Abstract
FABTOTS, Fit Active Bodies babies and toddlers, was a community-based intervention programme targeting parents of children up to the age of three. It consisted of 2 hour weekly sessions over a six week period aimed at building parental confidence and fostering positive parenting through nutrition, physical activity and lifestyle choices. The programme was delivered by staff at the 18 Children Centres and one teenage pregnancy centre in Sandwell, one of most deprived and ethnically diverse towns in the UK. This paper outlines the development of FABTOTS and an evaluation of the short term impact of the pilot programme on the 173 parents who took part in the first year.
Mixed methods of data collection were used; group discussions with the participants took place at the end of each session and facilitators’ observations were noted for process evaluation. Participants completed a questionnaire about their experience of FABTOTS and behavioural changes. After six months, 25 participants took part in a follow up telephone interview to identify the sustainability of the reported behavioural changes.
Findings suggested that the programme was feasible and sustainable in the short term but highlighted a number of issues: recruitment, acceptability, retention, duration and content of the programme. Challenges in developing rigorous acceptable tools for data collection in an area with predominantly low literacy rates were noted. Evaluation of its long term sustainability is highly recommended.
key words
early years, positive parenting, food & nutrition programme, community- based intervention, community development
Introduction
Concerns about childhood obesity are mounting; recent global figures indicate an estimated 43 million obese children under the age of 5, with approximately 35 million living in developed countries [1]. The UK National Child Measurement Programme (NCMP) [2] data on childhood obesity showed that a quarter of reception children and over a third of year 6 were overweight and obese. The proportion of boys in the obese and overweight categories were higher than girls in both age groups. There was a strong relationship between deprivation and obesity, and obesity prevalence among children in both reception and year 6 that increased with socioeconomic deprivation [3]. The UK Government set a target to reverse the growing trend of obesity in children by 2020 [4] there is no indication of any intervention being successful in reversing this trend [5,6]. If current trends continue, it is predicted that the additional projected cost of obesity-related healthcare will be 5.3 billion £GB a year by 2025 and an overall projected cost for overweight and obesity to approach 49.9 billion by 2050 [7].
Childhood obesity is a risk factor for a number of chronic diseases in adult life including Type 2 diabetes, heart disease, some cancers and osteoarthritis [8]. Obesity is complex and is influenced by our behaviour, genetics, culture and environmental factors [5]. Understanding appetite control and its link to parental feeding practices has practical implications for parenting.
The increased obesity prevalence in children has highlighted the need to focus on contributory environmental factors which influence the diet and exercise routines of children, including parental diet and behaviour; socio-economic status; the power of marketing and perceived control over health behaviours [9-12]. Early years are important formative years for health and development of dietary preferences [10]. It is also the time when children are most dependant on their carers for food. For pre-school children the major determinants for food choices and physical activities is the home environment rather than peer group. Mothers have a major role in shaping family food in early years, particularly in low income families where scarce resources have to be managed effectively [9]. There is therefore a need to focus on a combination of early years of life and parental understanding for meaningful impact in combating the problem of obesogenic environments. Barriers to healthier eating in disadvantaged communities has illustrated that some people had good knowledge about what constitutes a healthy diet, but found difficulty in applying their knowledge with conflicting messages [13]. Pregnancy and having young children provides a good opportunity for parents, particularly mothers to improve their own diets as a result of providing healthy food to their children [9]. Targeting young families and parents of young children in deprived socioeconomic areas is therefore crucial in offering support to develop positive parenting, establishing healthy life style choices in early years and facilitating sustained change.
Sandwell has one of the highest rates of childhood obesity in the country: one quarter of children at reception (24.1%) and approximately half of year 6 children (43.7%) are classified as obese or overweight [2]. Sandwell also has high levels of multiple deprivation and is culturally and ethnically diverse. This poses a range of challenges in addressing the long term needs of the community through the introduction of interventions that are suitable, acceptable, effective and sustainable [3]. This pilot study aimed to evaluate the feasibility, suitability and acceptability of this low cost community-based intervention programme through examining the appropriateness of the training programme, issues regarding recruitment and retention, and positive behavioural change in parents.
Programme development and delivery
FABTOTS was a prevention programme for families with children up to the age of 3. The programme provided structured active-learning sessions focused on improving nutrition, physical activity, lifestyle choices and positive parenting. It included topics that relate to three stages of infant and child development: stage 0: antenatal phase (4 weeks), stage 1: 0–12 months (6 weeks), and stage 2: 12–36 months (6 weeks). The programme was developed in collaboration with local parents following a health promotion needs assessment exercise during which they indicated that they need more information on appropriate foods to feed their children and asked for support to help with their children’s physical development. To ensure capacity and sustainability of the programme, fifty seven staff from 19 out of 21 Children’s Centres were trained to deliver the programme (Figure 1). Children’s centres were provided with all the resources to deliver the programme including consent forms, monitoring and evaluation forms and branded hand-outs. A Healthy Lifestyle Adviser in each Centre acted as the main point of contact. The Adviser’s role was to support the programme facilitator, observe, advise accordingly and to monitor the sessions so as to ensure and maintain quality.
Figure 1. The programme design & implementation
Methods and materials
The objectives were to:
- Consult with parents about the content of the programme and whether the programme met their needs and how it could be improved;
- Identify any potential constraints in the implementation process;
- Establish the appropriateness and effectiveness of the handouts;
- Assess the appropriateness and the length of the programme;
- Assess what promotes and hinders attending all the sessions;
- Measure reported behaviour change as a result of the intervention.
As this was a service development, formal ethical approval was not required. However ethical principles; [14,15] were adhered during data collection, analysis and reporting. All participants were informed about the aim and objectives of the study and gave their consent before it began. Assurance was given about the confidentiality and anonymity of information provided, and that data would be used only to assess the suitability of the programme and its future improvement and adding to knowledge through sharing the anonymised information.
Data collection
The initial plan was to collect 24 hour food frequency and activity/play diaries on a selected day each week. However, within the first 2 weeks it became clear that most participants were not engaging with the task; the diaries were either not completed, or those who started completing the forms and diary forgot to bring them. Participants mentioned that they did not like filling in the forms/diary. In response to this, it was decided to have an informal discussion at the end of each session to reflect on the programme and to evaluate the process evaluation. An impact evaluation through a self-completed questionnaire was carried out at the end of each programme. The self -reported questionnaire was developed by the evaluation team for this programme. It had structured and some open ended questions to provide an opportunity for participants to feedback on their experience of taking part in the programme and also to record any potential behaviour changes. Questions included any changes made in relation to food choices: shopping, cooking, consumption of fruit and vegetables, high salt and fat food, feeling confident in cooking, dealing with fussy eating children, reading food labels as well as any changes in their children’s routine in terms of TV viewing and play. Information was also collected about what participants valued best about the programme, what did they liked or disliked and how the programme could be improved. Finally, the experience of delivering the programme was also collected from staff through informal discussion.
Data analysis
Quantitative data from questionnaires were checked, coded and analysed using IBM SPSS Statistics software version 24. Descriptive and inferential analyses were carried out by age group, ethnic background and the stage of programme attended. Chi-square and Fisher Exact were used where appropriate, the level of significance for all tests was set at p = .05. Confidence interval of a proportion or count was calculated using the Poisson distribution [16].
