Abstract
Objectives: Investigations involving the influence of patient expectations on clinical outcomes are gaining popularity in the literature. Our purpose was to determine if 1) expectations about an intervention change after the intervention has been applied and 2) those changes in expectation are related to pain-related outcomes.
Methods: Ninety healthy volunteers were randomized to thoracic spinal manipulation (SMT), cranio-cervical flexion exercise (CCF), or no intervention (control) and then provided with a picture of the intervention. Pain sensitivity was assessed using thermal quantitative sensory testing using standardized methods for assessing patients with pain-related conditions. Participants then rated their expectation of pain-relief before the intervention (pre-intervention expectation). Immediately after the intervention, participants again rated their expectation for pain relief (post-intervention expectation) and pain sensitivity was assessed again. Proportions of participants expecting less, same or more pain were compared among intervention groups and pre- and post-intervention. The influence of expectations was examined by building separate regression models.
Results: Before the intervention was performed a greater than expected proportion of participants in the control group expected more pain after the intervention than in both the SMT and CF groups. These proportion of participants changed AFTER the intervention. More participants in the control group expected the same pain after lying quietly, than expected more or less pain. In both intervention groups the number expecting ‘more pain’ decreased and the number expecting the ‘same pain’ increased. There was no influence of expectation on the results for temporal summation. However, for single suprathreshold responses, there were main effects for pre-intervention expectation (people expecting more pain reported more pain before and after intervention) and interactions for post-intervention expectations and time; that is, people expecting less pain had less pain during post-intervention testing.
Discussion: These results suggest several things relevant to clinical practice. First, expectations changed within one treatment session even without the usual clinical contextual cues thought to be necessary for this to occur. Next, pre-interventions appear to be related to overall pain reporting and may represent a very general influence on outcomes. Post-intervention expectations were more significant predictors of the pain reported by participants during the post-test suggesting temporal salience and intrinsic judgment about the impact of the intervention.
Key words
post-intervention hypoalgesia, Pain sensitivity, cranio-cervical flexion exercise, thoracic spinal manipulation
Introduction
In the context of rehabilitation, patients’ expectations accompany all aspects of care from the choice of provider to the interventions preferred. In the specific case of interventions for pain, expectations are associated with clinical outcomes. For example, in a study of patients seeking care for low back pain from providers such as physicians, chiropractors, acupuncturists, and massage therapists, the expectation for improvement, independent of provider, was associated with improvements in disability [1]. Expectations also have a strong association with recovery in patients with spinal disorders [2,3]. Collectively, these findings support an association between clinical outcomes and expectations. Less well established is whether expectations change during an episode of healthcare. Confirmation of this would provide an opportunity to optimize treatment effects through enhanced communication between the clinician and patient aimed at leveraging expectations.
In a prior study, we compared the effects of two interventions for neck pain [4] on pain. The results showed differences between intervention effects on dynamic pain sensitivity. Subsequent work suggests that patients’ specific expectations for pain relief might outweigh the effects of type of intervention provided. The analysis we had performed for the prior study had not considered patient expectations on the effects of the interventions. In this current analysis, we test this using the data from that prior study examining the extent that measures of pain sensitivity were affected by expectation.
Consequently, our first goal was to determine whether an expectation regarding the effects of an intervention for pain changes after the intervention has been applied. The second goal was to examine whether expectations? held before, or after, the intervention impact the final outcome of that intervention.
Materials and Methods
The current study is a secondary analysis of a data from a study of the effect of common interventions for neck pain on pain sensitivity. The protocol and results of the primary study are provided in detail elsewhere [4].
Participants
Ninety participants (mean age 22.9 ± 2.7 years, 66 women) were recruited for the primary study between 2009 and 2010. Inclusion criteria for this study were: 1) between 18-35 years of age and 2) no neck or upper-extremity complaints within the past sixty days. Exclusion criteria for this study were: 1) identification of any medical signs and/or symptoms suggesting systemic dysfunction, 2) history of whiplash-type injury within 60 days of initial examination, 3) previous spinal or upper-extremity surgical interventions, 4) regular use of analgesic or anti-inflammatory drugs (within past 48 hours). All participants read and signed the informed consent form approved by the Institutional Review Board. As part of the informed consent process participants were told 1) the purpose of the study was to determine whether certain interventions used by physical therapists affect painful sensations, 2) the studied interventions are used in patients presenting with painful conditions in the neck and upper back, 3) the study was being performed in pain free individuals to determine if the interventions affected mild pain produced in the research setting, and 4) the interventions would be overseen by a licensed physical therapist.
