Purpose: We evaluated the efficacy of secondary treatment in patients with temporomandibular disorders (TMD), who did not show significant improvement with initial treatment combined with patient education, therapeutic exercises, manual therapy, cognitive behavior therapy, and management of head position and posture.
Procedures (observational study): In six patients, the treatment methods and the later processes during secondary treatment were evaluated. Four patients received pharmacological therapy with central muscle relaxants, one patient received a combination of pharmacological and stabilization splint therapy, and one patient received splint therapy as an additional treatment modality.
Results: Four cases showed improvement in symptoms and incidental symptoms, and two cases showed improvement in symptoms after splint therapy. In the case treated with combination of pharmacological and splint therapy, the improvement in pain was obtained due to splint therapy; this confirmed that situations wherein splint therapy can be required after failure of rehabilitation therapy may exist, even though most randomized control trials have revealed no additional benefits of splints in rehabilitation.
Conclusion: We concluded that additional treatment using pharmacological or splint therapy should be considered appropriate options, if rehabilitation does not provide adequate results.
temporomandibular disorders, secondary treatment, rehabilitation, medicine, splint
Rehabilitation therapy has been accepted as an effective treatment modality for temporomandibular disorders (TMD) [1]. It involves basic patient education, exercise therapy, and cognitive behavior therapy (CBT) to reduce masticatory muscle tension and psychological problems. Some reviews have suggested the efficacy of exercise therapy and CBT [2-7].
A randomized control trial (RCT) conducted by our team showed that multimodal therapy (MMT) combined with exercise therapy and habit control is as effective or might even be better than stabilization splint therapy [8,9]. In accordance with these results, we utilized MMT as the primary treatment modality in patients with TMD because of its safety and low cost. However, all RCTs, including our study, have compared two or more treatment groups, and hence, the conclusions obtained from these studies might not be true for individual patients. Some patients might actually require additional modalities of treatments after completion of MMT because of the lack of sufficient therapeutic result. Therefore, the necessity and methods of secondary treatment modalities should be considered, if MMT does not yield adequate treatment results.
In this study, we report secondary treatment modalities that should be considered for patients in whom MMT does not lead to significant improvement.
This study was approved by the Ethical Review Board of our Hospital (ECG-H-33).
Eight-five patients diagnosed with TMD based on the diagnostic criteria for temporomandibular disorders (DC/TMD) and treated only with MMT from 2009 to 2015 were included in the study to examine the efficacy of splint therapy [8,10] (Table 1).
Table 1. Patients treated with secondary treatment
Case |
Sex |
Age |
Chief complaint |
DC/TMD diagnosis |
1 |
Female |
48 |
TMJ pain, limited mouth opening |
Myalgia, Arthralgia, DD/woR, DJD |
2 |
Female |
65 |
TMJ pain, limited mouth opening |
Arthralgia |
3 |
Male |
54 |
TMJ pain, limited mouth opening |
Arthralgia, DD/wR |
4 |
Female |
14 |
TMJ pain |
Arthralgia, DD/woR |
5 |
Female |
14 |
TMJ pain, limited mouth opening |
Myalgia, Arthralgia, DD/wR |
6 |
Male |
20 |
TMJ sounds |
Myalgia, DD/wR |
DD/woR: Disc displacement without reduction; DJD: Degenerative Joint Disorder; DD/wR: Disc displacement with reduction; DC/TMD: Diagnostic criteria for temporomandibular disorders; TMJ: Temporomandibular joint
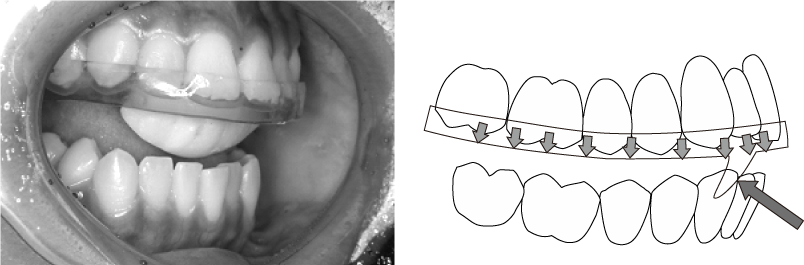
MMT included patient education regarding TMD, self-exercises such as pulling the last molars downward by the fingers in synchronization with patient’s opening movements, and CBT to reduce mental stress and bruxism. Moreover, manual therapy with ‘jog-manipulation’ was applied in the patients with limited mouth opening [9] (Figure 1).
