Abstract
Background: A laparotomy sponge, pad or gauze unintentionally retained in a patient after surgery is known as a gossypiboma. Due to the complications associated with gossypibomas and the measures that have been put in place to prevent their occurrence, gossypibomas are now considered ‘never’ events in surgery. We present a case of delayed diagnosis of gossypiboma following emergency Caesarean section performed at another facility.
Case presentation: A 25-year-old female presented to us with a painful abdominal mass 17 months following an emergency caesarean section performed for poor progress in labour at another facility. A contrast enhanced computed tomography scan revealed a loculated intraperitoneal mass with bubbles, thin enhancing capsule and calcifications suggestive of a gossypiboma. The patient underwent exploratory laparotomy with findings of a small bowel tumour. An intraluminal laparotomy sponge was found in the specimen after resection.
Conclusion: Timely and accurate diagnosis of gossypibomas requires a high index of suspicion together with good clinical examination and careful interpretation of radiological images. Prevention requires vigilance and strict adherence to safety protocols in the operating room.
Keywords
gossypiboma, retained surgical items, delayed diagnosis, intraluminal sponge
Introduction
Items unintentionally forgotten in a patient after surgery are known as retained surgical items (RSI). One of the most commonly forgotten items is gauze pieces and laparotomy sponges or pads [1]. A sponge forgotten in the surgical field is called a gossypiboma or textiloma. Gossypibomas are extremely rare, with a reported incidence of around 0.3 – 1.0/1000 abdominal surgeries [2]. However, it is most likely that occurrences are under-reported due to medicolegal and socio-cultural reasons [3].
Many factors can contribute to sponge retention during surgery, including emergency surgery, long surgical procedures or an unexpected change in the surgical procedure, poor communication, hurried sponge counts, change of teams during the procedure, unstable patient condition, obesity and inadequate or inexperienced staff members [4]. The sites where sponges and other items are most often forgotten are the abdomen (56%), pelvis (18%) and the thorax (11%) [2]. However, no body cavity is spared from retained foreign body after surgery.
The time from the index surgery to the diagnosis of a gossypiboma can vary considerably. While some are diagnosed shortly after surgery, others may take months or years to diagnose. Delays of more than 40 years have been reported in the medical literature [5]. In a Polish case series, the average time to diagnosis was 17 months [6]. Most patients present with vague symptoms like non-specific abdominal pain and malaise, making diagnosis difficult. A high index of suspicion together with judicious clinical exam and imaging like plain radiographs, ultrasound or computed tomography (CT) scan are helpful in making a correct diagnosis [7].
In operating room (OR) settings, RSIs constitute serious adverse or ‘never’ events and are a significant breach of surgical safety culture [8]. They can have grave consequences for patients including chronic debilitating abdominal pain, intra-abdominal abscesses, bowel obstruction, perforation and gastrointestinal fistulas. Most of these complications often require surgical intervention. In addition, forgetting a surgical item inside a patient indicates poor quality of care, and may lead to medico-legal consequences including huge monetary compensations by the hospital to the victim.
As a standard procedure to prevent RSIs, instrument and sponge counts are performed by the scrub nurse before and immediately after surgery, just before the surgical site is closed. This is to ensure that all items are accounted for and nothing is left behind in the patient. Despite the implementation of counting protocols and other important measures like the WHO safety checklist, RSIs still happen, with up to 88% occurring when the sponge and instrument counts have been declared correct [2]. This underscores the need for continuous vigilance and strict adherence to established counting procedures and checklists by all members of the operating team so as to prevent such adverse events.
We report the case of a young woman who underwent laparotomy at our hospital for a painful abdominal mass and an intraluminal gossypiboma was found more than a year after caesarean section.
Case presentation
A 25-year-old female, married with 2 children and with no known comorbidities was brought to our emergency department with a history of abdominal pain and vomiting. The patient reported constant generalized abdominal pain that had been present for 1 year and 5 months. Two months prior to presentation at our hospital, the patient had started to experience non-bilious spontaneous vomiting, about 2 to 3 episodes a day. The patient had lost a lot of weight during this period, dropping from 75 to 35 kg (40 kg weight loss in 1 year). Before coming to us, the patient had consulted in many other hospitals, had unremarkable ultrasound scans and ended up being managed for pain caused by intra-abdominal adhesions.