Qualitative data from the open ended questions and notes from discussion group and facilitators’ observation were typed, and analysed using Ritchie & Spencer’s [17] thematic approach and Rabiee’s guidelines [18] to identify themes and sub-themes. Data were interpreted taking into account the context within which topics were mentioned, the frequency and extensiveness of comments made, the intensity of comments, internal consistency, specificity of responses and the emergent picture. To ensure anonymity, each participant was coded by the first initial of the Centre followed by a number to show the intervention phase (0, 1 or 2), a number to identify the participant and the first letter of their ethnicity. For ethnicity the first initial letter was given (W for white, P for Pakistan, I for Indian, A for African, AC African Caribbean & M for mixed background). So, B03A meant an African participant number 3 from phase 0 at Bearwood, R14P means a Pakistani participant number 4 from family phase 1 at Rawley.
Results
When appropriate the results of quantitative and qualitative data are combined. Two hundred and twenty seven people aged between 15 – 41 years (M=31.8 years and (SD= ±2.8) participated in 32 programmes over a 12 month period, of those 173 (76%) completed the programme, attending a minimum of 4 out of 6 sessions. Participants were parents, grandparents or guardians and were either self-referrals or referred by Social Services or their GP as part of a care plan. Findings from those participants who completed the programme are presented in this paper.
Of the 32 programmes delivered, 6 were phase 0, 7 phase1 and 19 phase 2. The number of participants who attended and completed each programme ranged from 5-19. Phase 2 was the most popular with a retention rate of 90%, followed by phase1 with a retention of 76% (Table 1). The majority of participants were white (40%) followed by South Asians (31.5%) and black African or African Caribbean (26%), table 2 shows further details.
Table 1. Proportion of participants who have attended & completed different stages of the programmes
Intervention Programme in each phase |
Attended |
Completed * |
Confidence Interval** |
|
N |
N % |
(95% CI) |
Stage 0: Antenatal phase (n=6) |
38 |
13 34 |
0.24-0.55 |
Stage 1 (n=7) |
76 |
58 76 |
0.66-0.85 |
Stage 2 (n=19) |
113 |
102 90 |
0.83-.95 |
Total |
227 |
173 76% |
- |
*= Number of participants who completed a minimum 4 out of 6 sessions
**Test of Proportionate
Table 2. Participants’ Ethnic Backgrounds
|
Participants
|
N
|
%
|
|
White
|
70
|
40
|
|
South Asian:
|
-
|
-
|
|
Pakistani
Indian
Bangladeshi
|
27
23
4
|
16
13
2.5
|
|
African & African Caribbean:
African Caribbean
African
|
-
26
19
|
-
15
11
|
|
Mixed Background
|
4
|
2.5
|
|
Total
|
173
|
100
|
The majority of participants (93%) stated that they enjoyed the programme; 85% said it was well organised and 89% stated that they would recommend it to others. In relation to the organisation of the programme a number of participants mentioned:
“well organised, information was in order and the basics of child development was invaluable.”B03A
“Yes, every session was organised really well. Had a good variety of input i.e. instructor led, group discussion, group work.” O23I
The variety of inputs and in particular group work and discussion were valued, as they provided an opportunity for participants to air a number of concerns in relation to parenting skills and dealing with fussy eaters;
“The advice offered for weaning, routine, sleep. Experienced advice from people who have children.”R14P
The social aspect of the learning including peer group learning, provision of learning materials and crèche facility were frequently praised;
“Everyone was friendly, the fact that you can put them (Child) in the crèche and only be next door. The fact that they provide everything – ingredients, toys, etc. Crèche free I think that’s brill.” F27W
“Yes staff were good and the crèche in the room was lovely. It put my mind at ease not being far from my baby.” F14M
“Social aspects, cooking, chatting to other mums and course leaders about eating habits, problems etc. and resolving problems getting help and advice and good ideas and tips.”G21P
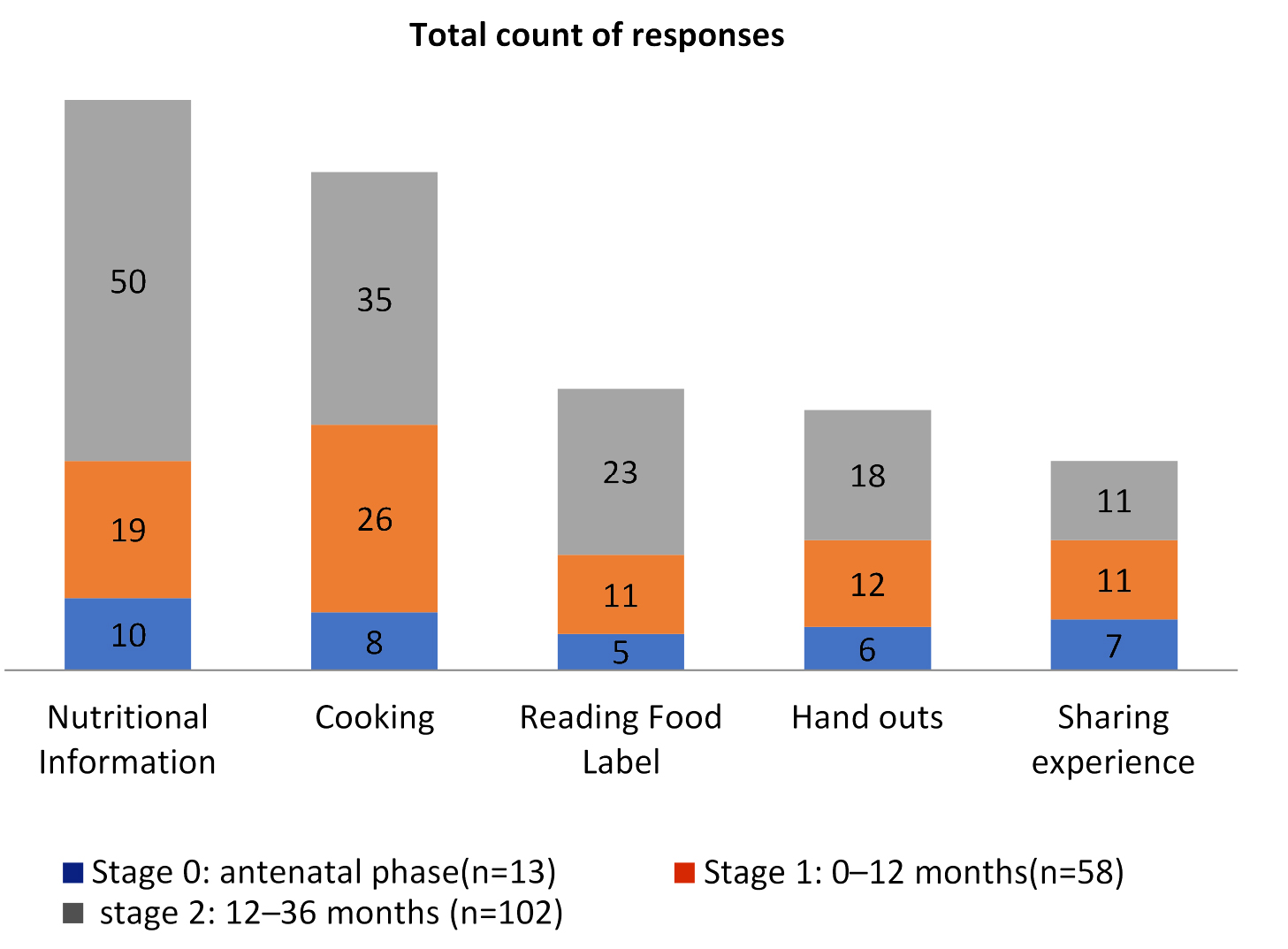
