We investigated whether calcitonin gene-related peptide (CGRP)-related gene polymorphisms are involved in the aggravation of migraines due to medication overuse. In total, 47 migraine patients (6 males and 41 females; 36.4 10.3 years) and 22 medication overuse headache (MOH) patients (1 male and 21 females; 39.6 9.9 years) who had migraine participated in this study. Calcitonin gene-related polypeptide-alpha (CALCA, α-CGRP, Insertion/Deletion rs1553005, rs145837941) and CGRP receptor (receptor activity-modifying protein 1: RAMP1, rs3754701, rs7590387) were analyzed by polymerase chain reaction (PCR) and PCR-restriction fragment length polymorphism (PCR-RFLP) methods. No significant differences were observed in the genotype distributions of CALCA and RAMP1 between migraine patients and MOH patients. The results of this study showed no association between CGRP-related gene polymorphisms and the complication of MOH in migraine patients.
medication overuse headache, migraine, polymorphism, calcitonin gene-related peptide
Migraine patients are particularly prone to developing medication overuse headache (MOH) [1-3]. Moreover, it has been shown that 56.8% of migraine sufferers use over-the-counter medicine alone [4]. Although MOH is known to be caused by triptan, ergotamine, opioid, and/or analgesic overuse in patients with headache [1], 85.1% of MOH patients overuse combination analgesics according to research by Imai et al. [2]. Most patients return to an episodic migraine pattern following drug withdrawal. However, the complication of MOH markedly decreases the quality of life of these patients [1]. In addition, the incidence of comorbidity with depression is higher in MOH patients than in migraine patients [3,5]. Therefore, the aggravation of migraines due to medication overuse needs to be prevented.
Calcitonin gene-related polypeptide-alpha (CALCA, α-CGRP) is a potent vasodilator and one of the mediators of neurogenic inflammation. Plasma levels of calcitonin gene-related peptide (CGRP), later called α-CGRP, are elevated in migraine patients [6,7], and an infusion of CGRP can trigger a migraine attack [8]. In addition, CGRP antagonists have good efficacy in the treatment of acute migraine attacks [9, 10]. Thus, CGRP is a key molecule in migraine pathogenesis. Interestingly, in MOH model animals, triptan increased CGRP levels [11]. In addition, exposure to μ opioids such as morphine also increased CGRP in cultured dorsal root ganglion cells [12,13]. Therefore, increasing CGRP through medication overuse seems to aggravate migraines.. On the other hand, Menson et al. [14] showed no significant association between the intronic 16 bp deletion in the CALCA gene and migraine. Sutherland et al. [15] also reported that CALCA polymorphisms (rs3781719, rs145837941) and CGRP receptor (receptor activity-modifying protein 1: RAMP1, rs3754701, rs7590387) are not involved in the pathogenesis of migraine. However, to the best of our knowledge, there have been no studies on the relationship between CGRP-related gene polymorphisms and MOH.
In present study, we focused on CGRP-related gene polymorphisms such as CALCA and RAMP1 and investigated the relationship between CGRP-related gene polymorphisms and the complication of MOH in migraine patients.
Subjects
We enrolled 47 migraine patients [6 males and 41 females: 5 with migraines with aura (MA), 36 with migraines without aura (MO), 6 with both MA and MO at different times; 36.4 10.3 years of age] and 22 MOH patients who had migraine (1 male and 21 females: 1 with MA and 21 with MO; 39.6 9.9 years of age) who were seen in an outpatient clinic of the Department of Neurology, Showa University East Hospital, Tokyo, Japan, between May 2010 and January 2011. These subjects were the same as those included in a previous study [16]. The incidence of depression was significantly higher in MOH patients than in migraine patients (p < 0.001) [16]. The medications that were overused were combination analgesics in 14 patients (64%), analgesics in 9 patients (41%), and triptans in 2 patients (9%) [16].
Migraines were diagnosed according to the International Classification of Headache Disorders, 2nd Edition (ICHD-II), 2004 [17]. We also confirmed by interview that migraine patients did not overuse headache medications. The revised ICHD-II criteria were used to diagnose MOH [1]. MOH patients were questioned about their primary headaches by headache specialists. In addition, these headache specialists confirmed the primary headache according to the ICHD-II criteria after treating MOH. Although the subjects of the present study included not only patients with migraines but also patients with migraines and tension-type headaches, patients with tension-type headaches were excluded. We used the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [18] to diagnose major depressive disorder.