Measures
Demographics: Participants completed a demographic survey that included information about their education, prior pain experiences and prior experience with the interventions used in this study.
Psychological Questionnaires: In the original study we measured several psychological factors given the reported influences of these constructs on pain intensity in experimental models of pain [5]; fear of pain (FPQ) [6], Tampa Scale of Kinesiophobia – General Population (TSK-G) [7], and Pain Catastrophizing Scale (PCS) [8]. There were post-randomization differences in the PCS among groups, but the PCS was not correlated with any of the outcomes and was, therefore, not included in any further modeling.
Experimental Pain Sensitivity: We used thermal stimuli to determine experimental pain sensitivity in arm and leg.
All thermal stimuli were delivered to the skin of participants using a computer-controlled Medoc Neurosensory Analyzer (TSA-2001, Ramat Yishai, Israel). Stimulation sites were varied to prevent carryover effects due to local sensitization. We had both a male and female examiner present during testing to account for sex and/or gender influence on pain reporting [9]. Before each testing session, participants underwent a practice session. During this session participants experienced the entire range of temperatures to which they were to be exposed. Participants practiced using the numeric rating scale (NRS) anchored at 0 (no pain sensation at all) and 100 (worst pain imaginable) to rate the intensity of the first and second pain experienced in response to each stimulus. A standardized instructional set was used for all participants during every exposure to the thermal stimuli.
First pain: Thermal stimuli of 5 seconds duration were applied to the volar forearm (cervical innervated region) and to the posterior surface of the upper calf below the popliteal fossa (lumbar innervated region), with the subject in a sitting position. The participants experienced a sequence of four thermal pulses that included 45ºC, 47ºC, 49ºC, or 51°C presented randomly.
Participants were cued to provide a rating of any pain experienced immediately after the peak of each thermal pulse using the NRS. This procedure was performed twice, and the average of both trials was used in subsequent analyses. The inter-stimulus interval was at least 60 seconds to avoid carryover effects from one stimulus to another, to prevent changes in receptor responses and to prevent tissue changes. Temperature levels were monitored by a contactor-contained thermistor and returned to a preset baseline of 35°C by active cooling at a rate of 10°C.sec-1 [10,11].
Temporal sensory summation (TSS): A train of 10 heat pulses peaking at 50ºC was applied to the glabrous skin of the hand and foot. Temperature levels returned to a preset baseline by active cooling at a rate of 10ºC.sec-1. The participants were asked to rate the magnitude of their delayed or “second” pain sensation following each of the 10 heat pulses using the same NRS. The increase in the second pain intensity rating that occurs from early to later inputs is referred to as TSS. The phenomenon is believed to be primarily C-fiber mediated [10]. We used a simple slope measure in our analyses.
Interventions
Participants were randomly assigned to one of three intervention groups: 1) High velocity, low amplitude intervention (SMT), 2) specific cervical exercise (CF) or, 3) control group.
The SMT group received an intervention commonly used for patients with cervical disorders and has been shown to be effective in reducing pain and self-report of disability [12]. The technique was performed with the subject in the supine position. The subject clasped their hands behind their neck and brought their elbows together in front of their chest. One hand of the physical therapist was placed on the upper thoracic region and the other on the participants’ elbows. The force application was directed through the participants’ elbows. The technique was applied two times in concordance with clinical literature related to the technique. This technique is hypothesized to affect the lower cervical and upper thoracic region.
The CF group performed a common exercise used for patients with cervical disorders that has been reported to be associated with immediate reductions in cervical pain. The movement involves flexion of the cranium on the cervical spine while ensuring the back of the head remains in contact with the supporting surface [13]. The subject was asked to perform three sets of ten repetitions with a five second hold at a sub-maximal (<25%) effort.
The control group rested quietly in supine for five minutes.