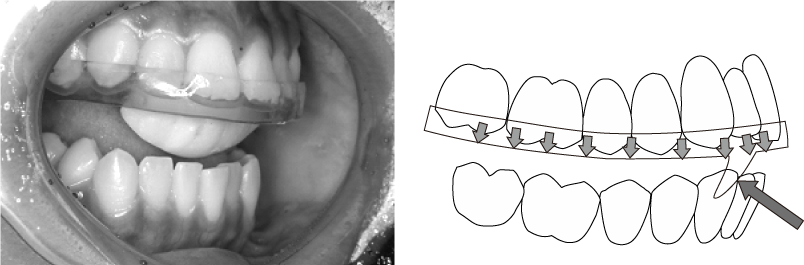
Figure 1. Stabilization splint with grinding control to prevent bruxism
The exclusion criteria of the study were patients that did not provide written informed consent, patients unable to comply with the regular recall visits every two or four weeks, and/or patients with psychological disorders requiring medications.
Of the 85 patients, 74 patients showed sufficient improvement, and 11 patients showed insufficient improvement in symptoms after completion of MMT. Of these, six patients received secondary treatment. The remaining three patients discontinued their treatments before sufficient improvement was evident, and two patients with a chief complaint of TMJ sounds did not consent for secondary treatment.
Evaluation parameters
The distance between the maxillary and mandibular medial incisor at autonomous maximum mouth-opening with bearable pain measured by a caliper (MMO), orofacial pain measured using the numerical rating scale with values assigned from 0 to 10 (PainNRS), and temporomandibular joint (TMJ) sounds (SoundNRS) were accessed to evaluate the therapeutic effects of primary and secondary treatments.
The assessment periods were before treatment, after treatment at first visit, and every two weeks thereafter. Secondary treatments were initiated after 2-3 sessions of MMT proved insufficiently effective, and patients agreed for additional treatment. Regarding patients with TMJ sounds, many patients complained of persistent TMJ sounds after completion of MMT. Hence, patients with the only complaint of TMJ sounds were selected. All the patients who accepted secondary treatment were instructed to continue MMT during secondary treatment.
Treatment methods
The secondary treatment included prescription of centrally acting muscle relaxants (Eperisone Hydrochloride, Chlorphenesin Carbamate, Tizanidine Hydrochloride) and/or use of stabilization splint during sleep. The treatment selection was based on the patient’s condition and request. The selection criteria for a particular treatment was as follows: muscle relaxants were used in patients with muscle and/or TMJ tenderness by palpation according to the DC/TMD criteria; splints were used in patients who complained of TMJ sounds or symptoms after waking up. However, unless the patients did not consent for drugs, pharmacological therapy was prioritized because of its simplicity and low cost.
The stabilization splint was fabricated on the maxillary teeth, and all the teeth were in contact. Anterior guiding plate was not included in the splint in the first appointment. If the symptoms did not improve, a bruxism controller that prevented eccentric movements of the mandible was added (Figure 1).