All patients were Japanese. All patients who provided informed consent, including those with migraines and the subset with MOH, were enrolled in the study. This clinical study was approved by the Ethics Committee for Genome Research of Showa University.
Genotyping
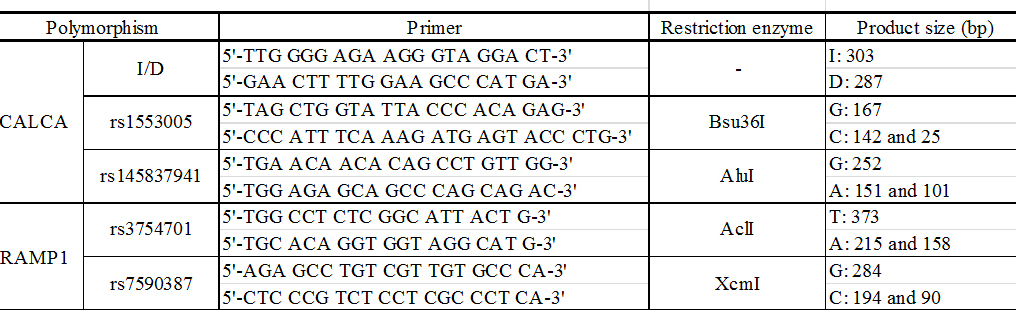
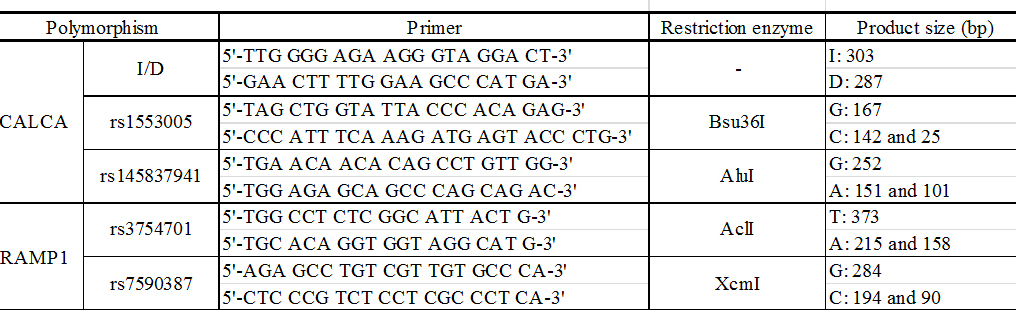
Genomic DNA was extracted from whole blood using NucleoSpin Blood QuickPure (NIPPON Genetics Co., Ltd., Tokyo, Japan). The gene polymorphisms of CGRP (Insertion/Deletion (I/D) [14], rs1553005, rs145837941) and RAMP1 (rs3754701, rs7590387) [15] were studied. The polymorphism of each gene was determined by polymerase chain reaction (PCR) and PCR-restriction fragment length polymorphism (PCR-RFLP) methods. Primer sequences, restriction enzymes, and expected fragment sizes of the gene polymorphisms are shown in Table 1. The PCR products or restriction enzyme-treated PCR fragments were run on 3% agarose gels and stained with ethidium bromide.
Table1. Primers and restriction enzymes used for genotyping.
Statistical analysis
Categorical variables were analyzed by 2 test or Fisher’s exact test using Excel Statistics 2008 for Windows (Excel Toukei, Social Survey Research Information Co., Tokyo, Japan). p values ≤ 0.05 were considered significant.
The genotype distributions of polymorphisms of the CALCA (Insertion/Deletion, I/I vs. I/D plus D/D, p=1.000; rs1553005, G/G vs. G/C plus C/C, p=0.646; rs145837941, A/A vs. A/G plus G/G, p=1.000) .and RAMP1 (rs3754701, A/A vs. A/T plus T/T, p=0.573; rs7590387; G/G vs. G/C plus C/C, p=0.342) genes were not significantly different between migraine patients and MOH patients (Table 2).
