
|
8
|
|
0.0286
|
> 0.05
|
Table 4. Snoring score before and after 4 weeks of treatment: number of cases and chi square values [3]
|
Snoring score
|
SM+AS
|
SM+WG
|
Chi square
|
|
Baseline
|
4 weeks
|
Baseline
|
4 weeks
|
Baseline
SM+AS Vs SM+WG
|
4 weeks
SM+AS Vs SM+WG
|
|
Occasional
|
4
|
1
|
5
|
1
|
0,4543a
|
0.5085a
|
|
Mild
|
7
|
2
|
3
|
2
|
0.1787a
|
0.6675a
|
|
Moderate
|
8
|
3
|
8
|
5
|
0.0174b; p > 0,05
|
0.3138a
|
|
Severe
|
11
|
5
|
12
|
9
|
0.0454b; p > 0.05
|
1.1434b; p> 0.05
|
|
Total
|
30
|
11
|
28
|
17
|
|
|
|
Number of improved
|
|
19 [63%]
|
|
11[39%]
|
4.386b ; p < 0.05
|
|
|
Number of impaired
|
|
0
|
|
0
|
|
|
a Fisher exact chi square test; bChi square with Yates correction
The two groups at baseline were comparable (chi square with Yates correction or Fisher exact chi square test p > 0.05). After 4 weeks of treatment the reduction of snoring scores were also similar (p < 0,05). However, considering the total number of patiens improved, the treatment with SM+AS was significantly more effective (p< 0.05) reducing the snoring score in about 63 % of cases compared to 39 % in the MS+WG group.
For what concerms the other OSA symptoms, the data matrix containing the number of patients with the relative scores and the total scores were summarized in the Table 5.
Table 5. Symptoms of OSA: score values matrix, total score, xerostomia at night, body weight (mean ± SD) at baseline and after 4 weeks of treatment
|
Symptoms
|
Baseline SM+AS
scores
|
Total
score
|
After 4 weeks SM+WG
scores
|
Total score
|
|
0
|
0.5
|
1.0
|
1.5
|
2.0
|
2.5
|
3.0
|
9.8
±
0.84
|
0
|
0.5
|
1.0
|
1.5
|
2.0
|
2,5
|
3.0
|
3.9ab
±
0.39
|
|
Daytime sleepiness
|
|
|
|
|
21
|
9
|
|
|
5
|
19
|
6
|
|
|
|
|
Falling asleep during the day
|
|
|
24
|
3
|
3
|
|
|
3
|
27
|
|
|
|
|
|
|
Fatigue
|
|
|
|
|
16
|
6
|
8
|
|
|
15
|
15
|
|
|
|
|
Awakening with breath holding
|
|
|
|
|
2
|
23
|
5
|
2
|
23
|
5
|
|
|
|
|
|
Gasping or choking
|
|
|
1
|
22
|
7
|
|
|
|
20
|
10
|
|
|
|
|
|
Total
|
0
|
0
|
25
|
25
|
49
|
38
|
13
|
Χ2a
|
5
|
75
|
2021 Copyright OAT. All rights reserv
49
|
21
|
0
|
0
|
0
|
Χ2b
|
|
Xerostomia at night
|
25/30
|
|
5/30c
|
|
|
Body weight [Kg]
|
82.4 ± 7.76
|
81.8 ± 7.52a
|
|
|
Baseline SM+WG
scores
|
Total score
|
After 4 weeks SM+WG
scores
|
Total score
|
|
|
0
|
0.5
|
1.0
|
1.5
|
2.0
|
2.5
|
3.0
|
9.6
±
0.51
|
0
|
0.5
|
1.0
|
1.5
|
2.0
|
2,5
|
3.0
|
8.5a
±
0.50
|
|
Daytime sleepiness
|
|
|
|
1
|
17
|
10
|
|
|
|
|
1
|
15
|
12
|
|
|
Falling asleep during the day
|
|
|
11
|
17
|
|
|
|
|
|
18
|
10
|
|
|
|
|
Fatigue
|
|
|
|
|
14
|
14
|
|
|
|
1
|
1
|
25
|
1
|
|
|
Awakening with breath holding
|
|
|
|
|
5
|
22
|
1
|
|
|
|
|
19
|
9
|
|
|
Gasping or choking
|
|
|
4
|
23
|
1
|
|
|
|
1
|
25
|
2
|
|
|
|
|
Total
|
0
|
0
|
15
|
41
|
37
|
46
|
1
|
Χ2a
|
0
|
1
|
44
|
14
|
59
|
22
|
0
|
Χ2 b
|
|
Xerostomia at night
|
24/28
|
|
22/28
|
|
|
Body weight [Kg]
|
83.0 ± 7.26
|
82.3 ± 6.34a
|
a Tukey test; p < 0.01 Vs baseline; b t test p<0.01 SM+AS, Vs SM+WG; c SM+AS Vs SM+WG, Fisher exact chi square = < 0.0001;
Χ2a chi square = 0.0022 p> 0,05; Χ2 b chi square 85.282 p < 0.001
In terms of total score, the values were quite similar in the two groups (t test p> 0.05). After 4 weeks of treatment the differences between the two groups were definitely in favor of SM+AS (t test p< 0.05) that ended up with -60 % compared to the baseline data.