The patient surgical history was significant for 2 previous Caesarean sections, both of which were indicated for poor progress in labour. The patient current symptoms started after the second Caesarean section 17 months ago. On arrival, the patient was in shock with blood pressure of 90/50 mmHg and heart rate of 120 bpm. The patient temperature was 36.5°C, respiratory rate 20 breaths/minute and oxygen saturation of 96% on room air. The patient blood glucose was 120 mg/dl.
The patient looked chronically sick, pale and cachectic. Her weight was 35 kg and BMI 16 kg/m2. There was no peripheral adenopathy. Chest exam was within normal limits. The patient abdomen looked asymmetrically distended and there was a transverse scar across the suprapubic area. There was a palpable 6 cm periumbilical intra-abdominal mass which was mildly tender and mobile in all directions. The patient did not have any signs of peritonitis. Digital rectal and vaginal exams were unremarkable.
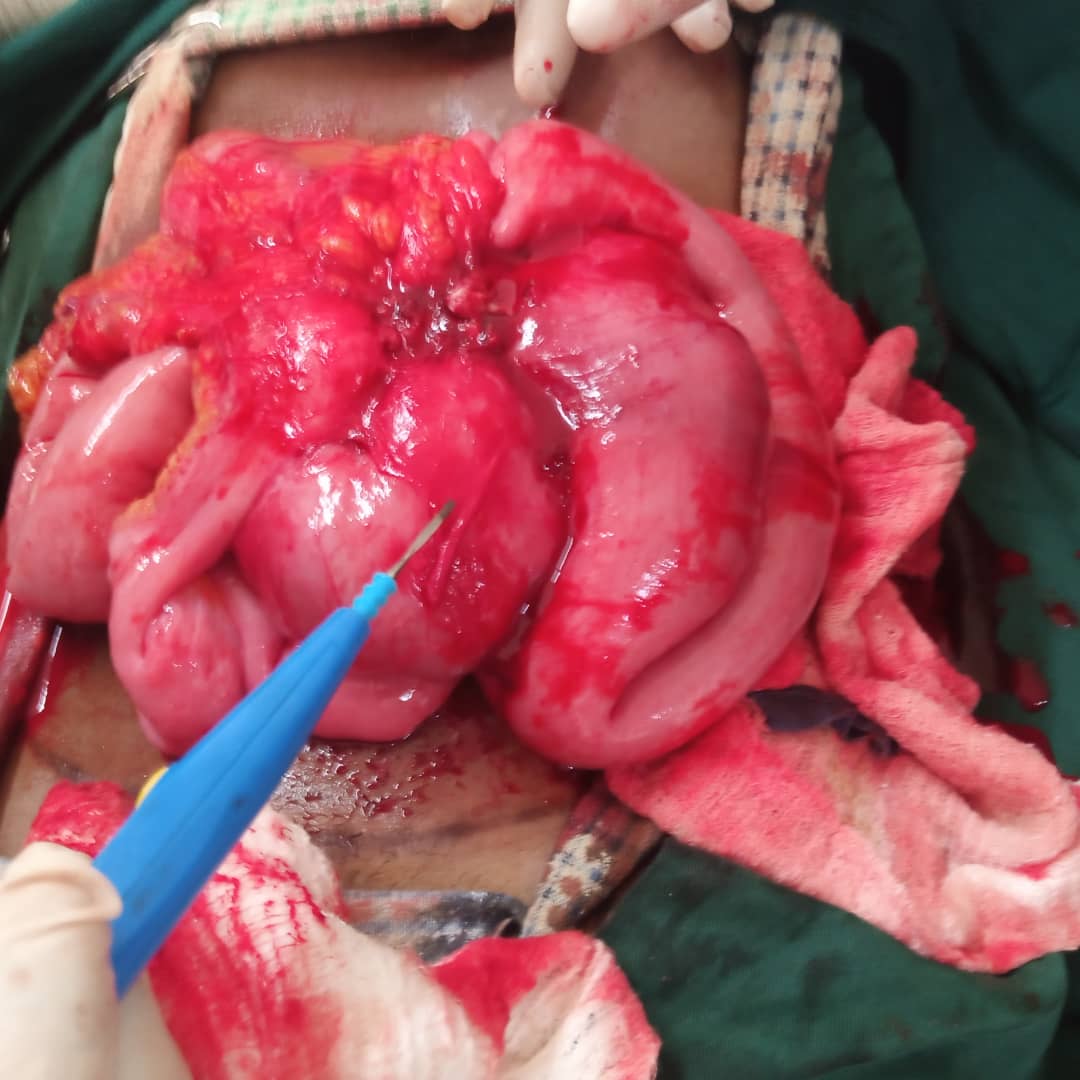
The patient white blood cell count was 9.9 × 10^3/uL, haemoglobin 9.4 mg/dl and platelet count of 230 × 10^3/uL. The patient blood urea nitrogen and serum creatinine were 10.65 and 0.51 mg/dl respectively. Mild hyponatremia was present (Na 130 mmol/L) along with hypochloraemia (Cl 95 mmol/L) and normal potassium level (K 3.8 mmol/L). Patient serum albumin was 1.5 g/dl. HIV test was negative. Following resuscitation with IV fluids, we performed an abdominal ultrasound that confirmed the presence of a periumbilical complex mass and suggested further evaluation with a CT scan. A contrast enhanced CT scan was performed and revealed a loculated intraperitoneal mass with gas bubbles, enhancing capsule and calcifications, associated with moderate ascites (Figure 1). The most likely diagnosis on CT scan was a gossypiboma with a differential diagnosis of a bezoar.