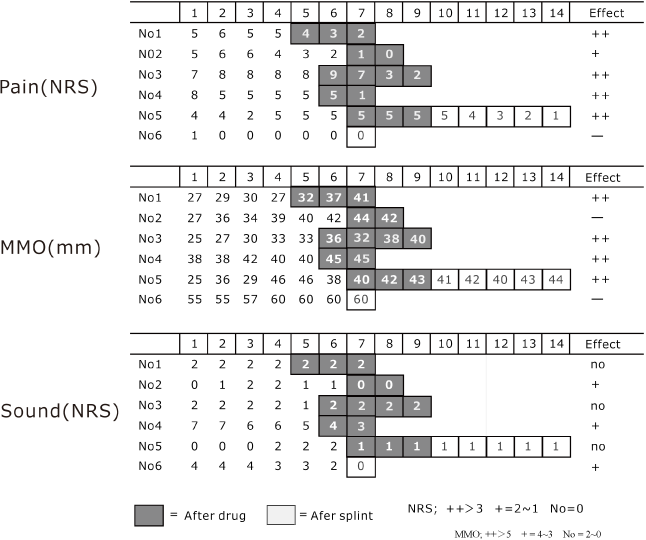
Figure 2 shows the schedule of treatment, and Table 2 shows the results of secondary treatment. Pharmacological therapy was used in four cases, combination therapy (pharmacological and splint) in one, and splint therapy was used in the remaining case.
Table 2. Results of secondary treatment
Case |
Treatment method |
Effects of secondary treatment |
Pain |
MMO |
Sound |
Total |
1 |
Medicine (EH+CC) |
++ |
+ |
No |
B |
2 |
Medicine (EH+CC) |
+ |
- |
+ |
A |
3 |
Medicine (EH+CC) |
++ |
++ |
no |
B |
4 |
Medicine (EH+CC) |
++ |
++ |
+ |
A |
5 |
Medicine (EH+CC) |
++ |
++ |
no |
B |
6 |
Medicine (TH), Splint |
- |
- |
+ |
A |
MMO: autonomous maximum mouth-opening; EH: Eperisone Hydrochloride, CC: Chlorphenesin Carbamate, TH: Tizanidine Hydrochloride
++: effective, +: slightly effective, no: ineffective, -: no-effect
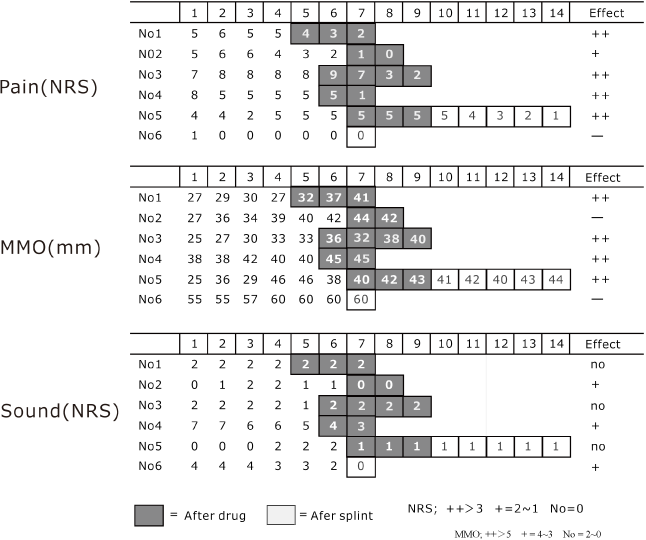
Figure 2. Diagram showing the transition of symptoms due to initial and secondary treatments. Pain improved in four cases after pharmacological therapy. Case 5 did not improve after pharmacological therapy but improved after splint therapy. Maximum mouth opening improved in four cases after pharmacological therapy. Temporomandibular joint sounds improved in only three cases after pharmacological or splint therapy
Pain improved in four out of five patients after secondary treatment. One patient showed limited improvement. MMO improved in all patients. Temporomandibular joint sounds decreased in three out of six patients. The estimate of total effects is that three cases were A (all symptoms improved), three cases were B (Temporomandibular joint sounds did not improve).
