Abstract
Intracranial hypotension (IH) has been recognized as one of the rare causes of chronic Subdural Hematoma (SDH), which is caused by post- procedural or trauma causing fistula or spontaneous intracranial hypotension (SIH). Due to its indolent course over time and variable in signs and symptoms, IH is often lower on a list of differential diagnoses during its initial presentation. We report case of SDH with SIH caused by Cerebral Spinal Fluid (CSF) leak from multiple spinal meningeal diverticula.
A 77-year-old female returned to the hospital for worsening clinical symptoms and worsening subdural hematoma, one week post-op from a right burr hole procedure for evacuation of a hematoma. Patient symptoms did not respond to standard surgical evacuation of subdural hematoma treatments. The patient postoperative imaging showed complete evacuation and effacement of basilar cisterns. Computerized tomography (CT) myelography showed multiple spinal meningeal diverticula. The patient underwent successful treatment with nontargeted epidural blood patch and bilateral middle meningeal artery MMA embolization after repeat bilateral craniotomies removal of SDH, leading to prompt improvement of neurological symptoms. Follow-up imaging showed resolution of subdural hematomas. Patient's new diagnosis of SLE can possibly have a pathogenetic relationship with multiple meningeal diverticula with subsequent spontaneous breakthrough of CSF leak.
Keywords
spontaneous intracranial hypotension, chronic subdural hematoma, cerebrospinal fluid, epidural blood patch, orthostatic headache
Introduction
Over the years, intracranial hypotension (IH) has been recognized as one of the rare causes of chronic subdural hematoma (SDH), which is caused by either post- procedural or trauma-causing fistula or spontaneous intracranial hypotension [1]. Both of these conditions present with low cerebrospinal fluid (CSF) pressure (<60 mm CSF), evidence of CSF leakage, brain sagging or pachymeningeal enhancement on imaging, with patients complaining of symptoms such as neck pain, tinnitus, changes in hearing, photophobia and/or nausea. These symptoms typically resolve after normalization of CSF pressure or successful sealing of the CSF leak [1]. According to The International Classification of Headache Disorders, 3rd edition (ICHD-3), there are three subtypes of headache attributed to low cerebrospinal fluid (CSF) pressure: post-dural puncture headache, Cerebrospinal fluid (CSF) fistula headache, or headache attributed to spontaneous intracranial hypotension.
For the purpose of this paper, only spontaneous intracranial hypotension (SIH) will be discussed. SIH was first recognized by a German neurologist, George Schaltenbrand [2]. According to ICDH-3, an orthostatic headache caused by SIH is characterized by low CSF pressure of spontaneous origin in the absence of a procedure or trauma known to be able to cause CSF leakage [1]. The CSF leakage can be found on spinal imaging which demonstrated ruptured or enlarged of pre-existing meningeal cysts.
The most common forms of meningeal cyst are perineural (Tarlov) cysts and meningeal diverticula. Tarlov cysts refer to the extradural portion of posterior spinal nerve roots in perineurial space between the endoneurial and the perineurial sheath. Classically, Tarlov cysts also contain nerve fibers within the cyst or in the lining of the cyst wall [3,4]. Meningeal diverticula are proximal to the dorsal nerve root ganglion and devoid of nerve fibers or nerve roots [4]. One of the usual symptoms of meningeal cyst leakage is postural headaches. However this symptom is not as prominent over time [1]. Other symptoms such as generalized weakness, nausea, vomiting, dizziness, cranial nerve deficits, and even seizure and altered mental status lead to SIH as the diagnosis of exclusion.