In response to what they liked best about the programme, participants from different intervention phases(0,1 and 2 ) identified a range of topics (Figure 2); but nutritional information and cooking sessions were the top two areas highlighted, followed by reading food lable, hand outs and sharing experience. Participants clearly valued the multi-dimensional aspects of the programme. In relation to food and nutrition the followings are the most frequent comments made:
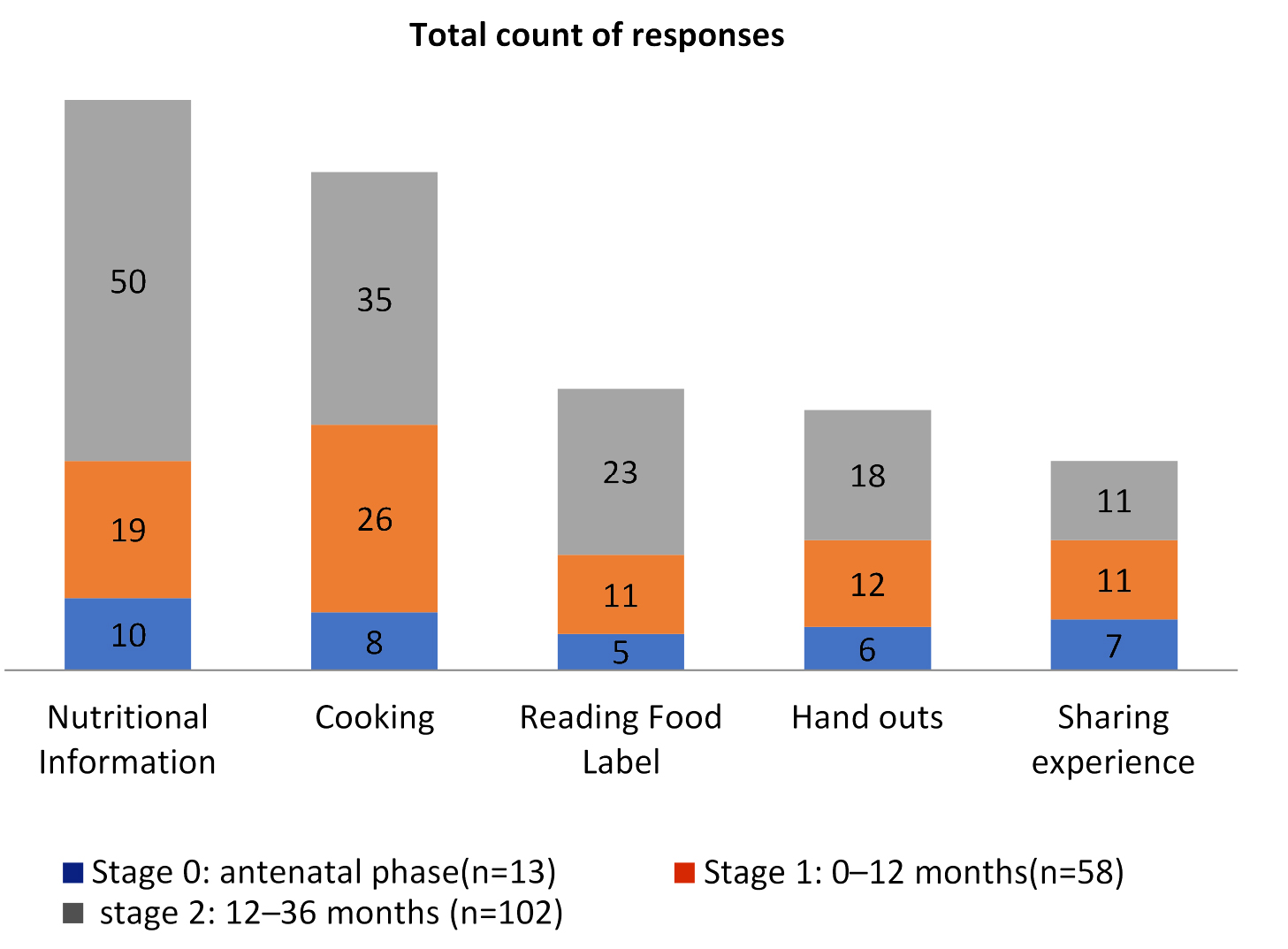
Figure 2. What participants Valued Most From Each Stage
“Learning about healthy eating, cooking, meeting new mums.”H02AC
“The whole course has been great and an eye opener. The session on salt and sugar has made a big difference in my diet.” O23I
“Learning different recipes for when I start weaning my baby. Learning how to read food labels. Knowing calorie intake and what portion amounts are recommended for each food group for both myself and my children.” C16A
Participants were pleased that the facilitators recognised that some of them were at different stages and needed more help. They also felt that the programme was really helpful in facilitating discussion on wide range of issues such as getting parents and children eating more fruit and vegetables:
“It was delivered professionally and at a great pace. The handouts were also very useful, especially the cards containing different sugars and fats.”C08P
There was however occasional criticism that the programme didn’t fully cater for the multi-ethnic communities, especially in relation to recipe and cooking programme:
“I’m still struggling with the fact that we cooked sausage rolls which have no nutrient goodness in them. Yet we couldn’t cook sweet and sour chicken jambalaya etc. It needs to be more creative and cook for other ethnicities. My son is mixed race and loves Jamaican food.” T22W
Participants mentioned finding out about how much fat, sugar and salt is hidden in foods as really helpful. They all liked the cooking sessions adding that the recipes were healthy and easy to follow and did not take a lot of preparation was a great bonus:
“Information about the fats, salts and sugars in food and jars compared with home cooking. Enjoyed the practical sessions cooking meals, this was really enjoyable.” R13W
Participants valued the practical aspects of the course and enjoyed all nutrition information sessions, but found the cooking, food labelling, information about hidden fats, sugars and salts in food particularly useful:
“Learning to read food labels for the content of ingredients such as salt and sugar enabling me to make better food choices.” F04W
“The handouts and the chart showing you how to work out how much sugar and salt in your food and the recipe book.”O12P
Being able to talk and discuss as a group and sharing information was extremely helpful and empowering:
“Knowing that what I’m doing isn’t too bad and that I now have more ideas for cooking and what to look for when shopping.” C25P
“Finding out what other parent think and behave with their kids.” G24M
Participants were asked if there was anything they didn’t like about the programme. Overall participants were satisfied with it, although a quarter (n=44) mentioned they didn’t like filling the forms and keeping the diary as it was time consuming. 8 people felt that the programme was overloaded with information at the beginning and again this resulted in the programme being adapted to address this issue. The flexibility of the facilitators by adapting the programme to meet the learning needs of the participants were key to overall satisfaction and retention rate. The informal discussion at the end of each session for process evaluation therefore appeared a useful excercise. Almost half of the participants felt that increasing number of people attending would have improved the experience for them. They were also not pleased with other participants “coming in late” or “not turning up”.
In response to what could make the programme better, the main suggestions for improvements was for more activities and games, and more cooking sessions, which supports the importance of practical aspects of the course and its usefulness for adult learners.