We admitted the patient, crossmatched blood and obtained consent for an exploratory laparotomy after adequate preoperative optimization. Since patient nutritional status was so poor, part of our plan included refeeding the patient and administering immunonutrition for at least 5 days prior to surgery, but abdominal pain and vomiting worsened prompting us to perform the laparotomy 3 days after admission.
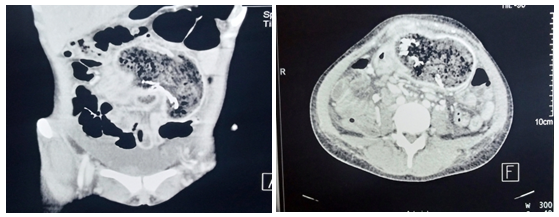
Figure 1. Contrast enhanced computed tomography, Coronal and axial views showing loculated low-density intraperitoneal mass with gas bubbles with a thin enhancing capsule and calcifications in close proximity with loops of small bowel; findings likely suggestive of gossypiboma
Intraoperatively, we found a 10 cm mass about 5 cm from the ileocaecal junction. The mass included tightly matted loops of small bowel and a portion of the circumference of the mid transverse colon. About 4 m of small bowel proximal to the mass looked normal. There were multiple enlarged mesenteric lymph nodes, making us suspect the possibility of malignancy. It was impossible to separate the small bowel loops, hence we did en bloc resection of the mass followed by a side-to-side ileum to ascending colon anastomosis. After detaching the transverse colon from the mass, we had a 1 cm enterotomy that we primarily repaired. The patient was transfused 1 unit of blood intra-operatively (Figure 2).