Case presentation
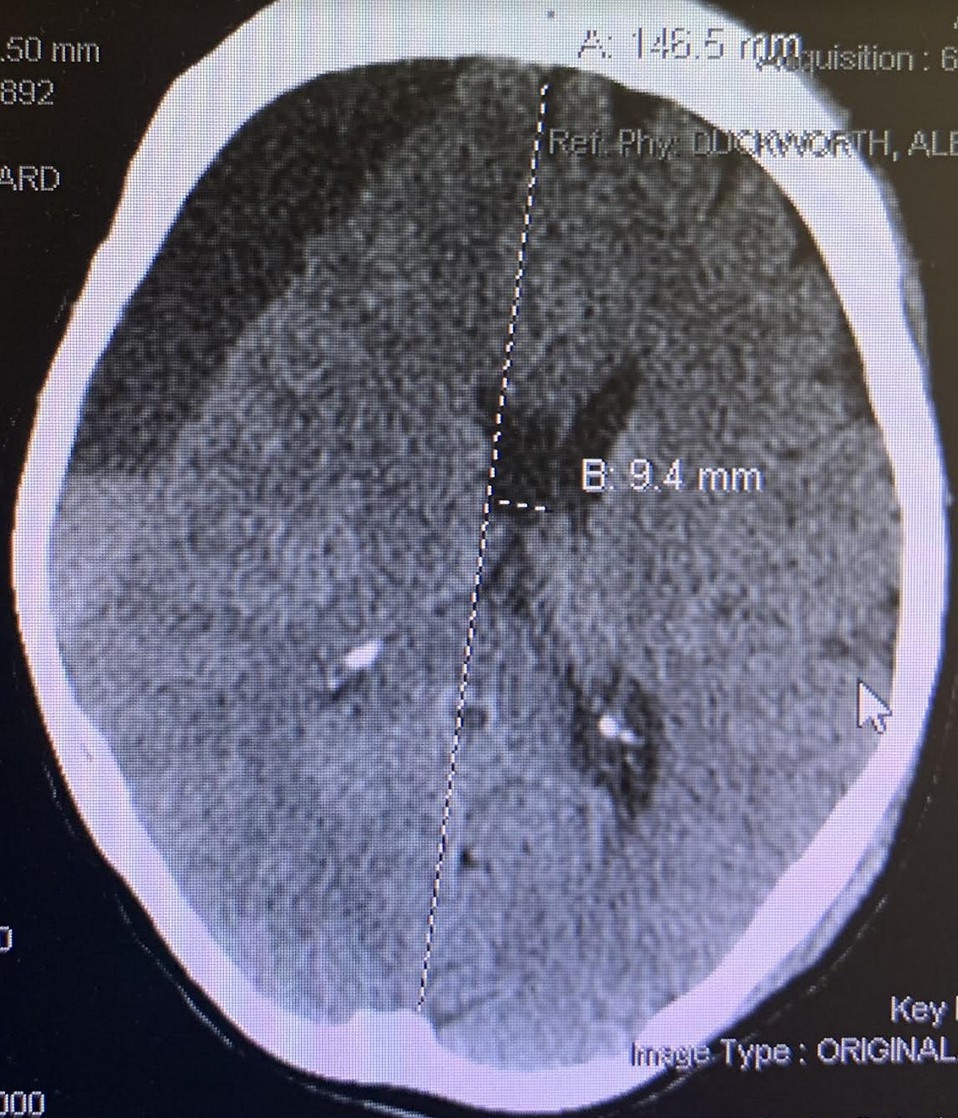
We reported a case of a 77-year-old right-handed female with a history of pre-diabetes, thyroid goiter, osteoporosis, hypertension, hyperlipidemia, transient ischemic attack/stroke on daily aspirin (ASA), presenting with one week of low-grade fever and generalized weakness. Patient had a fall in the bathroom and hit her head, prompting family members to bring the patient to the hospital. Computed tomography of the head (CTH) showed an old lacunar infarct in the right caudate nucleus, large acute on chronic subdural hematoma over the right frontoparietal region measuring up to 20 mm, and midline shift towards the left measuring 9.4 mm (Figure 1). On arrival, the patient was found to have significant sinus tachycardia, and the lab results were significant for urinary tract infection and chronic leukopenia. On exam, patient was awake, alert, oriented, with left facial droop, left drift, left sided weakness 4+/5.