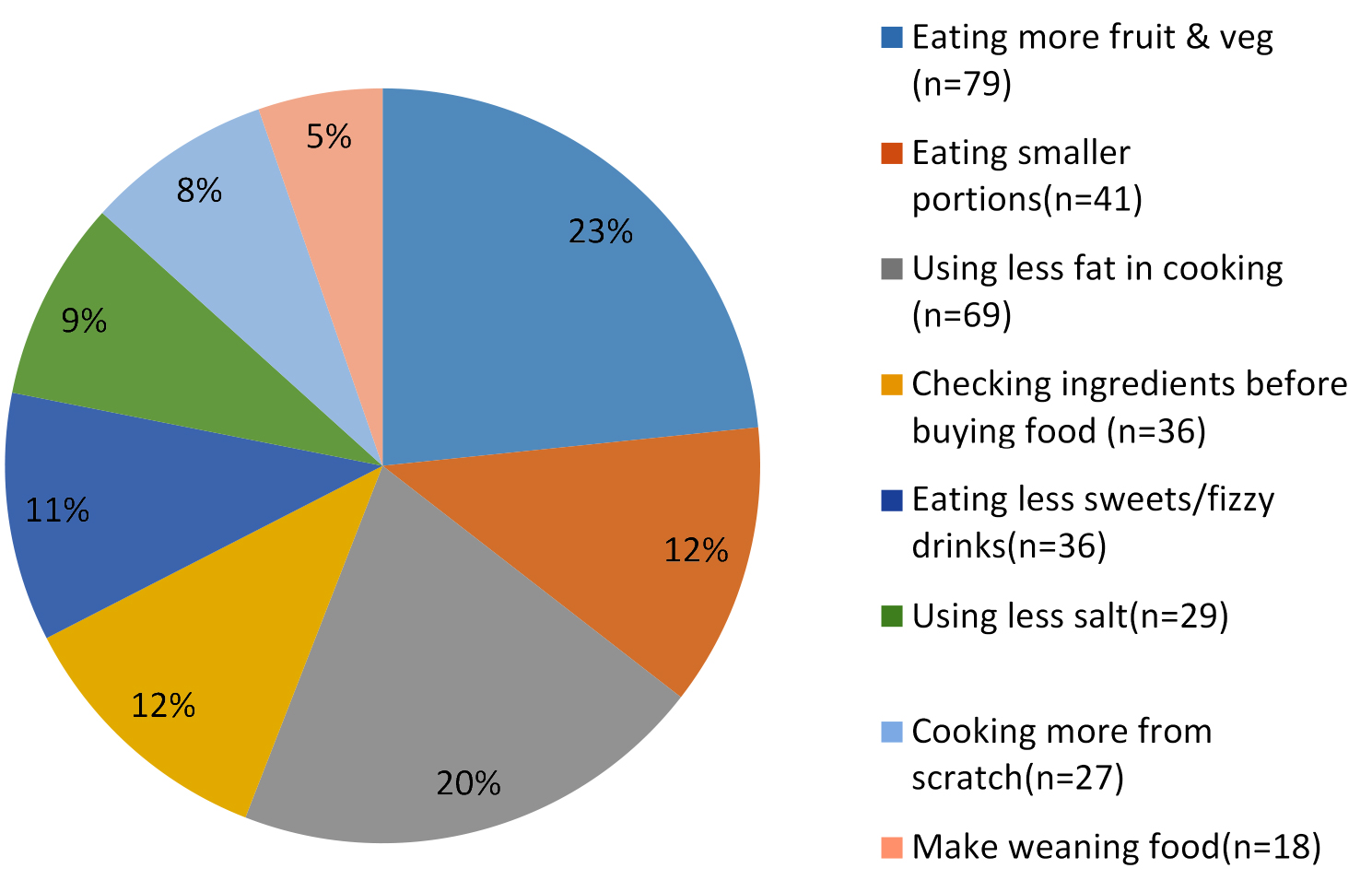
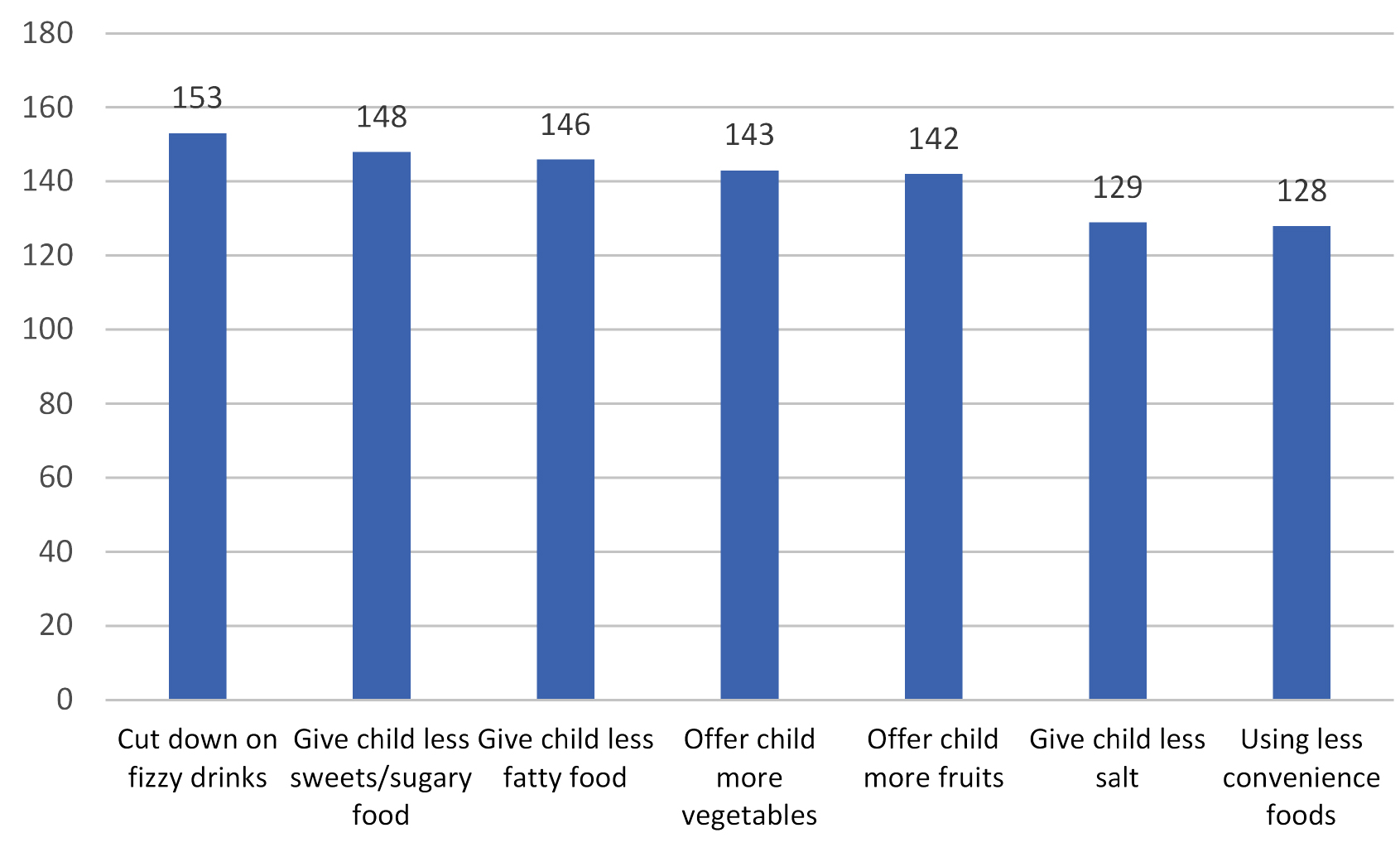
Paticipants were asked if the programme made them think differently about food, physical activity, TV screening and routines for kids. With the exception of 2, everyone answered positivity to this question; 94% (n=163) of them reported at least one positive behaviour change in relation to food, physical activity and/or positive parenting. As mentioned earlier date was collected via a self-reported questionnaire developed by the evaluation team for this programme. When analysed for outcome, there was no significant effect of ethnicity or age (judged by Fischer's exact test) on the likelihood of a food change or change in physical activity at the 0.05 level, figure 3 highlights reported changes made by parents for the family and figure 4 gives the top 6 food and nutritional changes made for their children. In addition participants reported that they tended to read food labels more, changed cooking methods including using less fat, making