Abstract
Tibiotalocalcaneal arthrodesis is a technically difficult reconstructive procedure. The customary surgical approach is usually performed through an anterior, medial, or lateral incision. These incisional approaches, although most popular amongst foot and ankle surgeons, are associated with numerous complications, both intra-operatively and post-operatively. The posterior approach provides the surgeon with an unmatched visualization of the subtalar and ankle joints. We report a case in which a midline posterior incision was used for a patient who required tibiotalocalcaneal arthrodesis with intramedullary nailing and who concurrently required excision of a painful posterosuperior calcaneal enthesiopathy.
Key words
tibiotalocalcaneal arthrodesis, posterior approach, intramedullary nail
Introduction
Tibiotalocalcaneal (TTC) arthrodesis is a staple amongst foot and ankle surgeons. It is performed as a salvage procedure for a myriad of pathology, including post-traumatic arthritis, severe osteoarthritis, Rheumatoid arthritis, posterior tibial tendon dysfunction, Charcot neuroarthropathy, avascular necrosis, and other neuromuscular disorders to name a few [1,2]. Various methods of fixation have been described throughout the literature including external fixation, plates, screws, intramedullary nails, steinmann pins, or a combination of the above. There is still debate on the appropriate manner in which the procedure is performed and the form of fixation is usually surgeon dependent [1-9]. Many surgical approaches have been described for TTC arthrodesis, including anterior, medial, and lateral. The approach chosen depends on multiple factors including fixation type, surgeon preference, previous trauma, and the soft tissue envelope [2,4,10-14]. There is little literature describing the posterior approach to the TTC arthrodesis. In 2006, Hammit et al. described the midline posterior approach to access the ankle and subtalar joints [11]. A thorough literature review revealed only one depiction of the TTC arthrodesis with intramedullary nailing [15]. The purpose of this paper is to present our method of TTC arthrodesis utilizing the posterior approach in a patient who concomittantly had severe insertional tendo achilles pain with a visible enthesopathy on radiograph.
Case report
A 53 year old female with prior cerebrovascular accidents, type 2 diabetes mellitus, vitamin D deficiency, rheumatoid arthritis, and left drop foot was referred to our office with chief complaint of left heel pain that had progressively worsened. Approximately six months prior to her referral, she had undergone a left achilles tendon debridement with retrocalcaneal resection by another surgeon. The patient complained of pain and edema to the surgical site, specifically the ankle and posterior heel. This was aggravated by ambulation and gradually became more painful over the course of the day. She had previously been custom fitted and wore comfortably, a hinged Modfied Ankle Foot Orthosis (MAFO) for her foot drop, however on initial presentation was unable to use this device due to the edema of her previous surgical procedure.
Upon clinical exam, the patient was vascularly intact with well-healed previous surgical scars. The patient had diminished epicritic sensation to the left lower extremity. There was pain on palpation along the distal course of the left achilles tendon as well as with passive and active ankle and subtalar joint ranges of motion. An equinus contracture was present and only trace muscle contractions were noted during the dorsiflexory range of motion of the foot on the ankle.
Pre-operative radiographic exam revealed 15 degrees of tibiocalcaneal varus with an 84 degree anterior distal tibial angle. The lateral distal tibial angle measured 94 degrees (Figure 1).

Figure 1. Preoperative radiographs showing 15 degrees of heel varus, 84 degree anterior distal tibial angle, and 94 degree lateral distal tibial angle.
The ankle joint appeared incongruous with a small anterior joint impingement. The posterior aspect of the posterior subtalar joint facet was noted seen to have osteoarthritic changes. There was also a significant posterosuperior calcaneal enthesiopathy.
Post-operatively, the patient was non-weight bearing to the left lower extremity in a splint compression dressing. At the patient’s first post-op visit, one week following surgery, there was moderate erythema to the peri-incisional area consistent with a superficial cellulitis. The patient was placed on oral antibiotics for this for ten days. The cellulitis resolved with completion of the antibiotics. At post op week seven the patient was transitioned into a controlled ankle motion (CAM) walker, however non weight bearing status was maintained for the initial ten weeks post opertive. Over the next four weeks the patient was transitioned from partial weight bearing in the CAM walker to weight bearing as tolerated in a flat surgical shoe. Soon thereafter and currently, the patient is ambulating without complaint in a sneaker. Follow-up radiographs throughout this time showed evidence of delayed union along the posterior aspect of the subtalar joint, however at 11 months post-operatively, radiographs showed full consolidation across the fusion sites without progression of the deformity. Alignment was well maintained and all hardware was intact (Figure 2).