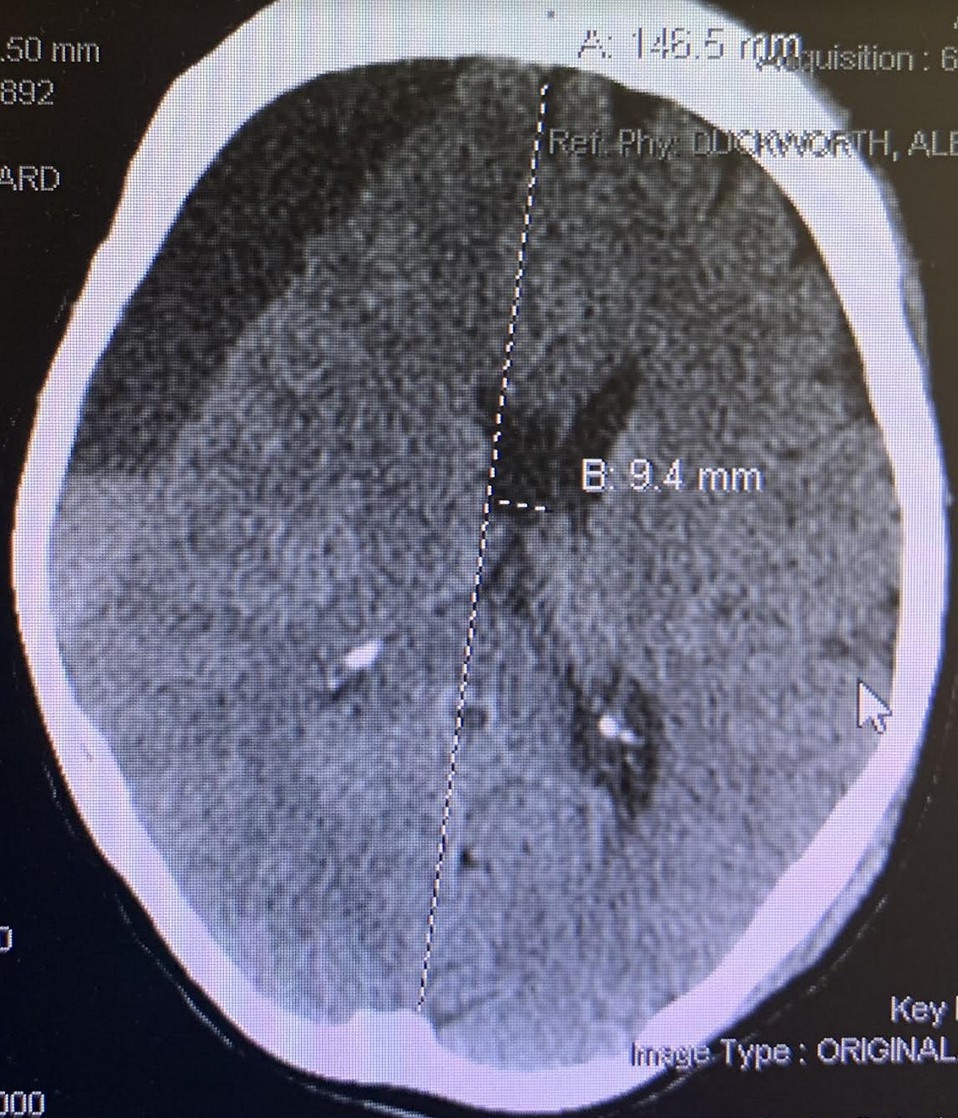
Figure 1. CTH large acute on chronic subdural hematoma over the right frontoparietal region measuring up to 20 mm. Midline shift towards the left measuring 9.4 mm
Patient was started on antibiotics and platelet transfusion, given the history of daily baby ASA used. Right Burr Hole craniotomy was done for evacuation of Subdural hemorrhage. After surgery, post op CTH demonstrated expected post op change with improved midline shift decreased to 4.2 mm. The patient was awake, alert and oriented after surgery, still had slight left facial droop, with improved left drift and left sided weakness (Figure 2).