food without ghee, reducing fat, sugar and salt, cooking more meals and baby foods from scratch, using less commercial baby food, reducing portion sizes, and eating less processed foods:
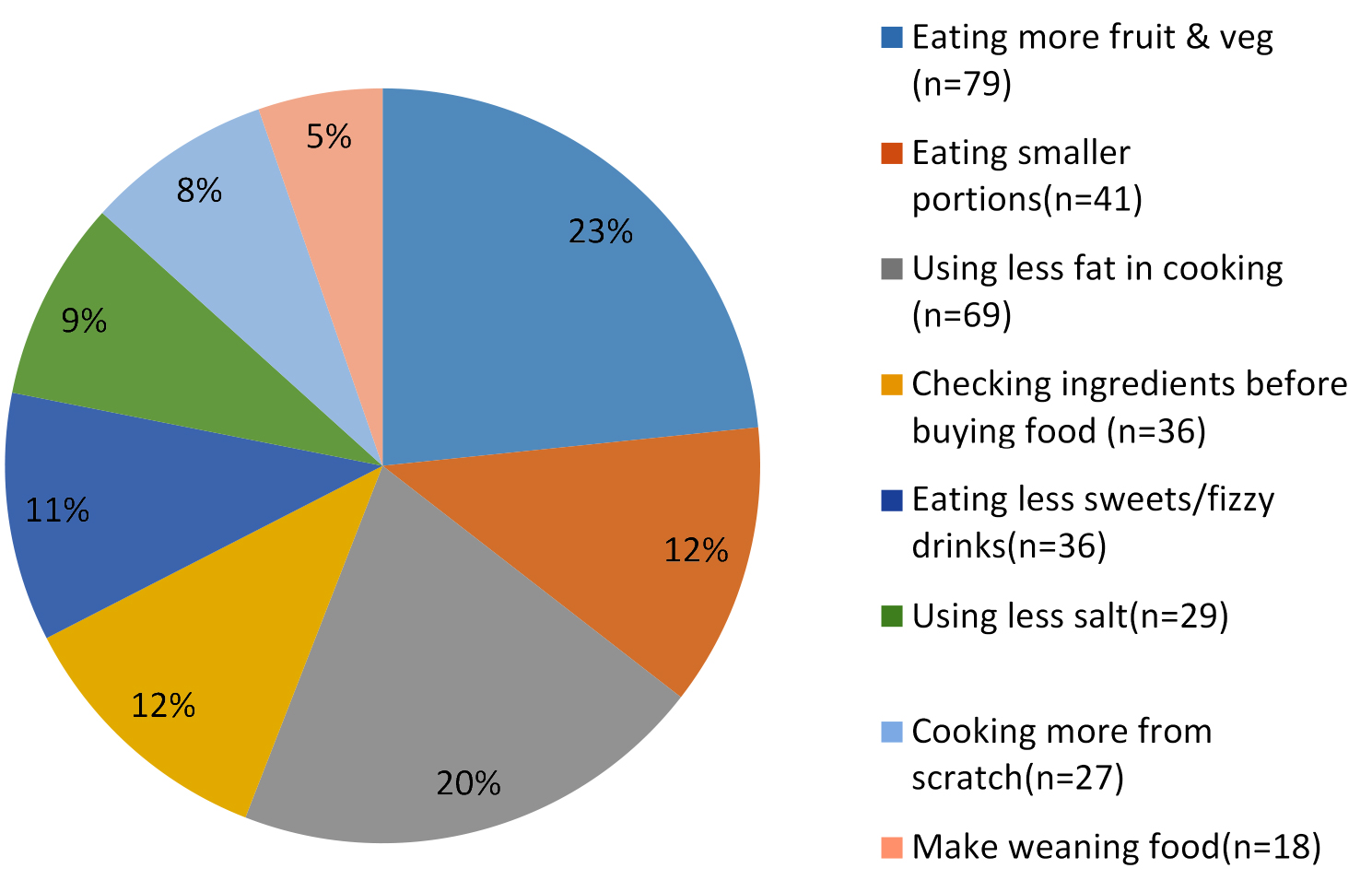
Figure 3. Reported Food & Nutritional Behaviour Changes (n=173)
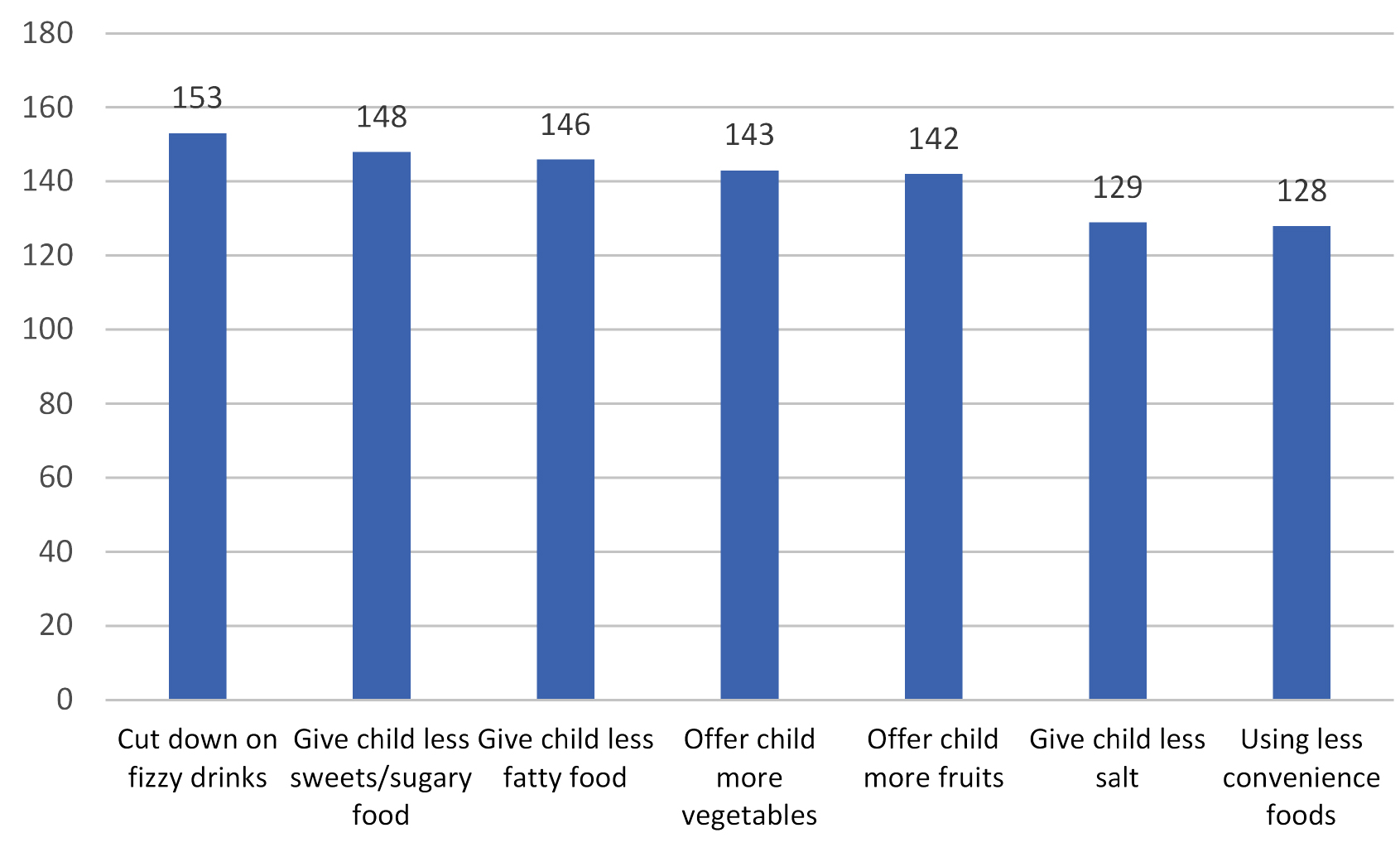
Figure 4. Top 6 Reported Food & Nutrition Changes for Their Children(n=173)
“Ensuring my baby gets a variety of foods. I’ve bought a steamer and slow cooker as a result of FABTOTS.” U23W
“I have stopped using jarred food and started making more homemade food and have noticed he is sleeping better since stopping jars.”C17I
“I do more cooking activities with my son to make much more exciting and he now explores more different healthier foods.” R26W
In response to reported physical activity behaviour: 77% said walking more, 73% mentioned doing more activities together as a family, 63% stated taking their child to the park more often and 25% said tring to use the car less for short journeys.
