Hand-foot-and-mouth disease (HFMD) is a common viral illness generally affecting the pediatric population. It usually manifests as a febrile illness with papules and vesicles on the oral mucosa, buttocks, hands and feet. The primary cause is an enterovirus, most commonly Coxsackie virus A16 or enterovirus 71 [1]. We present a case series of patients with an atypical presentation of HFMD caused by Coxsackie virus A6 to demonstrate the cutaneous manifestations, age distribution, associated clinical features, and laboratory diagnosis.
Patient 1
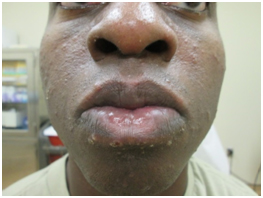
A 34-year-old African American (AA) man with known history of systemic lupus erythematosus presented with asymptomatic lesions on the face, palms, soles, and scrotum for one week. He denied fever, sick contacts, recent illnesses, or new sexual contacts.
On examination, 2-3 mm, uniform-appearing, crusted papules and erosions were present on his forehead, cheeks, ears and perioral area (Figures 1 and 2). Similar appearing lesions were present on his scrotum. His palms and soles demonstrated tender, erythematous macules (Figures 3 and 4) with mild edema. Intra-oral examination revealed 1-2 mm fine petechiae on the soft palate.

Figure 1. 2-3 mm, uniform-appearing, crusted papules and erosions were present on the forehead, cheeks, and ears
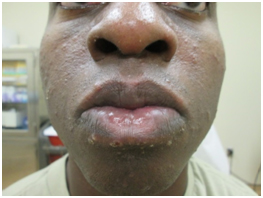
Figure 2. 2-3 mm, uniform-appearing, crusted papules and erosions were present in the perioral area

Figure 3. The soles demonstrated tender, erythematous macules with background mild edema.

Figure 4. The palms demonstrated tender, erythematous macules with background mild edema.
A Tzanck smear and varicella PCR were both negative. An initial Rapid Plasma Regain (RPR) was positive, however direct fluorescence antibody (DFA) for Treponemapallidum was negative. A rectal swab and blood sample were performed for suspected HFMD, which were sent to the Centers for Disease Control and Prevention (CDC) for reverse transcriptase polymerase chain reaction (RT-PCR) DNA sequencing. The rectal swab was positive for Coxsackie virus A6, however, serology studies were negative. The patient was treated with emollients and a low-potency topical corticosteroid and the skin lesions resolved over several days.
Patient 2
A 52-year-old AA man presented with a rapid onset of papules and vesicles on his face, upper back, soles, palms, as well as on his dorsal hands extending onto his forearms. He also noted tenderness and swelling of his left testicle. Prior to presentation he had a reported febrile illness with a temperature of 102°F with symptoms of fatigue and lethargy. The fever subsided and the skin eruption started two days later. He had noted that his daughter had a fever and sore throat one week prior, but no rash.
On examination, there were monomorphic, crusted papules on his face (Figure 5), and erythematous, ill-defined, tendermacules on his palms, soles, and the dorsal hands (Figures 6 and 7). The left testicle was warm, edematous, and tender to palpation. There were no intraoral lesions on exam.

Figure 5. Monomorphic, crusted papules on the face.

Figure 6. Erythematous, ill-defined, tender macules on patient 2’s dorsal hands.

Figure 7. Erythematous, ill-defined, tender macules on patient 2’s palms.
A rectal swab and serology were performed and both were positive for Coxsackie A6 viral infection by RT-PCR. The biopsy revealed a non-specific, spongiotic-vesicular dermatitis. Viral cytopathic effect or fungal element staining were absent, however, a viral infection was considered.
With supportive treatment, the patient’s rash and orchitis resolved over several days
Patient 3
An 18-year-old Caucasian man presented with a 12-day history of illness that began with fever and malaise, and progressed to development of painful lesions on his gluteal folds, hands, face, and feet. He subsequently developed a sore throat. Of note, the patient, who was a college student, had several similarly affected contacts, and lived in a dormitory-style living situation.
On examination, there were diffuse 1-3mm, discrete, monomorphic, erythematous papules concentrated primarily on the face in the perioral region and forehead, palms and soles, dorsal hands, fingers, and buttocks (Figures 8 and 9). Periungual hemorrhagic bullae were present on several digits of the hands and feet. A rectal swab and serology performed were both positive for Coxsackie A6 by RT-PCR. The patient’s condition resolved spontaneously over several days.

Figure 8. Diffuse 1-3mm, discrete, monomorphic, erythematous papules concentrated primarily on the face in the perioral region and forehead in patient 3.