Figure 2. CTH post op- expected pneumocephalus small SD fluid collection decreased midline shift to 4.2 mm
Of note, platelet count started trending down post operative. Patient was on Keppra for seizure prophylactic and due to concern for thrombocytopenia it was switched to Dilantin. On post op date four, patient had a transient episode of urinary incontinence and was aphasic, not answering questions, and staring. A code stroke was activated by nursing staff. STAT CTH showed residual fluid collection measuring 1.2 cm on the right and 0.7 cm on the left, no significant midline shift (Figure 3). The patient returned to baseline neurological status 50 minutes afterward, with no seizure detected on Electroencephalogram (EEG) and continued to improve throughout the remainder of the hospital stay. Discharged occurred on postoperative day 6 with recommendation for follow up with neurology for seizure management and hematology for ongoing evaluation of thrombocytopenia.
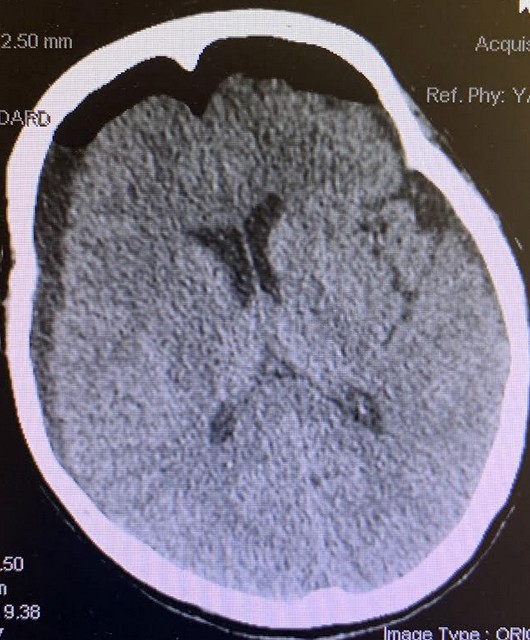
Figure 3. CTH axial showed residual fluid collection measuring 1.2 cm on the right and 0.7 cm on the left, no significant midline shift
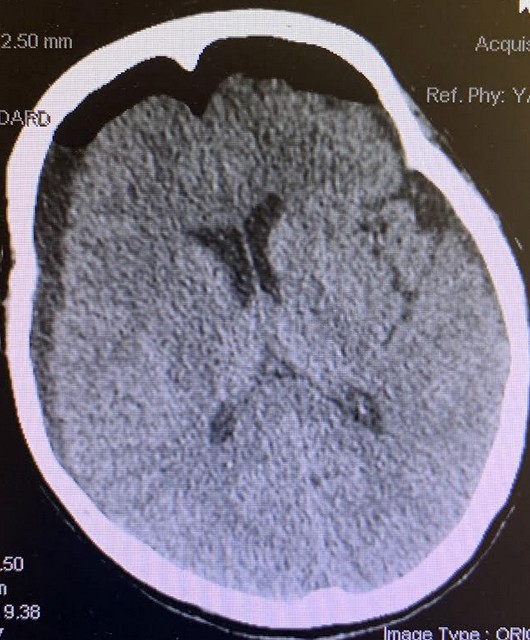
On Postop day 15, the patient was returned to the hospital for weakness and decreased appetite since discharge. On exam, patient was lethargic, followed commands intermittently, pupils equal round reactive to light (PERRL), left facial droop and left sided weakness 4/5. The patient was again found to have sinus tachycardia. The patient repeat CTH revealed resolution of the previously seen pneumocephalus, new interhemispheric SDH, previous bilateral subdural fluids collection increased right-sided subdural collection measures 16 mm in thickness compared to 11 mm previously and the left-sided subdural collection measures 11 mm compared to 5 to 6 mm previously, with increased midline shift to 6 mm (Figure 4).