Of the five cases that complained of pain, four patients showed improvement after pharmacological therapy (treatment was effective in four patients and slightly effective in one patient). One case showed no improvement with pharmacological therapy but showed improvement with additional splint therapy.
The MMO was less than 40 mm in four cases and increased by more than 5 mm after secondary treatment. Of the three parameters tested, TMJ sounds showed the least improvement. Three cases showed slight improvement on the NRS scale, while the remaining three cases showed no improvement. On the whole, secondary treatment showed considerable effects except for TMJ sounds.
Selection of secondary treatment
Rehabilitation therapy for TMD includes many treatment methods: basic patient education, habit control through CBT, therapeutic exercises performed by the patient and manual therapy (such as manipulation) executed by the practitioner, massage for the masticatory muscles, and correction of improper head positions and postures. Each treatment does not use some specific equipment or material, it is generally referred as conservative treatment (CT). CT is usually a combination of several treatments, and MMT is a type of CT.
In contrast, treatment that utilizes specific equipment or drugs, such as splints, drugs, biofeedback, and acupuncture, can be termed as extensional treatment (ET), if CT is assumed the standard treatment.
A practitioner may choose CT or ET or a combination of both for initial treatment, depending on the theory and his/her clinical experiences. Secondary treatment can be altered depending on the type of primary treatment chosen. Therefore, validity for the use of CT as a primary treatment modality should be known before determining the type of secondary treatment.
Several RCTs have compared the efficacy of CT and ET as a primary treatment modality. Two types of RCTs were conducted. One investigated the additional effect of ET while CT was used as standard treatment. The other used only CT or ET as initial treatment, and compared CT and ET directly.
Some RCTs conducted the former type of investigation, i.e., examined the efficacy of splint therapy combined with standard treatment modalities such as exercise or patient education.
Conflicting results were obtained from these studies; some RCTs revealed no additional therapeutic effects of splints, while some others showed limited additional therapeutic effects [8-16]. However, the RCT conducted by Costa showed that additional effects of splints were observed in patients wherein only education for patients was used as standard treatment [16]. Therefore, it can be considered a study with untreated controls.
Four RCTs conducted the latter type of study, i.e., compared directly the efficacy of splint therapy and CT. Of these, three concluded that results obtained from additional patient education and exercise were superior to the results obtained from splint therapy alone [17-19]. One RCT showed that habit control is as effective as splint therapy [20]. Many systematic reviews of splint therapy have shown the efficacy of untreating or non-contact splints in the treatment of TMDs, but superiority to other treatments could not be proved [21-26].
To summarize, the superiority of ET over CT has not been confirmed. Therefore, CT is reasonable choice for initial treatment because of its low cost, safety, and long-term effects.
In our study, MMT was effective as an initial treatment modality in 87.1% (95% CI = 78.7-94.4%) patients [8]. Therefore, we concluded that MMT was appropriate and effective as an initial treatment modality.
Results of the secondary treatment
Pharmacological treatment was the secondary mode of treatment in case 1 ~ case 5. Of the five patients that complained of pain, three recovered completely, and one showed limited recovery. All four patients that complained of limited mouth-opening recovered completely. Of the six patients that complained of TMJ sounds, three showed limited recovery, while three did not show any evidence of recovery. Therefore, additional medications such as central muscle relaxants were considered effective for secondary treatment excepted with TMJ sounds. However, the results pertaining to pain cannot be considered completely valid, as the number of subjects was too small to confirm the effect (the improvement ratio was 60%; 95% CI = 27.6 ~ 92.7).
Interestingly, case 5 did not show response to pharmacological therapy but showed considerable response to splint therapy. Case 6 reported that TMD sounds disappeared due to the splint. The improvement was considered a result of splint therapy; this confirmed that cases wherein splint therapy can be validated as a secondary treatment modality after failure of rehabilitation therapy. In our RCT, we had concluded that additional splint therapy did not show any benefits over MMT [8]. These results do not agree with the conditions of case 5 and case 6. However, our RCT compared two treatment groups. Hence, some exceptions can be expected depending on individual patient condition. The existence of such exceptions should be noted when applying the results of RCTs to clinical practice.