Figure 2. Radiographs 11 months post-operative. Full consolidation across the ankle and subtalar joints with hardware intact and alignment maintained.
Surgical technique
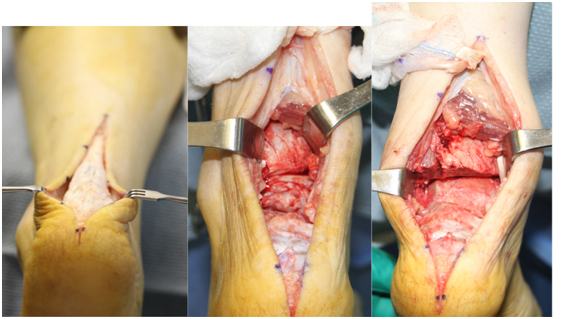
The patient was placed in the prone position and a pneumatic thigh tourniquet was applied. A linear incision was made, approximately 8 cm in length, spanning from the most distal and posterior aspects of the patients heel to 5 cm proximal to the ankle joint. After the skin was incised, dissection was carried down to the Achilles tendon. Intra-operatively, there were two slits of tendon with signs of non-viable portions of the tendon as well retained sutures from the previous procedure. A linear mid-substance incision was made through the Achilles tendon. The Achilles tendon was then freed from its distal calcaneal insertion and retracted out of the surgical field with a moist sponge. This provided great visualization of the posterior ankle capsule, ankle joint, subtalar joint, and irregularities at the posterosuperior aspect of the calcaneus (Figure 3).
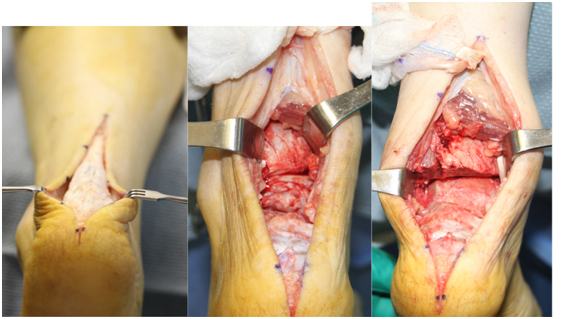
Figure 3. Intra-operative photos showing posterior midline incision. Once the Achilles tendon is detached, the subtalar and ankle joints are exposed, allowing for unparalleled visualization and the ability to better align the joint surfaces.
The ankle joint was placed through range of motion and the posterior capsule was released. Osteotome and mallet were used to perform wedge resection of the articular cartilage of the talar dome as well as the tibial plafond, allowing for minor correction of the calcaneal deformity. Care was also taken to resect the cartilaginous surfaces of the medial malleolus and medial aspect of the talar dome and body. Attention was then drawn to the subtalar joint where additional cartilaginous wedge resection of the posterior and middle facets was performed utilizing an oscillating sagittal saw as well as osteotome and mallet. Bony apposition and alignment of both the ankle and subtalar joints was confirmed with intraoperative fluoroscopy. The guide wire system including the targeting device was then applied to the lower extremity. A 3.2 mm guide wire was driven proximally from the plantar heel to the level of the talar dome. At this time, an additional aiming arm was applied to the guide wire system. A second 3.2 mm guide wire was then inserted through this aiming arm and driven until it met the first guidewire. At this point, the targeting device and first guide wire were removed leaving the guide wire system and additional aiming arm in place. A 13 mm cannulated drill was then used to drill through the calcaneus and talus. Once the drill was at the level just distal to the ankle joint the foot was appropriately positioned and the drill was carried approximately 1 cm into the distal tibia. The drill and second guidewire were removed and a ball-tipped guidewire was inserted into this respective drill hole. The guidewire was carefully advanced proximally up the tibia under fluoroscopic guidance. A 300 mm interlocking nail was determined to best suit the patient at this time. Leaving the guidewire in place, the lower extremity was reamed sequentially from 8 mm to 11 mm. The tibial canale was reamed 1 cm greater than the planned 10 mm diameter nail. Reaming was carried to the level of the ball-tip on the guidewire. The nail was then preassembled with the compression screw intact and placed on the insertion handle. An aiming nail alignment rod was used to ensure the nail was aligned correctly. The aiming arm was then removed and nail was inserted utilizing a mallet under fluoroscopic guidance until the most distal end was flush with the plantar cortex of the calcaneus. Following this, the locking screw targeting guide was applied to the apparatus. Attention was directed towards the calcaneus first, where a 5mm drill was inserted through the dynamic drill hole and forwarded to a level just proximal to the calcaneal-cuboid joint. The drill was removed and a 6 mm by 70 mm screw with a threaded head was then inserted into this position. A 4.2 mm drill was then inserted through the dynamic hole on the aiming apparatus for talar fixation. The drill was advanced to a level just proximal to the talonavicular joint. The drill was removed and a 5.0 mm by 48 mm screw was placed. The aiming arm was then adjusted to apply fixation proximally. Again, the dynamic slot was used and a 4.2 mm drill was used to create two tibial holes for screw insertion. These were performed in a medial to lateral fashion, ensuring that both cortices were penetrated. Two 5.0 mm by 26 mm screws were inserted into their respective drill holes. Once the tibial screws had been placed, the nail