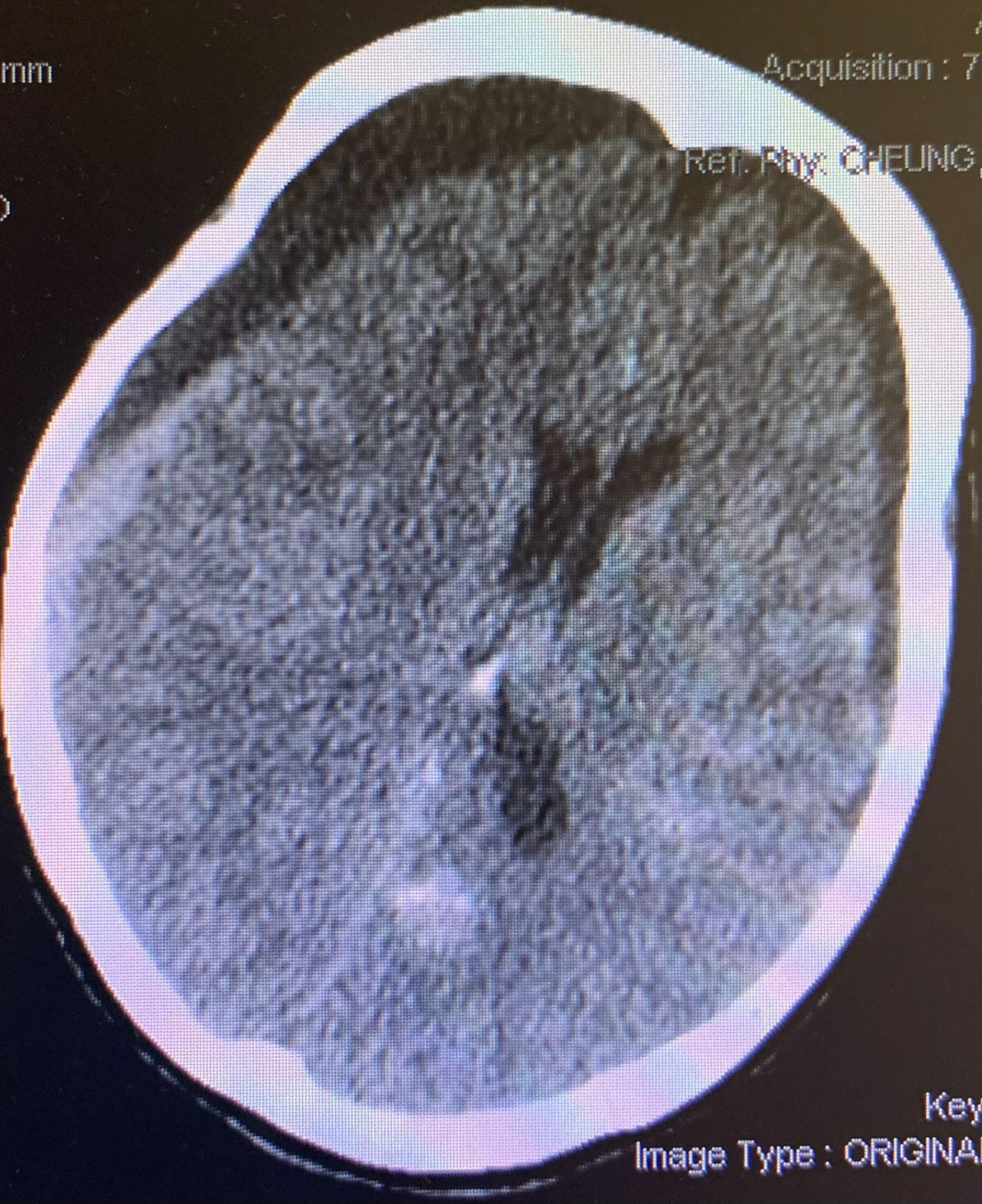
Figure 4. CTH - Resolution of the previously seen pneumocephalus, a large bilateral subdural hemorrhage more prominent on the right than the left
CT Myelogram showed multiple nerve root diverticula from cervical to lumbar with S1-S2 meningocele, no clear evidence of active CSF leak. However, there were multiple instances of contrast pooling around the thecal sac. MRI brain with and without contrast demonstrated meningeal enhancement. EEG was negative for seizure. On post admission day one patient clinically declined not to follow commands, for which patient was taken emergently to surgery for right craniotomy and left burr hole evacuation of subdural hematomas. After surgery, the patient was kept intubated.