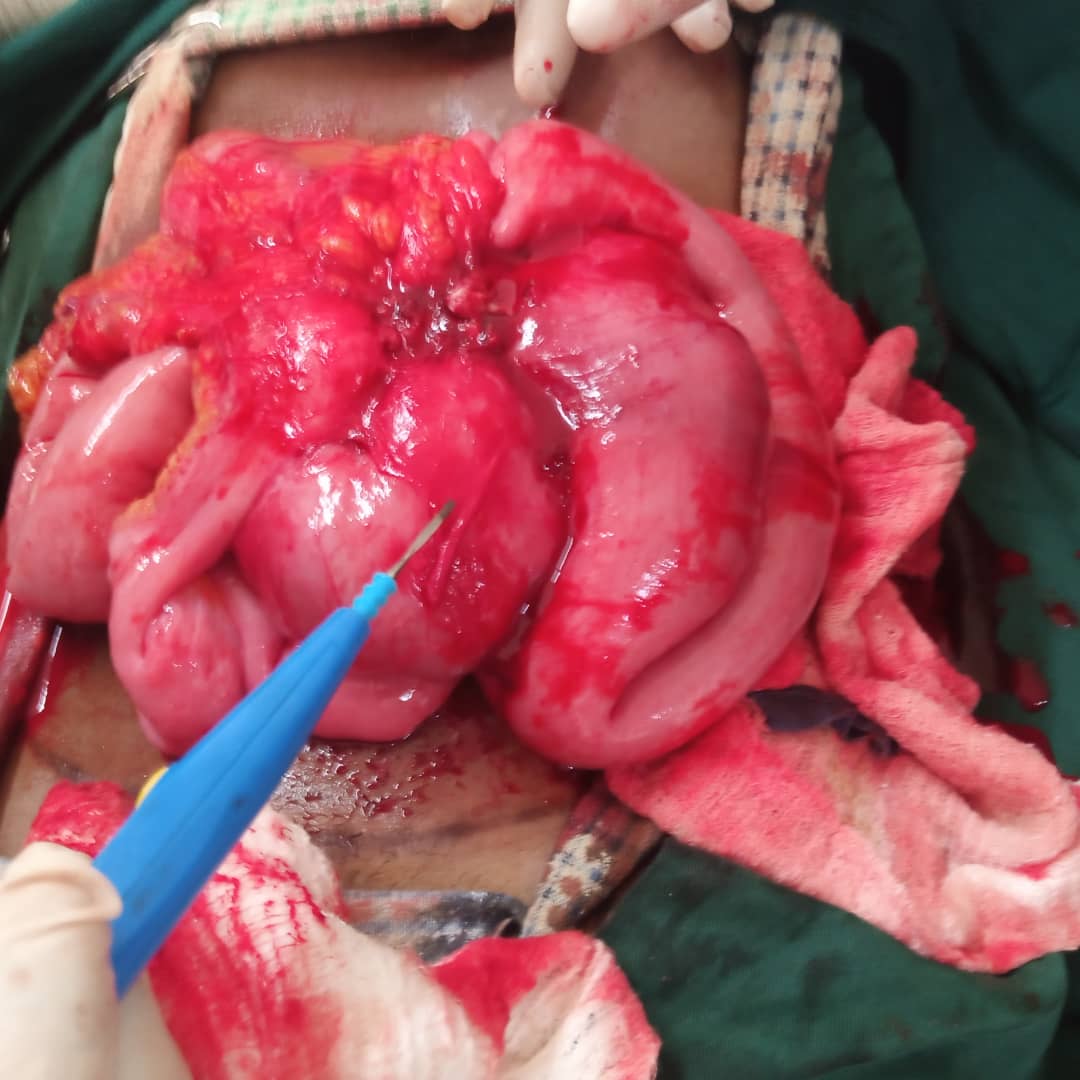
Figure 2. Intraoperative finding of inflammatory mass involving terminal ileum with dense adhesions of small bowel loops preventing separation
Opening the resected specimen on the back table revealed an intraluminal laparotomy sponge. No perforations were found on the resected bowel. The bowel specimen was then sent for histopathological examination. Patient postoperative course was complicated by surgical site infection and an intra-abdominal collection that required percutaneous drainage. The patient recovered well from the procedures and was subsequently discharged on postoperative day 16. The histopathology report came out several weeks later confirming the presence of a sponge and absence of malignancy in the surgical specimen (Figure 3).