Figure 9. Diffuse 1-3mm, discrete, monomorphic, erythematous papules on the dorsal feet of patient 3.
Patient 4
A 20-year-old Caucasian man presented with impetiginized erythematous papules and vesicles on his face, palms, soles, dorsal aspect of hands, buttocks, and medial thighs. The patient had a fever and symptoms of an upper respiratory infection that had improved several days prior to presentation. He had noted the yellow crusting of lesions a few days after the initial crop of lesions had developed on the face. The patient lived in the same dormitory as patient three, but no known contact occurred between the patients.
On examination, there were multiple erythematous, eroded macules and papules coalescing into larger plaques on the forehead, peri-nasal and peri-oral area of the face with overlying brown-yellow crust. On the dorsal hands and feet, buttocks and upper thighs were discrete, ill-defined, dusky erythematous to violaceous papules and vesicles. (Figures 10,11 and 12).

Figure 10. Multiple erythematous, eroded macules and papules coalescing into larger plaques on the forehead, peri-nasal and peri-oral area of the face with overlying brown-yellow crust.

Figure 11. On the dorsal hands were discrete, ill-defined, dusky erythematous to violaceous papules and vesicles.

Figure 12. The soles demonstrated discrete, ill-defined, dusky erythematous to violaceous papules and vesicles.
Aculture swab was obtained from one of the vesicles, and it was found to be positive for Coxsackie A6 by RT-PCR.
Hand-Foot-and-Mouth Disease (HFMD) is a common, contagious and typically, mild disease affecting children and, occasionally, exposed adults. Transmission occurs via respiratory routes or oral-oral or fecal-oral spread [2]. It is characterized by fever, painful vesicles on the oral mucosa, and papules and vesicles on the hands and feet, favoring the palms and soles. Papules and vesicles may also be present on the buttocks. Symptoms generally persist less than a week and are treated with supportive care. The most common causes are Coxsackie virus A16 and enterovirus 71 [1,3].
Cocksackie virus A6 causes a more severe form of HFMD in Europe, Asia, and the United States [1]. In children, this severe form has a spectrum of manifestations including widespread distribution, petechial eruption, and “eczema coxsackium”, which is the predilection of the HFMD vesicles for areas of eczema. This phenomenon is similar to eczema herpeticum, and among enteroviruses, only Coxsackie A16 is also known to cause it [4]. The presentation of Cocksackie A6 HFMD described in our four patients is atypical given the adult age predilection and a more generalized distribution involving the face and forehead as well as the dorsum of the hands and feet. Other unusual features that have been reported include onychomadesis, bullae formation, high fever, and increased rates of hospitalization [1]. While orchiitis has been demonstrated with other enterovirus infections (particularly coxsackie virus A9), we believe that patient two represents the first case reported of orchitis with Coxsackie virus A6 infection.
Coxsackie virus A6 should be suspected as the cause for HFMD in adults with more variable clinical manifestations [2]. To identify Coxsackie A6, we used rectal swabs, serology, and vesicular swabs. All cultures and blood serums were sent to the CDC for genetic sequencing for Coxsackie A6. Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) of vesicular fluid has been described as the most sensitive technique to identify Coxsackie A6 [3]. RT-PCR is the preferred method due to the high cross-reactivity of antibodies to other Coxsackie viruses and the virus’ poor growth in culture. Serology is often negative once the skin is involved as is evidenced by patient number one. Due to the fecal-oral spread, stool samples and rectal swabs can be used for diagnosis. In fact, even after the acute viremia, the virus can be detected in the stool for up to 4-8 weeks [2].
The unique presentations of our four adult patients with HFMD that tested positive for Coxsackie virus A6 demonstrate that this atypical form of HFMD is distinct (Tables 1 and 2). It is important for clinicians to suspect Coxsackie virus A6 in adult patients with HFMD, especially with unusual symptoms. Clinicians should also be aware of the techniques for diagnosis to ensure timely diagnosis.
Table 1. HFMD: Patient conditions descriptions
| Patient # |
Age/Gender |
Sites involved |
Fever |
Sick contacts |
Pathology results |
RT-PCR results |
| 1 |
34/M |
Face, palms, soles, ears, scrotum |
No |
No |
Not obtained |
Positive on rectal swab |
| 2 |
52/M |
Face, upper back, palms, soles, dorsal hands and forearms |
Yes |
Yes, daughter |
Spongiotic- vesicular dermatitis |
Positive on rectal swab and serology |
| 3 |
18/M |
Face, hands, feet, gluteal fold |
Yes |
Yes |
Not obtained
|
Positive on rectal swab and serology |
| 4 |
20/M |
Face, palms, soles, dorsal hands, medial thighs, buttocks |
Yes |
Yes |
Not obtained |
Positive on vesicle swab |
Table 2. Features of typical vs atypical hand-foot-and-mouth disease
| |
Typical |
Atypical |
| Etiology |
Coxsackie virus A16 or enterovirus 71 |
Coxsackie virus A6 |
| Age distribution |
Predominantly children |
Children and adults |
| Intraoral lesions |
Nearly universal |
Less common |
2021 Copyright OAT. All rights reserv
| Facial rash |
Uncommon |
Common |
| Involvement of areas of atopic dermatitis |
Rare |
Common |
| Onychomadesis |
Uncommon |
Common |
| Vesicles/bullae |
Rare |
Very common |
- 1) Feder HM Jr, Bennett N, Modlin JF (2014) Atypical hand, foot, and mouth disease: a vesiculobullous eruption caused by Coxsackie virus A6. Lancet Infect Dis 14: 83-86. [Crossref]
- 2) Downing C, Ramirez-Fort MK, Doan HQ, Benoist F, Oberste MS, et al. (2014) Coxsackievirus A6 associated hand, foot and mouth disease in adults: clinical presentation and review of the literature. J Clin Virol 60: 381-386.[Crossref]
- 3) Lott JP, Liu K, Landry ML, Nix WA, Oberste MS, et al. (2013) Atypical hand-foot-and-mouth disease associated with coxsackievirus A6 infection. J Am Acad Dermatology 69: 736-741. [Crossref]
- 4) Mathes EF, Oza V, Frieden IJ, Cordoro KM, Yagi S, et al. (2013) “Eczema coxsackium” and unusual cutaneous findings in an enterovirus outbreak. Pediatrics 132: e149-155. [Crossref]
Editorial Information
Editor-in-Chief
Torello Lotti
University of Rome "G.Marconi" Rome
Article Type
Review Article
Publication history
Received: October 14, 2014
Accepted: October 22, 2014
Published: October 24, 2014
Copyright
©2014 Harris M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Harris M, Kimes K, Chern C, Cunningham R, Handfield K, et al. (2014) Coxsackie A6 infection-atypical hand-foot-mouth disease in the US military: A case series. Glob Dermatol, 1: DOI: 10.15761/GOD.1000106
Table 1. HFMD: Patient conditions descriptions
| Patient # |
Age/Gender |
Sites involved |
Fever |
Sick contacts |
Pathology results |
RT-PCR results |
| 1 |
34/M |
Face, palms, soles, ears, scrotum |
No |
No |
Not obtained |
Positive on rectal swab |
| 2 |
52/M |
Face, upper back, palms, soles, dorsal hands and forearms |
Yes |
Yes, daughter |
Spongiotic- vesicular dermatitis |
Positive on rectal swab and serology |
| 3 |
18/M |
Face, hands, feet, gluteal fold |
Yes |
Yes |
Not obtained
|
Positive on rectal swab and serology |
| 4 |
20/M |
Face, palms, soles, dorsal hands, medial thighs, buttocks |
Yes |
Yes |
Not obtained |
Positive on vesicle swab |
Table 2. Features of typical vs atypical hand-foot-and-mouth disease
| |
Typical |
Atypical |
| Etiology |
Coxsackie virus A16 or enterovirus 71 |
Coxsackie virus A6 |
| Age distribution |
Predominantly children |
Children and adults |
| Intraoral lesions |
Nearly universal |
Less common |
| Facial rash |
Uncommon |
Common |
| Involvement of areas of atopic dermatitis |
Rare |
Common |
| Onychomadesis |
Uncommon |
Common |
| Vesicles/bullae |
Rare |
Very common |