Expectations for hypoalgesia: This construct was measured in two ways. First, prior to randomization but after pain sensitivity testing, participants were provided with a picture of the interventions (i.e., SMT, CF, and control) and asked to complete a 1-item, 3-point Likert scale survey (more pain, same pain, less pain) about their expectation for pain in response to the thermal pain sensitivity testing following the intervention. These were considered the pre-intervention expectations.
Second, participants repeated the Likert scale survey about their expectation for lower-extremity hypoalgesia immediately following the application of the intervention (i.e., SMT, CF, control) but before the repeat thermal pain testing. These were considered the post-intervention expectations?
Analysis
Demographic variables were compared among intervention groups using one-way analyses of variance (ANOVA) with t-tests for post-hoc comparisons of group means from continuous parametric and Mann-Whitney U and Chi-squared for non-parametric data. For first pain responses, data for 45°C and 51°C were not analyzed because these represented sub-threshold and tolerance values for a majority of patients, respectively [14-16].
Associations among pre- and post-intervention expectations, and group assignment were assessed using chi-squares. When a significant chi-square was found we used standardized residuals and comparisons of proportions were used to identify influential cells. In addition, we determined the proportions of participants in each group whose expectations improved (expected ‘more pain’ pre-intervention and expected ‘same’ or ‘less’ pain post-intervention) or worsened.
We used three-way mixed model ANOVAs to examine changes in each of the primary QST outcome variables (first pain, TSS) for this study. We built three sets of models for each of the outcome variables. Model 1 included only the factors for time and limb; In Model 2, pre-intervention expectations was added as a covariate; and Model 3, pre-interventions expectations were removed, and post-intervention expectations were added.
This was done to allow us to determine first, if the addition of expectations improved the quality of the models and second, which expectation had a greater influence on the final outcome. For each model, the between subject’s factor was group (SMT, CCF, control) and there were two within subject factors: time (pre, post) and body region (upper extremity, lower extremity). Consistent with the primary study other variables (e.g. psychological or demographic factors) different among groups post-randomization and associated with the outcomes were included as covariates. Any significant interactions were followed using two-way or one-way ANOVA as indicated. Pair-wise comparisons were made using t-tests, and Type 1 error was maintained at 5% using Bonferroni corrections. All analysis was performed using SPSS 24 (SPSS Inc, Chicago, IL).
Results
Ninety people (average age 22.8 (2.53); 66 women) volunteered for this study and completed the informed consent process. All 90 completed the study. Demographic data are shown in Table 1.
Table 1. Participant characteristics.
| | SMT | Exercise | Control | p-value |
Demographic factors |
Age (years) | 23.03 ± 2.44 | 23.03 ± 2.95 | 22.47 ± 2.21 | 0.61 |
Sex (number female) | 19 | 22 | 25 | 0.22 |
Psychological factors |
Anxiety (ASI) | 15.37 ± 6.42 | 15.03 ± 6.38 | 18.47 ± 8.70 | 0.14 |
Fear of pain (FPQ-9) | 12.93 ± 4.39 | 14.20 ± 3.89 | 14.03 ± 3.59 | 0.14 |
Catastrophizing (PCS) | 15.83 ± 9.77 | 13.63 ± 8.87 | 19.60 ± 7.38 | 0.03 |
Kinesiophobia (TSK-G) | 19.70 ± 4.00 | 19.63 ± 4.93 | 20.90 ± 4.34 | 0.46 |
Pre-intervention expectation |
Less pain | 8 | 3 | 5 | |
Same pain | 19 | 23 | 14 | |
More pain | 3 | 4 | 11 | |
Post-intervention expectation |
Less pain | 8 | 6 | 3 | |
Same pain | 22 | 24 | 21 | |
More pain | 0 | 0 | 6 | |
Changes in expectations for hypoalgesia
A significant difference among the intervention groups was noted pre-intervention (i.e. before randomization; χ2=10.89, p=0.028) in which there was a greater than expected proportion of participants randomly assigned to the control group who expected more pain after the intervention than in both the SMT and CF groups. Additionally, fewer individuals assigned to the control group expected the same pain when compared to the CF group. These proportion of participants changed AFTER the intervention but there remained a significant difference in frequencies of responses (χ2=14.44, p=0.006). This effect was still primarily driven by more participants in the control group expecting more pain than in the other two groups. However, the patterns of change in each group were different. The number of individuals expecting less pain decreased in the control group, as did the number expecting more pain; i.e. more participants in the control group expected the same pain after lying quietly, than expected more or less pain. In both intervention groups the number expecting more pain decreased and the number expecting the same pain increased. Specifically, 16% in SMT, 26% in CF and 23% in control had improved expectations for pain relief after intervention. Approximately 10% of participants had worse expectations post-intervention in each group.