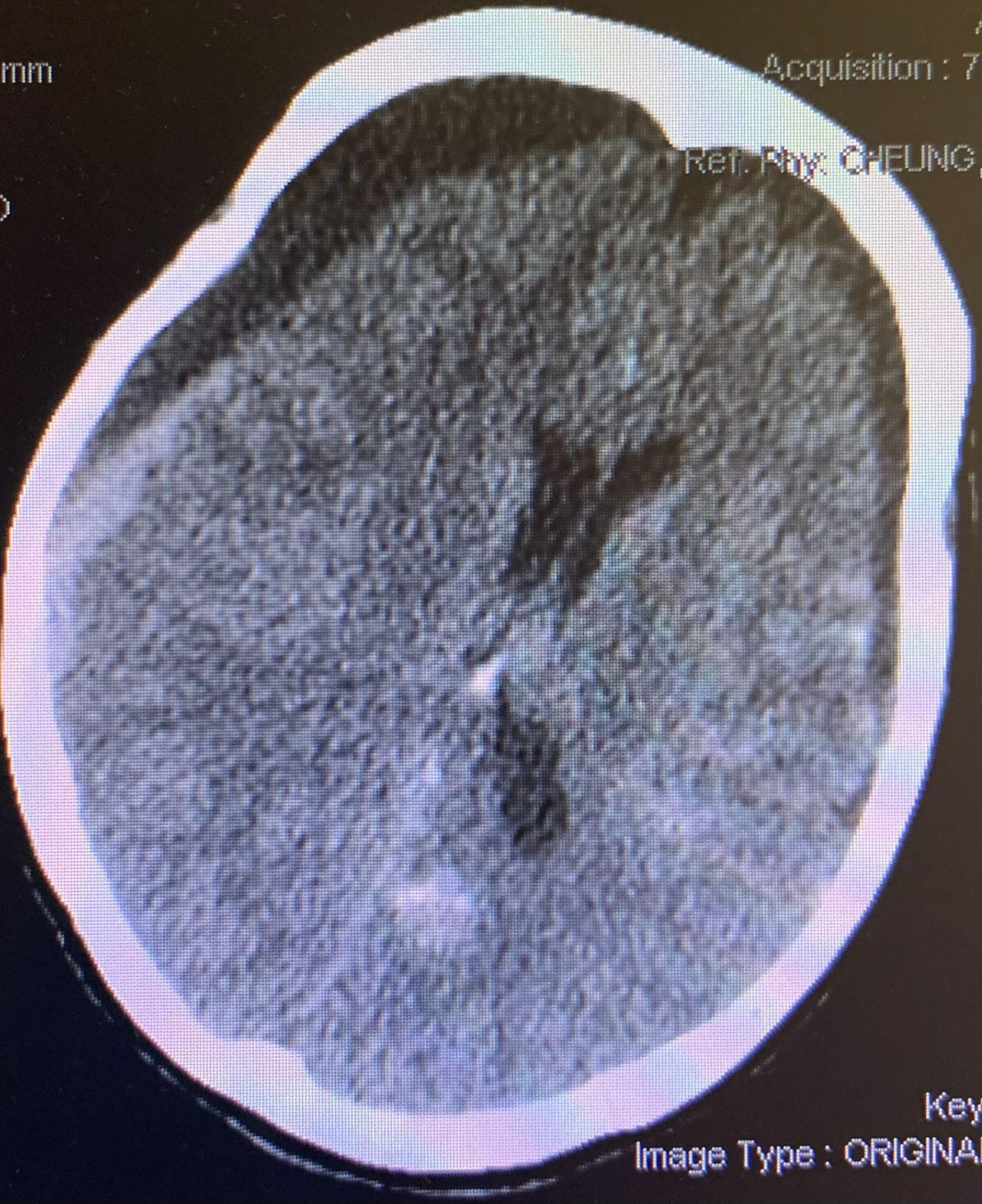
In the postanesthesia care unit (PACU), the patient was noted to have a seizure episode, with left upper extremity twitching which resolved with ativan administration. CTH showed subdural fluid evacuated with postoperative pneumocephalus and effacement of the basal cisterns which were concerned for downward herniation (Figure 5).

Figure 5. CTH post-operative with complete effacement of the basal cisterns
The patient was kept head of bed flat and the subdural drain was clamped. Sedation was changed to Versed. Patient then underwent epidural blood patch and bilateral MMA embolization and started to improve clinically and radiographically. On POD 7, the patient was awake and started to follow commands. Follow up CTH demonstrated decreased subdural fluid collection, basilar cisterns patent (Figure 6).

Figure 6. CTH status post bilateral meningeal artery embolization, resolution of subdural fluid collection with no midline shift, basilar cisterns patent
Patient’s hospital course was prolonged due to other medical issues. Patient had persistent pancytopenia during hospitalization with persistent chronic leukopenia, for which a formal bone marrow biopsy was performed, which revealed new Systemic Lupus Erythematosus diagnosis.
Patient subsequently discharged on post op day 48 to acute rehab with trach and peg. Three weeks afterward, the patient was discharged home with family care. At that time of discharge, the patient was tolerating a pureed diet with supplement tube feeds and was ambulating with a front wheel walker.
Results and discussion