“Letting him walk more instead of putting him in the buggy.” F21AC
“I took [name of the baby] to the park for the first time this weekend and I’ll be taking him to play more often.”C12P
“Playing bean bag games and ball with kids. The practice is good exercise for the hand.”T23I
Parents reported changing their children’s bedtime routines (39%), ensuring that their child sat at the table to eat (67%) cutting down their children’s TV time (74%) and turning the screen off during meals (63%). A number of participants mentioned they were now “Talking to the children more, and reading to them.”
“Maybe watch TV for half an hour in the evening, then we are doing things as a family.”G21M
“We don’t have the TV on at playtimes and mealtimes.”R24AC
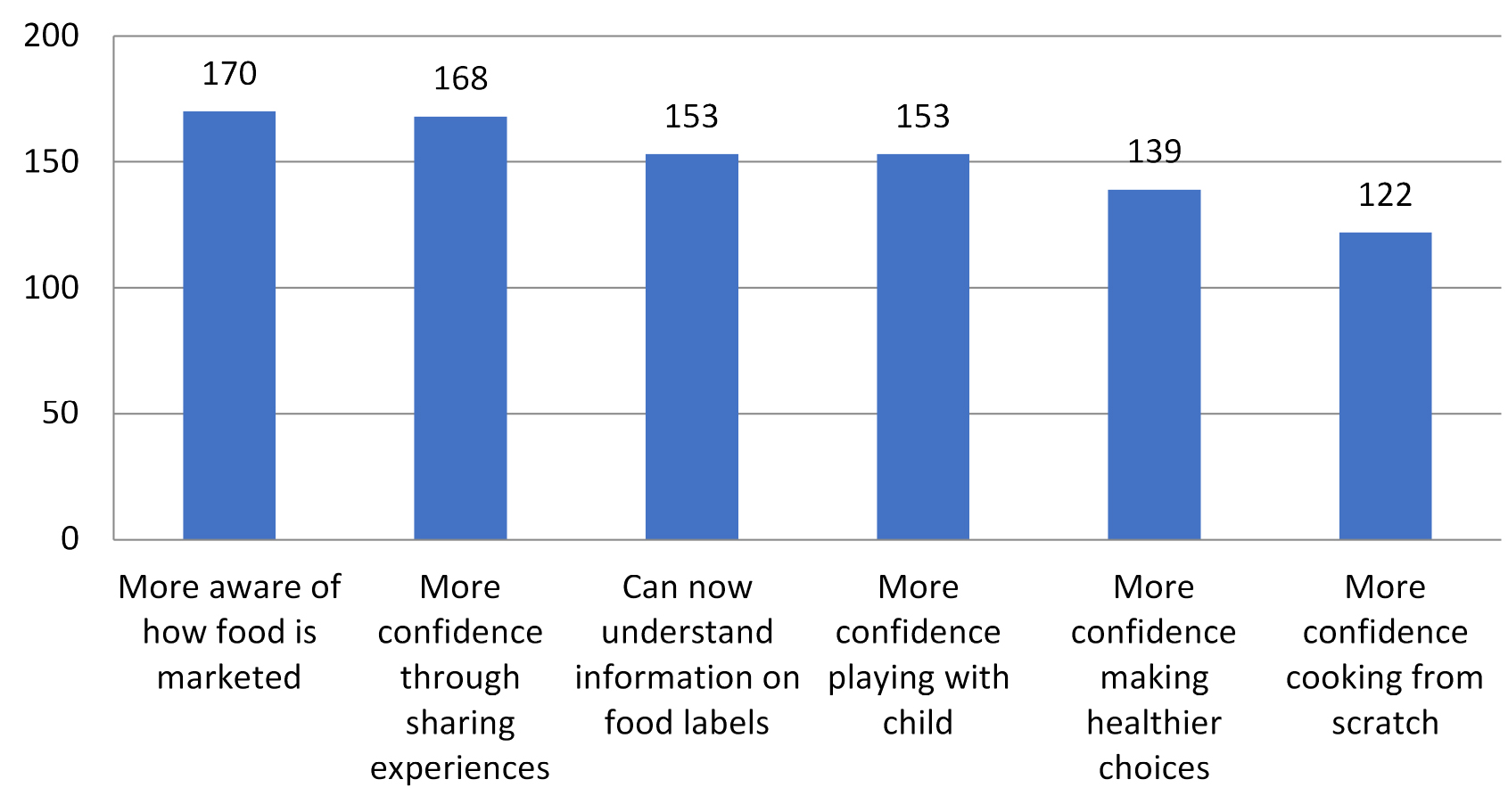
One of most pleasing changes reported by a high proportion of participants was how they built confidence and developed skills. Figure 5 shows the top 6 areas highlighted; almost everyone (98%) said they are more aware of how food is marketed to parents and children. Almost an equal proportion (97%) said they had more confident since meeting other parents and discussing ideas and tips. They now understood the information on food labels (88%), were more confident about making healthier choices (80%) and cooking from scratch (70%). They were more confident in playing with their children and understood its importance in child development and bonding (88%).