Based on these results, we conclude that additional treatment in the form of pharmacological or splint therapy can be considered appropriate in patients wherein CT did not lead to significant improvement, even though most RCTs have reported no additional benefits of splint therapy in the rehabilitation of such patients.
These cases treated using secondary treatment modalities did show varying degrees of improvement with initial treatment in the form of MMT. Some cases also revealed a certain degree of improvement, even if significant improvement was not achieved.
Hence, MMT was continued throughout the secondary treatment. Thus, the therapeutic effect of pharmacological or splint therapy obtained in this study should be determined as a combined effect, which included the effects obtained through MMT. Most RCTs have analyzed the initial treatment modalities for TMD. Unfortunately, few reports have documented the results from secondary treatment when initial treatment did not achieve desired results. Reliable assessments of secondary treatment modalities are necessary in the future, based on evidence-based medicine.
The efficacy of secondary treatment was evaluated in six patients, who did not show significant improvement with rehabilitation therapy. Four patients were treated using central muscle relaxants, one patient using a combination of pharmacological and stabilization splint therapy, and one patient was treated using splint therapy as an additional treatment modality.
Four cases showed improvement in symptoms and in incidental symptoms after pharmacological therapy, two cases showed improvement in symptoms after splint therapy. In the cases treated with splint therapy, the improvements obtained were due to splint therapy, even though most RCTs have revealed no additional effects of splints in rehabilitation. Based on these results, we conclude that additional secondary treatment with pharmacological or splint therapy can be considered appropriate in patients wherein rehabilitation therapy did not yield significant results.
There is no declarations of interest to report.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
- Lindfors E, Arima T, Baad-Hansen L, Bakke M, De Laat A, et al. (2019) Jaw Exercises in the Treatment of Temporomandibular Disorders-An International Modified Delphi Study.J Oral Facial Pain Headache33: 389-398. [Crossref]
- Medlicott MS, Harris SR (2006) A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther 86: 955-973. [Crossref]
- Moraes Ada R, Sanches ML, Ribeiro EC, Guimaraes AS (2013) Therapeutic exercises for the control of temporomandibular disorders. Dental Press J Orthod 18: 134-139. [Crossref]
- Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, et al. (2016) Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis.Phys Ther96: 9-25. [Crossref]
- Butts R, Dunning J, Pavkovich R, Mettille J, Mourad F (2017) Conservative management of temporomandibular dysfunction: A literature review with implications for clinical practice guidelines (Narrative review part 2).J Bodyw Mov Ther21: 541-548. [Crossref]
- Shimada, Ishigaki S, Matsuka Y, Komiyama O, Torisu T, et al. (2019) Effects of exercise therapy on painful temporomandibular disorders.J Oral Rehabil46: 475-481. [Crossref]
- Aggarwal VR, Tickle M, Javidi H, Peters S (2010) Reviewing the evidence: can cognitive behavioral therapy improve outcomes for patients with chronic orofacial pain? J Orofac Pain 24: 163-171. [Crossref]
- Nagata K, Maruyama H, Mizuhashi R, Morita S, Hori S, et al. (2015) Efficacy of stabilisation splint therapy combined with non-splint multimodal therapy for treating RDC/TMD axis I patients: a randomised controlled trial. J Oral Rehabil 42: 890-899. [Crossref]