Localizing the site of a CSF leak is difficult but crucial in SIH treatment. A delay in SIH diagnosing can lead to catastrophic rare complications such as worsening SDH, seizure, cerebral venous thrombosis [5]. According to Journal Headache Pain 2017 and Neurology 2020, there was a reported SIH incidence of 2-5/ 100,000 in the population, affecting females two to five times as often as males with a peak age incidence between 30-50 year old [2,6]. Positional or orthostatic headache is one of the early symptoms however, other time this symptom is much less obvious over time [1]. Only 50% of patients reported meningeal irritation symptoms, while other uncommon symptoms reported include: changes in hearing, difficulty balance, diplopia, blurring or visual field defects, cranial nerve paresis, numbness/weakness/spasm or pain, dysgeusia, galactorrhea, subtle cognitive deficits and coma due to diencephalic herniation [7,8].
Variable imaging modalities can be used to evaluate SIH. MRI with gadolinium contrast, CT, or digital subtraction myelography of the brain and spine can be used to provide radiographic SIH diagnosis and guide for treatment. Pachymeningeal enhancement, meningeal diverticula or extra-arachnoid fluid, subdural fluid collections, descent of cerebellar tonsils, obliteration of prepontine or perichiasmatic cisterns, and flattening of the optic chiasm, enlarged pituitary, and engorgement of cerebral venous sinuses are important features of SIH [1,7,9]. Other causes of meningeal enhancement must be ruled out such as meningitis or leptomeningeal metastases prior to concluding with a diagnosis of SIH as the cause of meningeal enhancement.