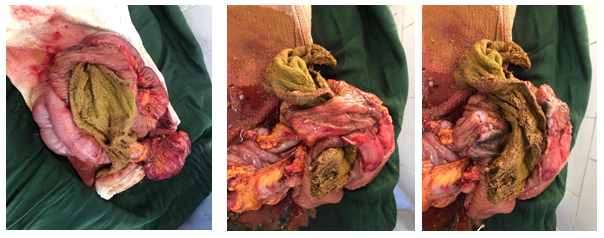
Figure 3. Resected specimen reveals intraluminal gossypiboma
Results and discussion
Gossypibomas and other retained surgical items are regarded as “never” events in surgery [1]. They carry significant medicolegal implications and indicate medical negligence and poor quality of care. They are and should be rare occurrences given that several measures including surgical counts and surgical safety checklists have been put in place to prevent these events. Having a case like this one in the year 2025 raises questions about the widespread and effective use of surgical safety checklists like the WHO checklist as well as other sponge counting procedures and technology. If these systems are failing, why are they failing and what are the barriers health care providers are facing in effectively implementing these measures?
One of the major challenges faced by clinicians in managing gossypibomas is delayed diagnosis. For our patient, the time interval from the index Caesarean section to diagnosis was 1.5 years. Only 40% of gossypibomas are found within the first year of surgery while up to 50% are discovered 5 or more years later [9]. While acute cases may present with features of infection or obstruction and are more easily detected, chronic ones may mimic tumours making diagnosis more challenging [10]. Radiological investigations like X-ray and CT scan are quite sensitive in picking up gossypibomas [11]. Plain radiographs may show curved and banded radio-opaque lines while on CT scan, gossypibomas may appear as cystic lesions with internal spongiform appearance with bubbles, hyperdense capsule and mottled mural calcifications [4]. In low resource settings like ours, good imaging facilities may not always be available and qualified radiologists are scarce. Furthermore, there is limited access to sponges with radio-opaque markers which limits detection by CT scan and other imaging modalities [12]. In our case, it took several months for the patient to be referred to a facility with a CT scanner and an experienced Radiologist. Thus to make an accurate and timely diagnosis, clinical examination and radiological findings must be combined with an increased awareness of the possibility of a retained sponge in patients who have had prior surgery [7].
For this patient, we performed a midline laparotomy and did a bowel resection and anastomosis. Most cases of gossypibomas reported in the literature were also managed by open surgery and required bowel resection and anastomosis [13]. In a case reported by Kundan, et al. a laparotomy was performed and the sponge was extracted via an enterotomy without resecting bowel [14]. Their patient presented only 3 months after surgery, preoperative diagnosis of intraluminal gossipyboma was well established on CT scan and the surgeons encountered less inflammatory changes in the abdomen. Neeraj, et al. successfully retrieved a gossypiboma using laparoscopy in a patient who presented 6 months after the index surgery [15]. This contrasts with the traditional approach to gossypibomas which has been open surgery due to the belief that intense foreign body reaction and dense adhesions around the sponge may make the laparoscopic approach difficult. Laparoscopy offers multiple advantages including less postoperative pain, fewer surgical site infections, and shorter length of hospital stay, faster recovery, quicker return to work and activities of daily living as well as superior cosmesis. However, given that our patient was more than a year out of the index surgery and was chronically deconditioned, we anticipated adhesions and a more “hostile” abdomen that would make laparoscopy technically challenging.
The sponge we found was completely intraluminal. This phenomenon has been described in case reports from other parts of the world. In the abdomen, a gossypiboma provokes an intense inflammatory response. Omentum and bowel loops surround and attempt to encapsulate the sponge, leading to irritation and necrosis of the intestinal wall which then permits the sponge to erode partially or completely into the bowel lumen [16].
Increased incidences of gossypibomas have been reported after emergency surgical procedures like the Caesarean section which our patient had [9]. Lower pelvic surgeries, obesity, unstable patient condition and an unexpected change in the intended surgical procedure are other factors that have been implicated in gossypibomas. Instrument and sponge counts as well as various checklists like the WHO safety checklist are some measures which have been implemented to prevent RSIs. Unfortunately, most cases of retained surgical sponges have occurred after a documented correct sponge count [17]. This calls for vigilance from all team members involved in the operation and the need to double check counts so as to minimize error.