Effect of expectation on pain sensitivity
First pain 47oC: The baseline model included main effects for time (F2,87=41.8, η2=0.25, p<0.001) and limb (F2,87=8.23, η2=0.11, p=0.005). No additional effects were noted (consistent with the primary study analysis).
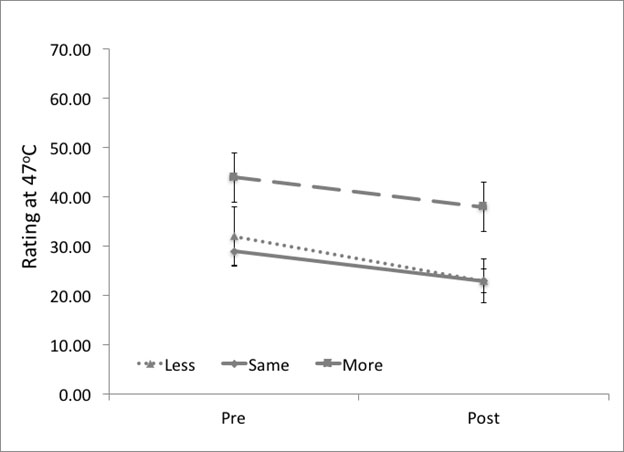
Including pre-intervention expectations resulted in only an effect for time (F2,86=15.12, η2=0.18, p<0.001) but there was no main effect for limb (F1,86=0.11, η2<0.01, p=0.739). Rather a main effect for expectation (F1,86=4.82, η2=0.09, p=0.031) was significant changing the interpretation of the model. This effect resulted from higher average pain ratings (across both pre and post intervention testing sessions) in the participants expecting ‘more pain’ than ‘less pain’ (p=0.006) (Figure 1).
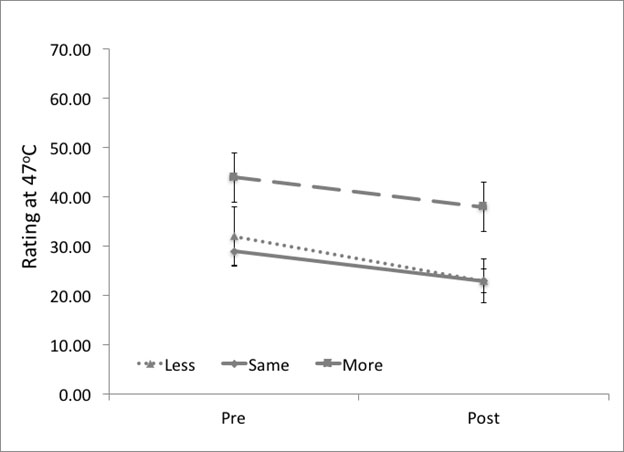
Figure 1. The effect of interaction between time and post-intervention expectations on ratings of pain during testing at 47oC. Participants expecting ‘less’ or ‘same’ pain reported significantly less pain during post-intervention testing (p<0.001). There was no difference in rating of pain before or after the intervention for participants expecting ‘more’ pain.
The inclusion of post-intervention expectations resulted in a significant interaction between time and post-intervention expectations (F1,86=4.12, η2=0.08, p=0.045). Here there was significant reductions in reported pain after the intervention for the ‘less pain’ and ‘same pain’ groups (p<0.001 for both) but not for the ‘more pain’ group (p=0.131). No other effects were noted (Figure 1).
First pain 49oC: The baseline model only included a significant main effect for time (F1,87=21.12, η2=0.20, p<0.001). No other effects were noted.
The addition of pre-intervention expectations resulted in a main effect for time was significant (F1,87=13.97 η2=0.14, p<0.001), and a main effect for pre-intervention expectations (F1,87=4.83, η2=0.05, p<0.031) changing the interpretation of the effect of the interventions. Similar to what observed at 470C, participants expecting more pain rated pain during QST higher than those expecting less (p=0.022).