Table 2. Genotype distribution of gene polymorphisms
|
|
|
Migraine |
MOH |
|
|
|
n=47 |
(%) |
n=22 |
(%) |
P value |
CALCA |
I/D |
I/I |
47 |
100.0 |
22 |
100.0 |
|
|
|
I/D |
0 |
0.0 |
0 |
0.0 |
|
|
|
D/D |
0 |
0.0 |
0 |
0.0 |
|
|
|
I/I |
47 |
100.0 |
22 |
100.0 |
1.000 |
|
|
I/D,D/D |
0 |
0.0 |
0 |
0.0 |
|
|
rs1553005 |
G/G |
22 |
46.8 |
9 |
40.9 |
|
|
|
G/C |
18 |
38.3 |
10 |
45.5 |
|
|
|
C/C |
7 |
14.9 |
3 |
13.6 |
|
|
|
G/G |
22 |
46.8 |
9 |
40.9 |
0.646 |
|
|
G/C,C/C |
25 |
53.2 |
13 |
59.1 |
|
|
rs145837941 |
A/A |
47 |
100.0 |
22 |
100.0 |
|
|
|
A/G |
0 |
0.0 |
0 |
0.0 |
|
|
|
G/G |
0 |
0.0 |
0 |
0.0 |
|
|
|
A/A |
47 |
100.0 |
22 |
100.0 |
1.000 |
|
|
A/G,G/G |
0 |
0.0 |
0 |
0.0 |
|
RAMP1 |
rs3754701 |
A/A |
18 |
38.3 |
10 |
45.5 |
|
|
|
A/T |
20 |
42.6 |
8 |
36.4 |
|
|
|
T/T |
9 |
19.1 |
4 |
18.2 |
|
|
|
A/A |
18 |
38.3 |
10 |
45.5 |
0.573 |
|
|
A/T,T/T |
29 |
61.7 |
12 |
54.5 |
|
|
rs7590387 |
G/G |
22 |
46.8 |
13 |
59.1 |
|
|
|
G/C |
23 |
48.9 |
8 |
36.4 |
|
|
|
C/C |
2 |
4.3 |
1 |
4.5 |
|
|
|
G/G |
22 |
46.8 |
13 |
59.1 |
0.342 |
|
G/C,C/C |
25 |
53.2 |
9 |
40.9 |
|
We previously reported that gene polymorphisms such as methylenetetrahydrofolate reductase (rs1801133) and dopamine D2 receptor (rs6275) were associated with the complication of MOH in migraine patients [16], in addition to the tumor necrosis factor (TNF)- β gene polymorphism [20]. Thus, gene polymorphisms that are unrelated to 5-hydroxytryptamine seem to be associated with the aggravation of migraines by medication overuse.
In the present study, we focused on the relationship between CGRP-related gene polymorphisms and the complication of MOH in migraine patients. However, no association was observed between CGRP (I/D, rs1553005, rs145837941) and RAMP1 (rs3754701, rs7590387) gene polymorphisms and the aggravation of migraines by medication overuse. Recently, Munksgaard et al. [21] reported that no change in CGRP was detected despite dramatic reduction in headache frequency after the detoxification of MOH patients, suggesting that CGRP is not involved in MOH. Although Cernuda-Morollon et al. [22] reported that CGRP levels in peripheral blood were a biomarker for chronic migraine outside migraine attack times, analgesic overuse did not significantly influence CGRP levels. Therefore, CGRP may be unrelated to MOH in migraine patients. However, because the small sample size was a limiting factor in the present study, larger genetic studies are required to identify CGRP-related gene fragments that may be associated with MOH in migraine patients.
- Headache Classification Committee, Olesen J, Bousser MG, Diener HC, Dodick D, et al. (2006) New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 26: 742-746. [Crossref]
- Imai N, Kitamura E, Konishi T, Suzuki Y, Serizawa M, et al. (2007) Clinical features of probable medication-overuse headache: a retrospective study in Japan. Cephalalgia 27: 1020-1023. [Crossref]
- Kanki R, Nagaseki Y, Sakai F (2008) Medication-overuse headache in Japan. Cephalalgia 28: 1227-1228. [Crossref]
- Sakai F, Igarashi H (1997) Prevalence of migraine in Japan: a nationwide survey. Cephalalgia 17: 15-22. [Crossref]
- Kaji Y, Hirata K (2009) Cha2021 Copyright OAT. All rights reservanese patients with medication-overuse headache. Intern Med 48: 981-986. [Crossref]
- Goadsby PJ, Edvinsson L, Ekman R (1990) Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol 28: 183-187. [Crossref]
- Juhasz G, Zsombok T, Modos EA, Olajos S, Jakab B, et al. (2003) NO-induced migraine attack: strong increase in plasma calcitonin gene-related peptide (CGRP) concentration and negative correlation with platelet serotonin release. Pain 106: 461-470.