Conclusion
Gossypibomas are preventable surgical events with significant impacts on both the patient and the health care team. Their diagnosis requires high index of suspicion, good clinical exam and careful interpretation of imaging results. Early diagnosis and treatment leads to better outcomes, hence physicians in hospitals without adequate facilities should maintain awareness of this diagnosis and ensure prompt referral of patients to better equipped centres where they can be properly investigated and managed. Close vigilance as well as strict adherence to surgical counts and safety checklists is necessary to prevent gossypibomas.
Informed consent
Consent: Written informed consent for the publication of this case report was obtained from the patient. All images involved were used with consent from the patient.
Conflicts of interest
There is no conflict of interest among the authors regarding this case report.
References
- Tchangai B, Tchaou M, Kassegne I, Simlawo K (2017) Incidence, root cause, and outcomes of unintentionally retained intraabdominal surgical sponges: A retrospective case series from two hospitals in Togo. Patient Saf Surg11: 25. [Crossref]
- Kanani J, Sheikh MI (2024) Undiagnosed, uncomplicated foreign body in abdominal cavity – A case of medical negligence. Surg Case Rep 2: 100024.
- Irabor DO (2012) Under-reporting of gossypiboma in a third-world country. A sociocultural view. Health 4: 56-59.
- Lata I, Kapoor D, Sahu S (2011) Gossypiboma, a rare cause of acute abdomen: A case report and review of literature. Int J Crit Illn Inj Sci 1: 157. [Crossref]
- Parra M, Oppliger F, Berríos R, Schiappacasse G (2015) Intrathoracic gossypiboma presenting 52 years later as a chest mass. Asian Cardiovasc Thorac Ann 23: 596-598. [Crossref]
- Modrzejewski A, Kowalik K, Grochal I, Kaźmierczak K (2022) Surgical materials retained in the abdomen after surgery. Pol J Surg 95:30-33.
- Mefire AC, Tchounzou R, Guifo ML, Fokou M, Pagbe JJ, et al. (2009) Retained sponge after abdominal surgery: experience from a third world country. Pan Afr Med J 2: 10. [Crossref]
- Sirihorachai R, Saylor KM, Manojlovich M (2022) Interventions for the Prevention of Retained Surgical Items: A Systematic Review. World J Surg 46: 370-381. [Crossref]
- Youshko, Facog D, Patel N, Dikmen S, Sirsi Facs S, et al. (2022) Gossypiboma: an asymptomatic presentation ten years post gynecologic surgery. Obstet Gynecol Int J 13: 218-220.
- Naiem MEA, Suliman SH, Elgurashi MEA, Arabi NA, Mohammedkhair AAA, et al. (2021) Small bowel obstruction and ileocolic fistula caused by post-myomectomy Gossypiboma transmural migration: A case report and review of the literature. Int J Surg Case Rep 87: 106431. [Crossref]
- Srivastava KN, Agarwal A (2014) Gossypiboma posing as a diagnostic dilemma: A case report and review of the literature. Case Rep Surg 2014: 1-3. [Crossref]
- Agada H, Malgwa Ishaku Y, Iliya J (2024) Bowel obstruction from complete transmural migration of a gossypiboma into the ileum; a rare occurrence: Acute bowel obstruction from gossypiboma. Med J Zambia 50: 292-295.
- Ukweh ON, Akpan SO, Ntamu CO, Enang ME, Ekpo KO, et al. (2024) Gossypiboma: A case of retained intra-luminal surgical sponge leading to delayed diagnosis and treatment in a Nigerian patient. SAGE Open Med Case Rep 12: 2050313X241272732. [Crossref]
- Patil K, Patil S, Gorad K, Panchal A, Arora S, et al. (2010) Intraluminal migration of surgical sponge: Gossypiboma. Saudi J Gastroenterol 16: 221. [Crossref]
- Saxena N, Kardam DK, Chauhan R, Chaudhary T (2021) Gossypiboma - Successful retrieval through laparoscopy: A case report. Int J Surg Case Rep 84: 106109. [Crossref]
- Aminian A (2008) Gossypiboma: A case report. Cases J 1: 220. [Crossref]
- Kaiser CW, Friedman S, Spurling KP, Slowick T, Kaiser HA, et al. (1996) The retained surgical sponge. Ann Surg 224: 79-84. [Crossref]