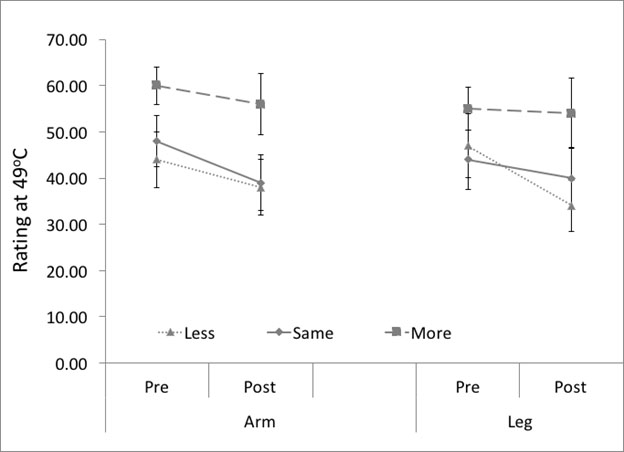
However, in contrast to 470C, in the inclusion of post-intervention expectations changed the interpretation of model again. In this model only the time*limb*post-intervention expectation (F2,87=8.71, η2=0.07, p=0.016) was significant. Decomposition of this effect indicated that participants with expectations for less pain, reported significantly less pain in the leg but not the arm (Figure 2).
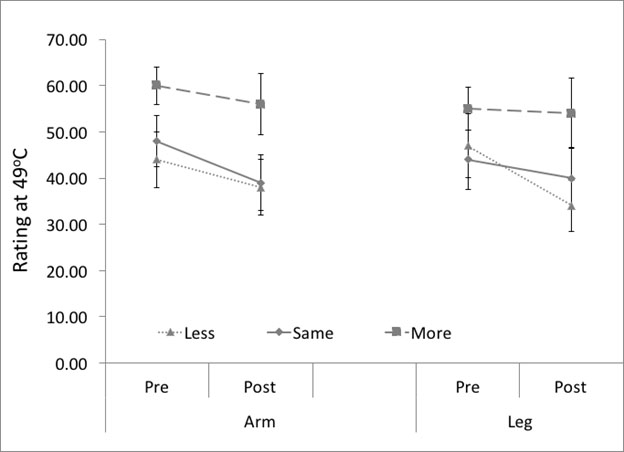
Figure 2. The effect of interaction between time, post-intervention expectations and limb on ratings of pain during testing at 49oC. Participants expecting ‘less’ pain reported significantly less pain at the leg post-intervention compared to participants expecting ‘more’.
Temporal Sensory Summation
The baseline model for TSS indicated a significant time*group interaction (F2,87=5.43, η2=0.11, p=0.006) and a significant main effect for limb (F1,87=6.97, η2=0.07, p=0.010). The interaction occurred due to a larger decrease in TSS after SMT compared to the other groups. Adding pre-intervention expectations did not change the primary interpretation of the model. The time*group interaction remained significant (F2,87=5.83, η2=0.12, p=0.004) although the limb effect disappeared. There was no interaction term that included pre-intervention expectations nor was there a significant main effect. Similarly, the inclusion of post-intervention expectations did not modify the time*group interaction (F2,87=5.27, η2=0.11, p=0.007), and post-intervention expectations were not part of any significant interactions nor were main effects identified.
Post-hoc sample size calculations
To examine the extent to which our findings were influenced by the restriction of using previously collected data (i.e. were important findings were not identified because the analysis was under powered we calculated required sample sizes based on the effect sizes from the current analysis. To identify a significant interaction effect including pre- or post-intervention expectations with 80% power for responses at 470C we would have needed to enroll and test a minimum 708 people. Similarly, identifying a significant interaction effect including pre- or post-intervention expectations with 80% power for temporal summation we would have needed to enroll and test a minimum 518 people. Given these large required numbers and the fact that we did identify significant interactions we remain confident that the results represent meaningful findings.
Discussion
Our goals in this current study were to determine whether expectations for pain relief change after an intervention has been applied, and if pre- or post-interventions differed in the influence on outcome.