In addition, some studies report genetic connective tissue disorders predisposing patients to higher risk of developing CSF leak. However, the incident of CSF leak in patients with SLE was only through a small number of case reports. It was hypothesized that in SLE, inflammation could weakening and perforation of the dura [10].
Conclusion
Failure to recognize or delay in SIH diagnosis can cause further neurological deficits, coma or even death. Treatment for SIH is focused on restoring CSF volume/pressure and preventing further CSF leak. Previous reported conservative treatments such as bed rest, oral hydration, caffeine, steroids, theophylline and use of an abdominal binder were options. However, they lacked efficacy. In acute setting such as coma, intrathecal infusion of saline was reported to temporarily relieve symptoms. In the case of multiple meningeal diverticula and CSF leak that cannot be localized, nontargeted epidural blood patch can be used, and has a 70%-77% success rate in a first attempt and up to a 98% for second attempt [11-13]. Percutaneous placement of fibrin sealant, with a 30% success rate, can also be considered.13 However, if the site of the CSF leak is known, direct occlusion or surgical repair of the CSF leak are viable options [2,3,7,9].
Conflicts of interest
The authors declare no conflicts of interest.
References
- Headache classification committee of the international headache society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38: 1-211.
- Armstrong SA, Nguyen HT, Rebsamen SL, Iskandar B, Stadler III JA, et al. (2020) Epidural fibrin sealant injection for the management of cerebrospinal fluid leak following dural puncture in children. Cureus 12: e6940. [Crossref]
- Feigenbaum F, Henderson F (2006) Surgical management of meningeal cysts, including perineural (Tarlov) cysts and meningeal diverticula. Semin Spine Surg 18: 154-160.
- Häni L, Fung C, Jesse CM, Ulrich CT, Miesbach T, et al. (2020) Insights into the natural history of spontaneous intracranial hypotension from infusion testing. Neurology 95: e247-e255. [Crossref]
- Hillegass MG, Luebbert SF, McClenahan MF (2018) Percutaneous epidural hydrogel sealant for the treatment of spontaneous intracranial hypotension: A case report of chronic thoracic neuralgia and technical lessons learned. Case Rep Anesthesiol 2018: 4189518. [Crossref]
- Berroir S, Loisel B, Ducros A, Boukobza M, Tzourio C, et al. (2004) Early epidural blood patch in spontaneous intracranial hypotension. Neurology 63: 1950-1951. [Crossref]
- Cohen-Gadol AA, Mokri B, Piepgras DG, Meyer FB, Atkinson JL, et al. (2006) Surgical anatomy of dural defects in spontaneous spinal cerebrospinal fluid leaks. Neurosurgery 58: ONS-238-ONS-245. [Crossref]
- Lin JP, Zhang SD, He FF, Liu MJ, Ma XX, et al. (2017) The status of diagnosis and treatment to intracranial hypotension, including SIH. J Headache Pain 18: 1-8. [Crossref]
- Cohen-Addad DI, Efendizade A, Grigorian A, Hewitt K, Velayudhan V, et al. (2019) Spontaneous intracranial hypotension in a patient with systemic lupus erythematosus. Radiol Case Rep 14: 1188-1192. [Crossref]
- Yamamoto A, Hattammaru Y, Uezono S (2020) Spontaneous intracranial hypotension associated with cerebral venous thrombosis detected by a sudden seizure: A case report. JA Clin Rep 6: 59. [Crossref]
- Horikoshi T, Watanabe A, Uchida M, Kinouchi H (2010) Effectiveness of an epidural blood patch for patients with intracranial hypotension syndrome and persistent spinal epidural fluid collection after treatment. J Neurosurg 113: 940-946. [Crossref]
- Schievink WI (2006) Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA 295: 2286-2296. [Crossref]
- Tarlov IM (1938) Perineurial cysts of the spinal nerve roots. Arch Neur Psych 40: 1067-1074.