guide apparatus was removed and the compression bolt, which was placed in the nail prior to insertion, was tightened utilizing a hexagonal driver. Tightening was performed under fluoroscopy and compression was visualized across both the subtalar and ankle joints. Attention was re-directed back to the Achilles tendon where the nonviable portion of the tendon and previous sutures were debrided and excised. The two slits of the tendon were repaired with two Ethibond sutures in a whipstitch locked fashion. An osteotome and mallet were used to resect the prominent, painful posterosuperior aspect of the calcaneal deformity. Following resection, a rasp was then used to smooth any sharp prominences. Two suture loop guide wires were placed in a converging direction in the posterosuperior aspect of calcaneus, one entering slightly medial and one more lateral. A drill was used to create pilot holes over these guide wires. The ends of the suture from the whipstitch were then passed through the suture loop and pulled through the plantar calcaneus and out through the heel. While manual tension was applied to both suture strands, two 8 mm by 25 mm tenodesis screws were implanted in the posterosuperior aspect of the calcaneus. The incision was then closed in a layer fashion and a splint was applied.
Discussion
Numerous techniques have been described addressing the TTC arthrodesis, validating the complexity and difficulty of the procedure. The surgical approach should allow for optimal visualization of the joint surfaces. Although anterior, medial, and lateral approaches have been well documented, the authors believe the posterior approach affords the surgeon greater visualization and provides greater exposure for frontal plane correction. If performing the resection through medial or lateral incisions, it can be difficult to intra-operatively determine the amount of correction due to the narrow field of view. No matter what type of resection the surgeon prefers, we hypothesize that in patients with severe frontal plane malalignment, as was the case with our patient, the direct coronal view grants us the maximum potential for re-alignment.
The posterior approach allows for the preservation of the fibula, which provides additional support across the subtalar and ankle joints. The lateral approach can often find the fibula problematic while performing joint resection. Preserving the fibula not only deepens the structural support but can act as a stabilizing factor if future total ankle replacement is decided upon [15].
Wound complications associated with a tendo-achilles incision are described throughout the literature. Angiosomes are three dimensional vascular areas of skin, subcutaneous tissue, muscle, tendon and bone [16,17]. We performed a midline posterior incision to lower the risk of vascular compromise to the area, considering this area lies between the posterior tibial and peroneal angiosomes [17]. Kile and Johnson and Hammitt et al. agreed with our incision placement and felt wound healing became problematic when the incision swayed to the medial or lateral aspects of the Achilles [11,18]. On the contrary, Yepes et al. found that skin overlying the posterior midline was of the poorest vascularity when compared to the medial or lateral surrounding integument. They recommended that surgeons who prefer a medial incision, keep the skin incision at least 1 cm medial to the Achilles tendon. They also recommended that the surgeon incise the paratenon without dissecting it from the fat and skin overlying the tendon [19]. Hirsch and Fleming understood the concept of preserving the paratenon during this dissection, however they argue that this jeopardizes the ability to acquire hemostasis during the procedure [15].
Our case was not only unique in that we chose to use a posterior approach to gain access to the subtalar and ankle joints but also because we opted to utilize the SBI A3 nail. The A3 is distinct by reason of its 15 degree posterior and 10 degree valgus bend. The posterior bend allows for increase purchase into the calcaneus while your typical valgus nail may only afford limited contact. In comparison, we prefer straight nails when performing tibiocalcaneal fusions, for example in Charcot reconstructions where talectomy is required. We feel other pearls of inserting intramedullary nails for TTC arthrodesis are choosing a longer rather than shorter nail for increased stability and torsional strength. The end cap should also be applied to obtain purchase of the plantar cortex of the calcaneus. We opted not to do this in the current case because we felt the position of the distal nail was flush with the plantar cortex, thus application of the end cap would create a plantar prominence.