Figure 1. 2-3 mm, uniform-appearing, crusted papules and erosions were present on the forehead, cheeks, and ears
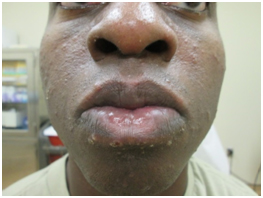
Figure 2. 2-3 mm, uniform-appearing, crusted papules and erosions were present in the perioral area

Figure 3. The soles demonstrated tender, erythematous macules with background mild edema.

Figure 4. The palms demonstrated tender, erythematous macules with background mild edema.

Figure 5. Monomorphic, crusted papules on the face.

Figure 6. Erythematous, ill-defined, tender macules on patient 2’s dorsal hands.

Figure 7. Erythematous, ill-defined, tender macules on patient 2’s palms.

Figure 8. Diffuse 1-3mm, discrete, monomorphic, erythematous papules concentrated primarily on the face in the perioral region and forehead in patient 3.

Figure 9. Diffuse 1-3mm, discrete, monomorphic, erythematous papules on the dorsal feet of patient 3.

Figure 10. Multiple erythematous, eroded macules and papules coalescing into larger plaques on the forehead, peri-nasal and peri-oral area of the face with overlying brown-yellow crust.

Figure 11. On the dorsal hands were discrete, ill-defined, dusky erythematous to violaceous papules and vesicles.

Figure 12. The soles demonstrated discrete, ill-defined, dusky erythematous to violaceous papules and vesicles.