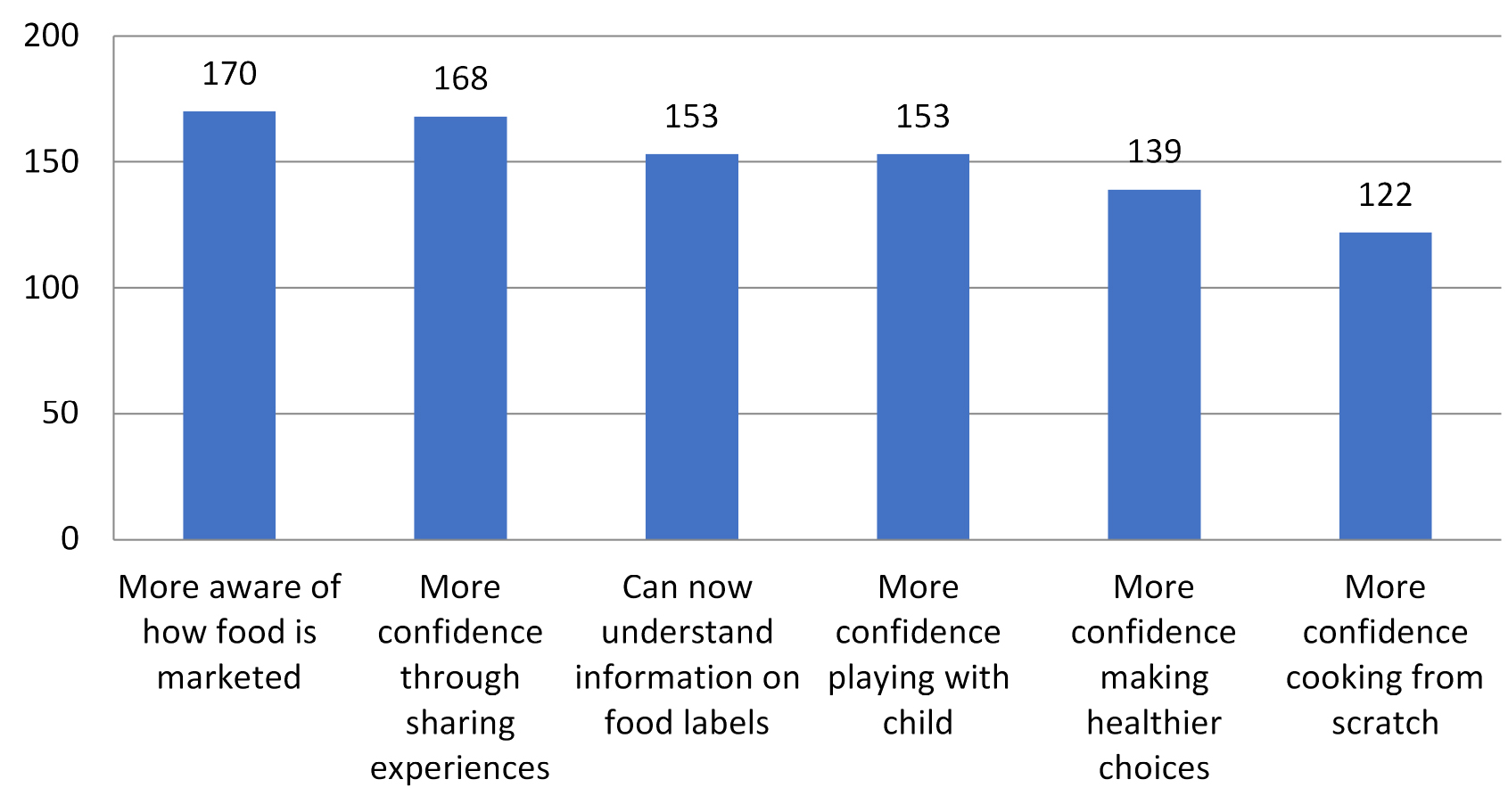
Figure 5. Top 6 skills developed reported from total number of 173
Post intervention telephone interview
Six months after completing the programme 25 randomly chosen participants (15%) followed up with a telephone interview to assess the sustainability of the reported behaviour changes. Questions included what they liked best about the programme and if it continued to influence their thinking about food and physical activity. Responses indicated that all 25 participants maintained changes that they had made in their pattern of food or physical activity, some mentioned additional changes in relation to food:
“have cut down on portion sizes”, “Changed the oil I use for cooking; no more ghee”; Stopped giving my children Lunchables as I learnt that one used in training hadn’t changed in appearance after two years.”; “More aware of what I’m eating.”; “Felt I fed the children healthy already, but now think more about” , “For my little one, she is a fussy eater and I read the label to see what is good for her. I give her things that are healthy she has five a day now” and “I cook with my children more now, which I think they really enjoy”
More changes were mentioned in relation to drinks: “I make sure juice is well diluted and give more water”; “I try to give water instead of pop now”; and “have become more conscious of giving healthy snacks, cutting down on fizzy drinks”.
Other changes also reported:
“We tend to be out and she has more things (toys) in the garden now. I bought a slow cooker, use that a lot. I only buy ready meals once in a blue moon, but never really bought them anyway”.
In relation to physical activity, respondents mentioned the following: Walking more now, use the car less.”; “Try to be more active with the kids”.
Other changes i.e. positive parenting, a number of respondents mentioned that they “Have cut TV time down for children”; “I have used baby-led weaning since doing the course and my baby has really come on loads. He eats great now”; I have tried to include more healthy snacks and like to go outside and play more with my children”.
Reported changes in the diatary pattern, physical activity, and pareting skills and confidence six months post intervention programme clearly indicated lasting impact of the programme on healthy lifestyle choices and fostering positive parenting.
Discussion
Monitoring behaviour change without any base line data can be very difficult as the validity and reliability of self-reported behaviour tools are questionable [19]. Twenty four hour food recall and physical activity diaries were included originally as part of the evaluation process but were not completed consistently enough to be included in the final evaluation. Approximately a quarter of the participants, irrespective of age and ethnicity, said they did not like filling forms or diary; “it was time consuming”. This may have been due low literacy levels [20], or a lack of confidence in sharing the information. The community- centred approach [21] of the programme required negotiation and flexibility. Opting for group discussion at the end of each session and reported behavioural change at the end of each programme were therefore a good compromise to make participants feel comfortable and encourage them to continue with the programme.
More than two third of the participants (76%) completed the programme (Table 3), which clearly indicated that participants valued the programme, found it interesting and useful. There was a significant effect of the stage of the programme and the regularity of contact on the likelihood of families completing it, especially stages 1 and 2 (as judged by Fischer's exact test, p < 0.004). The popularity of these two phases may reflect relevance to parental circumstances after having children and the practicalities of caring for them. This was particularly evident in weaning; most parents waited until their baby was six months before weaning [22]
The antenatal phase had the lowest retention rate (34%), and was also challenging to establish with the exception of one programme run especially for teenage mothers. This was partly to do with the lack of referrals from and communication with midwives Pregnancy is a challenging time for women; being able to take time off work, attend ante natal classes and FABTOTS may have been too much for some.
Participants talked frequently about impact of the programme, in terms of information, resources and learning new skills. They highlighted the value of information received about food, weaning, healthy eating, nutrition and food labelling, the amount of exercise required, TV screening and play “The day they showed us how much fat we eat it was shocking but true and now I think twice before I eat. The advice of how I can help my baby to sleep by massaging her, which worked perfectly and also how I can help my baby to eat by switching off the TV also worked as well perfectly.”F27A. Resources such as handouts and food label cards were highly valued as were the cooking skills and the opportunities to talk to other parents. The informality encouraged information sharing, social support from peers and confidence building which is consistent with previous research [23,24].