- Nagata K, Hori S, Mizuhashi R, Yokoe T, Atsumi Y, et al. (2019) Efficacy of mandibular manipulation technique for temporomandibular disorders patients with mouth opening limitation: a randomized controlled trial for comparison with improved multimodal therapy.J Prosthodont Res63: 202-209. [Crossref]
- Michelotti A, Alstergren P, Goulet JP, Lobbezoo F, Ohrbach R, et al. (2016) Next steps in development of the diagnostic criteria for temporomandibular disorders (DC/TMD): Recommendations from the International RDC/TMD Consortium Network workshop. J Oral Rehabil 43: 453-467. [Crossref]
- Truelove E, Huggins KH, Mancl L, Dworkin SF (2006) The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc 137: 1099-1107. [Crossref]
- Niemelä K, Korpela M, Raustia A, Ylöstalo P, Sipilä K (2012) Efficacy of stabilisation splint treatment on temporomandibular disorders.J Oral Rehabil39: 799-804. [Crossref]
- Katyayan PA, Katyayan MK, Shah RJ, Patel G (2014) Efficacy of appliance therapy on temporomandibular disorder related facial pain and mandibular mobility: a randomized controlled study. J Indian Prosthodont Soc 14: 251-261. [Crossref]
- Qvintus V, Suominen AL, Huttunen J, Raustia A, Ylöstalo P, et al. (2015) Efficacy of stabilisation splint treatment on facial pain - 1-year follow-up.J Oral Rehabil42: 439-446. [Crossref]
- Ficnar T, Middelberg C, Rademacher B, Hessling S, Koch R, et al. (2013) Evaluation of the effectiveness of a semi-finished occlusal appliance--a randomized, controlled clinical trial.Head Face Med9: 5. [Crossref]
- Costa YM, Porporatti AL, Stuginski-Barbosa J, Bonjardim LR, Conti PC (2015) Additional effect of occlusal splints on the improvement of psychological aspects in temporomandibular disorder subjects: A randomized controlled trial. Arch Oral Biol 60: 738-744. [Crossref]
- Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M (2012) Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles.J Am Dent Assoc143: 47-53. [Crossref]
- Haketa T, Kino K, Sugisaki M, Takaoka M, Ohta T (2010) Randomized clinical trial of treatment for TMJ disc displacement.J Dent Res89: 1259-1263. [Crossref]
- van Grootel RJ, Buchner R, Wismeijer D, van der Glas HW (2017) Towards an optimal therapy strategy for myogenous TMD, physiotherapy compared with occlusal splint therapy in an RCT with therapy-and-patient-specific treatment durations. BMC Musculoskelet Disord 18: 76. [Crossref]
- Glaros AG, Kim-Weroha N, Lausten L, Franklin KL (2007) Comparison of habit reversal and a behaviorally-modified dental treatment for temporomandibular disorders: a pilot investigation. Appl Psychophysiol Biofeedback 32: 149-154. [Crossref]
- Al-Ani MZ, Davies SJ, Gray RJ, Sloan P, Glenny AM (2004) Stabilisation splint therapy for temporomandibular pain dysfunction syndrome.Cochrane Database Syst Rev CD002778. [Crossref]
- Turp JC, Komine F, Hugger A (2004) Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig 8: 179-195. [Crossref]
- Fricton J, Look JO, Wright E, Alencar FG Jr, Chen H, et al. (2010) Systematic review and meta-analysis of randomized controlled trials evaluating intraoral orthopedic appliances for temporomandibular disorders. J Orofac Pain 24: 237-254. [Crossref]
- Ebrahim S, Montoya L, Busse JW, Carrasco-Labra A, Guyatt GH, et al. (2012) The effectiveness of splint therapy in patients with temporomandibular disorders: a systematic review and meta-analysis. J Am Dent Assoc 143: 847-857. [Crossref]
- Zhang C, Wu JY, Deng DL, He BY, Tao Y, et al. (2016) Efficacy of splint therapy for the management of temporomandibular disorders: a meta-analysis. Oncotarget 7: 84043-84053. [Crossref]
- Eliassen M, Hjortsjö C, Olsen-Bergem H, Bjørnland T (2019) Self-exercise programmes and occlusal splints in the treatment of TMD-related myalgia-Evidence-based medicine?J Oral Rehabil46: 1088-1094. [Crossref]