- Lassen LH, Haderslev PA, Jacobsen VB, Iversen HK, Sperling B, et al. (2002) CGRP may play a causative role in migraine. Cephalalgia 22: 54-61. [Crossref]
- Olesen J, Diener HC, Husstedt IW, Goadsby PJ, Hall D, et al. (2004) Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N Engl J Med 350: 1104-1110. [Crossref]
- Petersen KA, Birk S, Lassen LH, Kruuse C, Jonassen O, et al. (2005) The CGRP-antagonist, BIBN4096BS does not affect cerebral or systemic haemodynamics in healthy volunteers. Cephalalgia 25: 139-147. [Crossref]
- De Felice M, Ossipov MH, Wang R, Lai J, Chichorro J, et al. (2010) Triptan-induced latent sensitization: a possible basis for medication overuse headache. Ann Neurol 67: 325-337. [Crossref]
- Ma W, Zheng WH, Kar S, Quirion R (2000) Morphine treatment induced calcitonin gene-related peptide and substance P increases in cultured dorsal root ganglion neurons. Neuroscience 99: 529-539.
- Belanger S, Ma W, Chabot JG, Quirion R (2002) Expression of calcitonin gene-related peptide, substance P and protein kinase C in cultured dorsal root ganglion neurons following chronic exposure to mu, delta and kappa opiates. Neuroscience 115: 441-453.
- Menon S, Buteri J, Roy B, Murrell M, Quinlan S, et al. (2011) Association study of calcitonin gene-related polypeptide-alpha (CALCA) gene polymorphism with migraine. Brain Res 1378: 119-124. [Crossref]
- Sutherland HG, Buteri J, Menon S, Haupt LM, Macgregor EA, et al. (2013) Association study of the calcitonin gene-related polypeptide-alpha (CALCA) and the receptor activity modifying 1 (RAMP1) genes with migraine. Gene 515: 187-192. [Crossref]
- Onaya T, Ishii M, Katoh H, Shimizu S, Kasai H, et al. (2013) Predictive index for the onset of medication overuse headache in migraine patients. Neurol Sci 34: 85-92. [Crossref]
- Katsarava Z, Dzagnidze A, Kukava M, Mirvelashvili E, Djibuti M, et al. (2009) Primary headache disorders in the Republic of Georgia: prevalence and risk factors. Neurology 73: 1796-1803. [Crossref]
- Headache Classification Subcommittee of the International Headache Society (2004) The International Classification of Headache Disorders: 2nd edition. Cephalalgia 24 Suppl 1: 9-160. [Crossref]
- Diagnostic and Statistical Manual of Mental Disorders. IVth Edition. Washington. American Psychiatric Association Press.
- Morita A, Nakayama T, Soma M, Mizutani T (2007) Association between the calcitonin-related peptide alpha (CALCA) gene and essential hypertension in Japanese subjects. Am J Hypertens 20: 527-532.
- Ishii M, Onaya T, Katoh H, Kiuchi Y, Kasai H, et al. (2012) Association between the G252A Tumor Necrosis Factor-β Gene Polymorphism and Medication-Overuse Headache. J Clin Neurol 8: 301-304. [Crossref]
- Munksgaard SB, Frandsen E, Bendtsen L, Jensen RH (2014) EHMTI-0388. Levels of calcitonin-gene related peptide in medication overuse headache – a pilot study. Journal of Headache Pain 15 (Suppl 1): I9.
- Cernuda-Morollón E, Larrosa D, Ramón C, Vega J, Martínez-Camblor P, et al. (2013) Interictal increase of CGRP levels in peripheral blood as a biomarker for chronic migraine. Neurology 81: 1191-1196. [Crossref]