Similarly, the scores frequency at baseline were not significantly different (Χ2a = 0.0022; p <0.05), whereas after the treatment the shift towards the lowest scores was much more consistent with SM+AS (Χ2b = 85.282; p< 0.001) confirming the results of the total score.
The xerostomia during the night was reduced in 20 out of 25 cases, whereas in the group SM+WG the reduction was found in 2 out of 24 cases (Fisher exact chi square < 0.0001).
The BW modification was similar in both groups, and despite the difference compared to baseline values were minimal (less than 1 kg) they were statistically significant (Tukey test p < 0.01) (Table 5).
The xerostomia during the nigh was similar in the two groups at baseline (p > 0.05; chi square with Yates correction) and after 4 weeks of treatment it remained similar to the baseline value in the group SM+WG, whereas in the group SM+AS it was drastically reduced (Fisher test p< 0.0001.
For each symptoms the percentage reduction was calculated using the mean values or the frequency after 4 weeks of treatment compared to the baseline values. These data are reported in Table 6.
Table 6. Mean value and range of the OSA variables; percentages of improvement of each variable after 4 weeks of treatment
|
Symptoms
|
SM+AS
|
SM+WG
|
|
Baseline
|
4 weeks
|
R %a
|
Baseline
|
4 weeks
|
R %a
|
|
Daytime sleepiness
|
2.2 [2.0-2.5]
|
1.0 [0.5-1.5]
|
55
|
2.2 [1.5-2.5]
|
2.2 [1.5-2.5]
|
0
|
|
Falling asleep during the day
|
1.2 [1.0-1.5]
|
0.4 [0.0-0.5]
|
66
|
1.3 [1.0-1.5]
|
1.2 [1.0-1.5]
|
8
|
|
Fatigue
|
2.4 [2.0-3.0]
|
1.3 [1.0-1.5]
|
46
|
2.3 [2.0-2.5]
|
2.0 [1.5-2.5]
|
13
|
|
Awakening with breath holding
|
2.6 [2.0-3.0]
|
0.6 [0.0-1.0]
|
77
|
2.4 [2.0-3.0]
|
2.2 [2.0-2.5]
|
8
|
|
Gasping or choking
|
1.6 [1.0-2.0]
|
0.7 [0.5-1.0]
|
55
|
1.4 [1.0-2.0]
|
1.0 [0.5-1.5]
|
28
|
|
Total score
|
9.8 ± 0.84
|
3.9 ± 0.39
|
60
|
9.6 ± 0.51
|
8.5 ± 0.50
|
11
|
|
Xerostomia at night
|
25/30
|
5/30
|
80
|
24/28
|
22/28
|
8
|
|
Body weight [Kg]
|
82.4 ± 7.76
|
81.8 ± 7.52b
|
0.7
|
83.0 ± 7.26
|
82.3 ± 6.34b
|
0.9
|
a R %= percentage reduction of the mean Baseline values b Tukey test; p < 0.01 Vs baseline
In the the group SM+WG the percentage modificiations were limited to gasping/choking and fatigue (respectively -28 % and -13 %) since for the other OSA symptom the mean decrease was inconsistent (the total score reduction was only -11 %).
Instead, with the combination of SM+AS all the symptoms were favorably modified. A part of the BW the percentage reduction were ranging between -46 % (fatigue) and -80 % (xerostomia at night) consistent with the total score modification of-60 %.
Discussion
This study has some limitation that are typical of an observational Registry, as the lack of treatment with placebo and the blindness.
The placebo group was subtituted by the use of WG, and for the blindness the only measure adopted was that the investigators analyzing the cases were not aware of the type of treatment., The clinical record form filled up by the couple patient/partner were reporting only treatment A or B. Furtermore, to minimize the bias the expected reduction of main symptoms was settled to the 50 % of the cases. The need of the patient’s partner represents another limitation since the registry inclusion was possible only for people able to manage the symptoms according to the ordinal scales. This aspect was discriminant, since some 20 % of the cases (the couples patient/partner) were not capable to fit correctly the measures.