Our results indicate that not only do expectations change rapidly within a treatment session but the expectations that develop immediately after the first intervention may have a larger impact than those with which the individual initially presents. The manner in which the expectations changed, however, was not how we had expected. We had speculated that participant’s receiving an active intervention would expect less pain after experiencing it than they did beforehand and certainly more so than the no intervention control. These findings may have potentially been influenced by our healthy pain free sample. Patients frequently seek healthcare with high expectations for the effectiveness of treatment [17]. This did not appear to be the case for our healthy sample where only 18% indicated expecting to have less pain in response to the studied interventions pre- randomization. Expectations may differ based on the number of study arms and the wording of the informed consent process. For example, antidepressants demonstrate greater effectiveness in studies of active comparators as compared to placebo-controlled studies [18]. Participants in studies with an active comparison were twice as likely to respond and one and one-half times as likely to experience remission as participants in a traditional placebo-controlled study of depression. Such findings are attributed to expectation as participants are aware in this study design they will receive an active intervention as compared to a placebo control study in which participants are aware of a 50% chance of receiving a placebo. Similarly, the magnitude of placebo analgesia increases when studies include unbalanced randomization (i.e. a lower than 50% likelihood of receiving a placebo treatment) [19]. Our participants were aware through the consent process of the possibility of receiving no intervention. Subsequently, this could explain the pre- randomization lower expectations for treatment success than is generally observed in clinical care where patients present with the expectation of receiving treatment. Subsequently, we cannot speculate if these directional changes in expectation would be similar for participants seeking care for clinical pain conditions. The statistical difference in the broad group comparisons was predominantly driven by a larger proportion of the control group expecting ‘more pain’ both pre- and post-intervention. The greater than expected proportion of participants in the control group who expected more pain after the intervention in comparison to the SMT and CF groups was not completely surprising and potentially suggests that awareness of receiving an active intervention (i.e., SMT or CF) alone influence likelihood for positive expectations. However, when we examined the individual changes more closely, equivalent numbers in each group both improved, and worsened, in the expectation for pain after the intervention. This finding suggests that expectations change within a treatment session for some people. This is similar to work studying recovery expectations in patients with low back pain by Kamper, et al. [20] that suggests while expectations remained constant over time for the majority of patients, 20% of patients reported changes in expectations (improved and worsened) over the course of treatment. Although the directional changes in expectations were unexpected, our findings provide support that expectations do change providing an opportunity for these to be modified through enhanced patient-provider communication to optimize treatment effects.
Including expectations (pre or post-intervention) for pain relief caused no changes in the interpretation of the influence of SMT on dynamic pain sensitivity; strengthening the findings of the original study. Specifically, SMT has consistently been shown to decrease temporal summation of pain, and in the original study we had concluded that SMT had a general effect on temporal summation. That this finding was unchanged when participant expectations were included in the present study suggests hypoalgesic effects of SMT may represent a finding separate from the additive effects of expectation and placebo. This is supported by other work by our group in which SMT caused greater changes in temporal summation than both placebo SMT or enhanced placebo SMT suggesting effect beyond expectations for SMT in participants with low back pain [21].
There were, however, significant main effects and interactions involving expectations that impacted the findings related to first pain responses. These are the responses that that represent sharp pain in response to a single suprathreshold stimulus. At both stimulus intensities, we identified a significant main effect for pre-intervention expectations. Pre-intervention expectations were collected after the first pain sensitivity test and before the intervention and focused specifically on pain the participant would experience after the intervention. The main effect of pre-intervention expectation was a result of participants expecting more pain reporting statistically higher pain intensity before AND after the intervention. One possible interpretation is that this represents a potential ‘trait’; i.e. the participant would tend to always report higher pain intensity. However, there were no associations between the pre-intervention expectations and measures of negative affect often associated with higher reports of pain intensity in studies that have used similar experimental pain protocols; e.g. fear of pain or pain catastrophising. An alternative explanation may be that participants who expect ‘less pain’ have better efficacy or optimism, measures we unfortunately did not collect in this study.
In contrast, significant interactions were identified that included post-intervention expectations and time at both stimulus intensities (i.e. differing changes in pain pre to post intervention based on an individual’s expectations immediately following treatment). Our previous work and that of others that have showed the pre-intervention expectations measured during the patient’s initial examination are related to mid to long-term outcomes. We suggest, based on this, that expectations are fluid and need to be assessed several times early during an episode of care particularly when the intervention in question is administered during successive treatment sessions.