As with any surgery there are disadvantages to our proposed approach. The patient can develop a painful scar to the posterior Achilles and/or at the posterosuperior aspect of the calcaneus, which can be significant in shoe gear. Obviously, there can be associated post-surgical pain and pathology to the Achilles tendon. Our case describes detachment and reattachment of the Achilles at its insertion. Although the function of the achilles tendon is extremely hindered upon fusion of the subtalar and ankle joints, it can still provide structural support across the posterior aspect of the knee joint.
In our experience, accessing the subtalar and ankle joint simultaneously can be effectively accomplished through a posterior midline incision. We feel that in patients with severe frontal plane deformity, this approach should be more greatly considered. Future studies will need to be performed to more adequately determine the success of this incision.
References
- Burks JB (2012) Tibiotalocalcaneal arthrodesis. Clin Podiatr Med Surg 29: 529-545. [Crossref]
- Hyer CF, Cheney N (2013) Anatomic aspects of tibiotalocalcaneal nail arthrodesis. J Foot Ankle Surg 52: 724-727. [Crossref]
2021 Copyright OAT. All rights reserv
- Thomas RL, Sathe V, Habib SI (2012) The use of intramedullary nails in tibiotalocalcaneal arthrodesis. J Am Acad Orthop Surg 20: 1-7. [Crossref]
- Niinimäki TT, Klemola TM, Leppilahti JI (2007) Tibiotalocalcaneal arthrodesis with a compressive retrograde intramedullary nail: a report of 34 consecutive patients. Foot Ankle Int 28: 431-434. [Crossref]
- Jeng CL, Campbell JT, Tang EY, Cerrato RA, Myerson MS (2013) Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int 34: 1256-1266. [Crossref]
- O'Neill PJ, Logel KJ, Parks BG, Schon LC (2008) Rigidity comparison of locking plate and intramedullary fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int 29: 581-586. [Crossref]
- Jeong ST, Park HB, Hwang SC, Kim DH, Nam DC (2012) Use of intramedullary nonvascularized fibular graft with external fixation for revisional Charcot ankle fusion: a case report. J Foot Ankle Surg 51: 249-253. [Crossref]
- Yakacki CM, Khalil HF, Dixon SA, Gall K, Pacaccio DJ (2010) Compression forces of internal and external ankle fixation devices with simulated bone resorption. Foot Ankle Int 31: 76-85. [Crossref]
- DiDomenico LA, Wargo-Dorsey M (2012) Tibiotalocalcaneal arthrodesis using a femoral locking plate. J Foot Ankle Surg 51: 128-132. [Crossref]
- Hayes AG, Nadkarni JB (1996) Extensile posterior approach to the ankle. J Bone Joint Surg Br 78: 468-470. [Crossref]
- Hammit MD, Hobgood ER, Tarquinio TA (2006) Midline posterior approach to the ankle and hindfoot. Foot Ankle Int 27: 711-715. [Crossref]
- Boer R, Mader K, Pennig D, Verheyen CC (2007) Tibiotalocalcaneal arthrodesis using a reamed retrograde locking nail. Clin Orthop Relat Res 463: 151-156. [Crossref]
- Hammett R, Hepple S, Forster B, Winson I (2005) Tibiotalocalcaneal (hindfoot) arthrodesis by retrograde intramedullary nailing using a curved locking nail. The results of 52 procedures. Foot Ankle Int 26: 810-815. [Crossref]
- Millett PJ, O'Malley MJ, Tolo ET, Gallina J, Fealy S, et al. (2002) Tibiotalocalcaneal fusion with a retrograde intramedullary nail: clinical and functional outcomes. Am J Orthop (Belle Mead NJ) 31: 531-536. [Crossref]
- Fetter NL, DeOrio JK (2012) Posterior approach with fibular preservation for tibiotalocalcaneal arthrodesis with an intramedullary nail. Foot Ankle Int 33: 746-749. [Crossref]
- Hersh IR, Fleming JJ (2012) Considerations of a midline posterior approach to the ankle and subtalar joints. J Foot Ankle Surg 51: 482-486. [Crossref]
- Attinger CE, Cooper P, Blume P (1997) Vascular anatomy of the foot and ankle. Oper Techniq Plast Reconstr Surg 4:183–198. \
- Kile TA, Donnelly RE, Gehrke JC, Werner ME, Johnson KA (1994) Tibiotalocalcaneal arthrodesis with an intramedullary device. Foot Ankle Int 15: 669-673. [Crossref]
- Yepes H, Tang M, Geddes C, Glazebrook M, Morris SF, et al. (2010) Digital vascular mapping of the integument about the Achilles tendon. J Bone Joint Surg Am 92: 1215-1220. [Crossref]