However, the cases analyzed in this study belong to a long term study on vascular diseases based on > 800 patients, that are followed since many years. Because of this, they are very well known by all the investigators and considered very reliable in the symptom reporting.
Despite this, the need of applying ordinal scales, scores or dicotomic variables still remain a limitation due to the relative lack of precision/sensitivity of the measures that were not validated. Furthermore, the differential efficacy of a treatment for a given symptom has to be taken with prudence since it may depends on the “feathering” between the symptom and the scale.
However, despite all these limitations the information deriving from the study were quite interesting.
The first observation is concerning the improvement shown in the group SM+WG. This finding was expected, because of the physical activity increase and the calorie reduction. The effect of physical exercise on OSA was alredy described even with minimal body weight change [7], and may futher improve once a more consistent body weight reduction will be achieved [16].
In other terms, the SM per se showed some effect despite the relative short period of treatment. However, as already mentioned, the short period of SM treatment was purposely adopted to allow the expression of the AS activity that was the real objective of this research.
Coming to the main variables, the xerostomia was reduced more efficiently in the SM+AS group compared to SM+WG (respectively -80% vs -8%) and represents the largest difference between treatments. This finding is understandable, because the use of the 2.5 ml of GW do not have the capability of wetting the pharinx for the entire night, whereas the AS had much longer permanence.
For what concerns snoring one may observe that the reduction in the SM+AS group was much more consistent than in the SM+WG (respectively -63 % Vs- 36 %) and stands for a real benefit of the use of the AS.
For the other OSA symptoms reported as total score, the average distance between the two groups was minimal at baseline (9.8 for SM+AS and 9.6 for SM+WG) but after 4 weeks the distance between the two treatments become extremely large (3.9 for SM+AS and 8.5 for SM+WG).
Despite they were only ancillary variables, their modification in the group SM+AS may give some information. The first is that all the symptoms were present in every patient and the expected reduction in 50 % of the cases was achieved: this means that the sample size was fitting also these variables.
Considering separately each single symptom, the differences were also quite consistent since in the SM+WG group the reductions were between 0 % (daytime slipiness) to -28 % (gasping and choking), instead in the group SM+AS the reduction were between -46 % (fatigue) and -77 % ( awakening with breath holding). In general the symptoms reduction seen in the SM+AS group were very consistent, close or more than -50 %. This aspect open a vindow on the activity of AS also to the ancillary symptoms. Particularly interesting was the falling asleep during the day, reaching -66 % in the group SM+AS compared to only -8 % for SM+WG.
Considering in general the results, the hypothesis is that AS consents a more relaxing and continuous sleeping, due to the xerostomia/snoring reduction followed also by the other OSA symptoms improvement, such as the fatigue and falling asleep during the following day.
These findinds open a window on OSA underlining the importance of the relationship between local condition in the oral cavity and the central respiratory system driving the upper airways dilator muscles. At the end, it seems that the condition of oral wettability may have an impact on the oxigen saturation decrease that is a characteristic of OSA.
The data of the present study are a confirmation of what has been described in children suffering from Down syndrome and OSA [10], who were having clinical benefit increasing the oral wettability and hygiene.
Any artificial saliva has a local activity only and theoretically the favorable modification of OSA symptoms can be determined only by the moisturing effect in the mouth, which is maintained at least for few hours after the application. This local effect may consent an adequate elasticity of the pharinx, reducing the fluttering triggered by the rigidity of the soft tissues. A vicious cycle among the rigidity of the soft tissues and the pressure increase due to the air flow seems to be interrupted by AS, ending up with with snoring and (consequent) xerostomia reduction together with almost all the other OSA symptoms.
AS may have a role in all the picture because its rheological and biological properties (viscosity and film forming wettability) are very similar to the human saliva and can be maintained for many hours after the application [17].
Despite criticism about non prescription treatments of snoring or OSA [18], the present study shows that it is possible to detect some activity with a simple AS.
However, the findings that AS may improve OSA should be studied more deeply and further studies using polysomnography are needed to clarify the activity and mechanism of action of AS.
Conclusions
The use of MS+AS gel was found effective in the relief symptoms of OSA. Xerostomia, snoring, awakening with breath holding were shown to be the most sensible symptoms; gasping and choking, fatigue and sleeping during the day, were also significantly reduced.