The finding that pre-intervention expectation did not affect the immediate response to an intervention, but post-intervention did is similar to other work [22] that showed expectations collected before treatment for low back pain were not significantly associated with back pain intensity at 6 weeks. However, the expectations measured after treatment began were strongly related to pain intensity at 6- and 12-weeks. Another comparable result was reported in a study of acupuncture for patients with chronic back pain [23]. In that study, pretreatment expectation was not a significant predictor of improvement in back-related symptoms or function at 8 or 52 weeks. However, after 5 treatments, revised expectation of success was predictive of both symptoms and function at 8 and 52 weeks.
Furthermore, there was a three-way interaction at 49oC. In this interaction, participants expecting less pain, reported less pain at the calf during post-intervention testing. Our finding of a somatospecific nature of expectations is consistent with studies from the placebo literature. For example, an analgesic effect was isolated to half of the forearm in a study of sham acupuncture [24].
The primary caveat to the interpretation of these results is that this study was performed in pain-free people using pain sensitivity (i.e. experimentally induced pain) as the outcome. Although the design of this current study may not be directly translatable to clinical settings, we identified that the act of receiving a commonly provided intervention (of any type in this study) was associated with modified expectations for pain relief in some participants, which does provide important implications for clinical practice. All participants in our study received a standard instruction set that did not include any contextual information about the potentially beneficial changes for pain relief beyond ‘commonly used to treat pain’. The context in which the intervention is provided has been shown to profoundly influence pain relief. Additionally, the application of the intervention without context resulted in both improved and worsened expectations highlighting the importance of the patient-provider interaction and education/informed consent process prior to treatment.
Our prior work has indicated that expectations can be manipulated experimentally with instructional set (i.e negative or positive instructions result in associated negative or positive expectations) [25,26] and this manipulation affects hyper- or hypoalgesia after intervention implying that the language and descriptions used by the provider can dramatically impact the subsequent outcomes. Those preliminary findings, along with others from our group, warrant further investigation to determine the extent to which enhanced communication provided by clinicians can enhance patient expectations and how this impacts management of pain by rehabilitation, consistent with recent suggestions [27]. Additionally, the recent systematic review by Nickel, et al. [28] concluded that varying the terminology used to describe a condition influences patient preferences and evidence suggests that healthcare providers can learn to improve communication skills in this domain Linton et al. [29].
Conclusion
Collectively, our findings support the importance of routine and ongoing assessment of patient expectations for an intervention for neck pain. Moreover, assessment of expectations should be distinctly aligned with clear operational definitions (e.g., pain intensity, bothersomeness, disability) to distinguish between outcome domains of interest.
References
- Myers SS, Phillips RS, Davis RB, Cherkin DC, Legedza A, et al. (2008) Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med 23: 148-153. [crossref]
- Bishop MD, Mintken PE, Bialosky JE, Cleland JA (2013) Patient expectations of benefit from interventions for neck pain and resulting influence on outcomes. J Orthop Sports Phys Ther 43:457-65. [crossref]
- Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA (2001) Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine (Phila Pa 1976) 26: 1418-1424. [crossref]
- Bishop MD, Beneciuk JM, George SZ (2011) Immediate reduction in temporal sensory summation after thoracic spinal manipulation. Spine J 11: 440-446. [crossref]
- George SZ, Dannecker EA, Robinson ME (2005) Fear of pain, not pain catastrophizing, predicts acute pain intensity, but neither factor predicts tolerance or blood pressure reactivity: An experimental investigation in pain-free individuals. Eur J Pain 10: 457-465. [crossref]
- McNeil DW, Rainwater AJ 3rd (1998) Development of the Fear of Pain Questionnaire--III. J Behav Med 21: 389-410. [crossref]
- Houben RM, Leeuw M, Vlaeyen JW, Goubert L, Picavet HS (2005) Fear of movement/injury in the general population: factor structure and psychometric properties of an adapted version of the Tampa Scale for Kinesiophobia. J Behav Med 28: 415-424. [crossref]
- Kapoor S, Thorn BE, Bandy O, Clements KL (2015) Pain referents used to respond to the pain catastrophizing scale. Eur J Pain 19: 400-407. [crossref]
- Robinson ME, Wise EA, Gagnon C, Fillingim RB, Price DD (2004) Influences of gender role and anxiety on sex differences in temporal summation of pain. J Pain 5: 77-82. [crossref]
- Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD (2001) Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. Pain 91: 165-175. [crossref]
- Wright A, Graven-Nielsen T, Davies II, Arendt-Nielsen L (2002) Temporal summation of pain from skin, muscle and joint following nociceptive ultrasonic stimulation in humans. Exp Brain Res 144: 475-482.