As part of the programme, participants are offered an opportunity to visit a local market garden. This was part of a stand-alone service delivered in partnership with a local agency. They operated a vegetable bag scheme to encourage local communities to buy local fresh produce. The market garden reported to facilitators that the number of bags they sold had increased and this was partly due to the demand by parents visiting from the Children’s Centres. This supported the reported behaviour changes that indicated participants were using more fresh ingredients. Whether increased knowledge and confidence in cooking or relative low cost and access to fresh ingredients was a contributory factor requires further investigation.
Obesity is complex and requires a multifaceted approach that addresses the problem on many levels. People need to be motivated to make positive behaviour changes [25]; they also need to gain the confidence and belief in themselves [26] to make the changes sustainable. More importantly helping people to gain the skills that will enable them to make informed decisions is most effective and empowering. Data generated from discussion with parents in this pilot study and during the 6 months follow up, confirmed the community-centered approach [21] taken for this programme was valued by participants as well as effective in building parental confidence and fostering positive parenting through increasing their knowledge, confidence and skills in making healthy lifestyle choices. The link between poor diet, health and poverty among lower socio economic groups are well established independent of obesity [27,28]. The important role of parents in establishing healthy lifestyle in early years is well documented [29]. The programme was based on positive parenting [30] and had a life course approach to healthy lifestyle [31]. Focusing on early years and supporting parents of young children increased participants’ knowledge, skills and ability to implement healthy lifestyle in their household, develop positive parenting and sustain it for at least 6 months post intervention programme.
Conclusion
Findings suggest that the implementation of this low cost intervention programme is feasible in deprived areas and the changes made also appear to be sustainable in the short term. Evaluation of the long term sustainability is highly recommended. For future programmes it is recommended to:
- Make cooking sessions relevant to multi ethnic population
- to validate the questionnaire developed for this programme
- Build in evaluation of other services such as shop tours and grow well as these add value to the programme.
- Build in confidence measures to the evaluation establishing how far participants have come through the process.
Acknowledgements
Our gratitude to all participants who took part in the programme for giving us their time, thoughts and experiences of attending the programme. We are also grateful to staff and facilitators at Children’s Centres in Sandwell for their commitment, enthusiasm and invaluable advice, support and facilitation. Special thanks to Robert Cook & Stavroula Bibila for their technical support regarding quantitative analysis. Last but not least thanks to Silvia Gullino for her constructive feedback, Paula McGee for her valuable comments and expert editing & Amy Foster for proof reading.
Conflict of interest
No conflict of interest. The programme was funded by the Sandwell Public Health Dept as part of the Childhood Obesity Prevention Programme.
References
- World Health Organisation. (2012) Childhood overweight and Obesity. [Available:
http://www.who.int/dietphysicalactivity/childhood/en /]
- NCMP (2016/17) National Child Measurement Programme - England, Official statistics, National statistics. [Available:
https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement-programme/2016-17-school-year]
- Public Health England (2017) Health Inequalities. [Available at
http://webarchive.nationalarchives.gov.uk/20170110170055/https://www.noo.org.uk/NOO_about_obesity/inequalities NCMP and Child Obesity Profile ]
- Foresight report (2007) Tackling Obesities: Future Choices. [Available:
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07-1184x-tackling-obesities-future-choices-report.pdf]
- Foresight (2017) Dusting off Foresight’s obesity report. [Available:
https://foresightprojects.blog.gov.uk/2017/10/04/dusting-off-foresights-obesity-report/]
- Department of Health and Social Care (2017) Childhood obesity: a plan for action. [
https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action/childhood-obesity-a-plan-for-action]
- PHE (2017) Health matters: obesity and the food environment. Public Health England. [Available:
https://www.gov.uk/government/publications/health-matters-obesity-and-the-food-environment/health-matters-obesity-and-the-food-environment]
- World Health Organisation. (2012) Global Strategy on Diet, Physical Activity and Health. [Available: http://www.who.int/dietphysicalactivity/en/]
- Sally Lovelace, Fatemeh Rabiee-Khan (2013) Food choices made by low-income households when feeding their pre-school children: a qualitative study. Maternal and Child Nutrition.
- Birch LL (1998) Development of food acceptance patterns in the first years of life.Proc Nutr Soc57: 617-624. [Crossref]
- Larsen JK, Hermans RC, Sleddens EF, Engels RC, Fisher JO, et al. (2015) How parental dietary behaviour and food parenting practices affect children's dietary behaviour. Interacting sources of influence? 89: 246-257 [Crossref]
- Reicks M, Randall JL, Haynes BJ (1994) Factors affecting consumption of fruit and vegetables by low-income families. J Am Diet Assoc 94: 1309-1311. [Crossref]
- O’Neill M, Rebane D, Lester C (2004) Barriers to healthier eating in a disadvantaged community. Health Education Journal 63: 220-228.
- Department of Health and Social care (2005) Research governance framework for health and social care. Second edition.
- Beauchamp T and Childress J (2001) Principles of Biomedical Ethics. 5th edition Oxford: Oxford University Press.
- Quick Calcs (2018). [https://www.graphpad.com/quickcalcs/confInterval1/]
- Cooley MC (2008) Nurses' motivations for studying third level post-registration nursing programmes and the effects of studying on their personal and work lives.Nurse Educ Today28: 588-594. [Crossref]
- Rabiee F (2004) Focus-group interview and data analysis.Proc Nutr Soc63: 655-660. [Crossref]
- Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC et al. (2008) A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act5: 56 [Crossref]
- Haun J, Luther S, Dodd V, Donaldson P (2012) Measurement Variation Across Health Literacy Assessments: Implications for Assessment Selection in Research and Practice J Health Commun 3: 141-159. [Crossref]
- Public Health England (2015) A guide to community-centred approaches for health and wellbeing. Briefing.[https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/402889/A_guide_to_community-centred_approaches_for_health_and_wellbeing briefi.pdf]
- National Institute of Health & Care Excellence (2014) Maternal and child nutrition. NICE Guidelines. London.
- Rabiee F, Robbins A, Khan M (2015) Gym for Free: The Short-Term Impact of an Innovative Public Health Policy on the Health and Wellbeing of Residents in a Deprived Constituency in Birmingham, UK. Health Education Journal 74: 691-704.
- Gallant MP (2003) The influence of social support on chronic illness self-management: a review and directions for research.Health Educ Behav30: 170-195. [Crossref]
- Michie S, van Stralen MM, West R (2011) The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 6: 42. [Crossref]
- Iris Vermeir, Wim Verbeke (2008) Sustainable food consumption among young adults in Belgium: theory of planned behaviour and the role of confidence and values. Ecological Economics 64: 542-553.
- Cade J (2008) The Low-Income Diet and Nutrition Survey: Implications for Relationships between Diet and Disease. Proceedings of the Nutritional Society. Satellite symposium 67: E89.
- Carey G, Crammond B (2015) Systems change for the social determinants of health.BMC Public Health15: 662. [Crossref]
- Mitchell GL, Farrow C, Haycraft E, Meyer C (2013) Parental influences on children’s eating behaviour and characteristics of successful parent-focussed interventions. Appetite 60: 85-94. [Crossref]
- Sanders MR, Mazzucchelli TG (2017) The Power of Positive Parenting: Transforming the Lives of Children, Parents and Communities- Using the Triple P System. Oxford Press. ISBN 9780190629069.
- Darnton-Hill I, Nishida C, James WP (2004) A life course approach to diet, nutrition and the prevention of chronic diseases.Public Health Nutr7: 101-121. [Crossref]