These findings indicate that the maintainance of wettability in the oral soft tissues may improve the elasticity of the pharnix allowing a more relaxing and continuous sleeping that will have a favorable impact on OSA symptoms during the night and the day.
Aknowledgements
Funding
No funding was requested or given for this registry study. Certmedica International GmbH, Magnolienweg 17, 63741 Aschaffenburg, Germany was providing AS (aldiamed®mouth gel) free of charge, whereas the water gel was provided by the investigators. The patients were not paid for participating in the trial and received free treatments.
Ethical committee
Despite this registry study was not needing any official ethical approval, it was submitted to IAPSS (International Agency for Pharma-Standard Supplement- PE Italy) that gave its approval.
Authors contribution
UC, GB, were responsible for designing the research, CM, GB and FB were conducting the trial; UC and GB were responsible for trial data analysis; UC and GB wrote the paper.
Authors information: all the authors approved the text
Competing interest
None
References
- The international Classification of sleep disorders, revised (2001) Am Acad Sleep Med 17.
- Jordan AS, McSharry DG, Malhora A (2014) Adult obstructive sleep apnea. Lancet 383: 736-747.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S et al. (1993) The occurrence of sleep-disorders breating among middle-aged adults. NEJM 328: 1230-1235. [Crossref]
- Chi L, Comyn FL, Mitra N, Reilly MP, Wan F, et al. (2011) Identification of craniofacial risk factors for obstructive sleep apnoea using three dimensional MRI. Eur Resp J 38: 348-358. [Crossref]
- Lugaresi E, Cirignotta F, Montagna P (1989) Snoring: Pathogenic, clinical, and therapeutic aspects. In: Kryger MH, Roth T, Dement WC, eds. Principles and practice of sleep medicine. Philadelphia: WB Saunders 494–500.
- Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165: 1217-1239. [Crossref]
- Iftikar IH, Kilne CE, Youngstedt SD (2014) Effect of exercise training on sleep apnea: a meta-analysis. Lung 192: 175-184. [Crossref]
- Schecther A. Obstructive sleep apnea and energy balance regulation: a systematic review. Sleep Med Rev 2017; 34:59-69.
- Araghi MH, Chen YF, Jagielski A, Choudhury S, Banerjee D, et al. (2013) Effectiveness of lifestyle intervention on obstructive sleep apnea (OSA): systematic review and meta-analysis. Sleep 36: 1563-1562. [Crossref]
- Cornelli U, Belcaro G, Recchi M, D’Orazio N (2017) Long term treatment of overweight and obesity with polyglucosamine (PG L112): randomized study compared with placebo in subjects after caloric restriction. Curr Dev Nutr 1: e000919.
- Sato K, Shirakawa T, Niikuni N, Sakata H, Asanuma S (2010) Effects of oral care in Down syndrome children with obstructive sleep apnea. J Oral Sci 53: 145-147. [Crossref]
- Engelhart K, Popescu A, Bemhardt J (2016) Using mid infrared technology as new method for the determination of the dwell time of salivary substitutes on three dimensional gingiva models. BMC Ear, Nose, Throat Disorders 16: 6.
- Hahnel S1, Ettl T, Gosau M, Rosentritt M, Handel G, et al. (2010) Influence of saliva substitutes films on the initial adhesion of Candida albicans to dental substrata prior and after artificial ageing. Arch Oral Biol 55: 391-396. [Crossref]
- Belcaro G, Ippolito E, Dugall M, Hosoi M, Cornelli U, et al. (2015) Pycnogenol®and Centella asiatica in the mannagemet of asymptomatic atherosclerosis progression. Int Angiol 34: 150-157. [Crossref]
- The international Classification of sleep disorders, revised (2001) Am Acad Sleep Med pag 195-196.
- St-Onge MP, Shecther A (2014) Sleep disturbances, body weight fat distribution, food intake and/or energy expenditure: pathophysiological aspects. Horm Mol Biol Clin Invest 17 : 29-37.
- Giovani AM, Croci AT, Oliveira CR, Filippi RZ, Santos LA, et al. (2006) Comparative study of cryopreserved bone and tissue preserved in a 98 % glycerol solution. Clinics (Sao Paulo) 61: 565-570. [Crossref]
- Meoli AL, Rosen CL, Kristo D, Kohrman M, Gooneratne N, et al. (2003) Nonprescription treatments of snoring or obstructive sleep apnea: an evaluation of products with limited scientific evidence. Sleep 26: 619-624. [Crossref]