- Price DD, Bennett GJ, Rafii A (1989) Psychophysical observations on patients with neuropathic pain relieved by a sympathetic block. Pain 36: 273-288. [crossref]
- Staud R, Cannon RC, Mauderli AP, Robinson ME, Price DD, et al. (2003) Temporal summation of pain from mechanical stimulation of muscle tissue in normal controls and subjects with fibromyalgia syndrome. Pain 102: 87-95. [crossref]
- Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL (2007) Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther 87: 09-23. [crossref]
- O'Leary S, Falla D, Hodges PW, Jull G, Vicenzino B (2007) Specific therapeutic exercise of the neck induces immediate local hypoalgesia. J Pain 8: 832-839. [crossref]
- Bialosky JE, Bishop MD, Robinson ME, Barabas JA, George SZ (2008) The influence of expectation on spinal manipulation induced hypoalgesia: an experimental study in normal subjects. BMC Musculoskelet Disord 9:19. [crossref]
- Bialosky JE, Bishop MD, Robinson ME, Zeppieri GJ, George SZ (2009) The Immediate Effects of Spinal Manipulative Therapy on Thermal Pain Sensitivity in Participants with Low Back Pain: A Randomized, Controlled Trial. Phys Ther 89.
- George SZ, Bishop MD, Bialosky JE, Zeppieri GJ, Robinson ME (2006) Immediate effects of spinal manipulation on thermal pain sensitivity: an experimental study. BMC Musculoskel Disord 7: 68. [crossref]
- Zeppieri G Jr, George SZ (2017) Patient-defined desired outcome, success criteria, and expectation in outpatient physical therapy: a longitudinal assessment. Health Qual Life Outcomes 15: 29. [crossref]
- Rutherford BR, Sneed JR, Roose SP (2009) Does study design influence outcome? The effects of placebo control and treatment duration in antidepressant trials. Psychother Psychosom 78: 172-181. [crossref]
- Diener HC, Dowson AJ, Ferrari M, Nappi G, Tfelt-Hansen P (1999) Unbalanced randomization influences placebo response: scientific versus ethical issues around the use of placebo in migraine trials. Cephalalgia 19: 699-700. [crossref]
- Kamper SJ, Kongsted A, Haanstra TM, Hestbaek L (2015) Do recovery expectations change over time? Eur Spine J 24: 218-226.
- Bialosky JE, George SZ, Horn ME, Price DD, Staud R, et al. (2014) Spinal manipulative therapy-specific changes in pain sensitivity in individuals with low back pain (NCT01168999). J Pain15: 136-148. [crossref]
- Haas M, Vavrek D, Neradilek MB, Polissar N (2014) A path analysis of the effects of the doctor-patient encounter and expectancy in an open-label randomized trial of spinal manipulation for the care of low back pain. BMC Complement Altern Med 14:16. [crossref]
- Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Delaney K, et al. (2010) Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine 35: 1471-1477. [crossref]
- Kong J, Kaptchuk TJ, Polich G, Kirsch I, Vangel M, et al. (2009) An fMRI study on the interaction and dissociation between expectation of pain relief and acupuncture treatment. NeuroImage 47: 1066-1076. [crossref]
- Department of Health and Human Services. National Pain Strategy: A Comprehensive Population Health Strategy for Pain. 2016.
- Nickel B, Barratt A, Copp T, Moynihan R, McCaffery K (2017) Words do matter: a systematic review on how different terminology for the same condition influences management preferences. BMJ Open 7: e014129. [crossref]
- Linton SJ, Flink IK, Nilsson E, Edlund SL (2017) Can training in empathetic validation improve medical students' communication with patients suffering pain? A test of concept. Pain Rep 2: e600. [crossref]