Abstract
Ilioinguinal nerve block has shown great utility as a diagnostic, prognostic, and therapeutic maneuver in the evaluation and treatment of groin and genital pain that is thought to be mediated via the ilioinguinal nerve. When combined with iliohypogastric and genitofemoral nerve block, ilioinguinal nerve block can also be utilized to provide surgical anesthesia for groin and genital surgery. While ilioinguinal nerve block can be performed utilizing a anatomic landmark guided technique, the addition of ultrasound guidance will improve the accuracy of needle placement and decrease complications. This article describes a simplified technique for performing ultrasound guided ilioinguinal nerve block.
Key words
ilioinguinal nerve block, ultrasound guided nerve block, ilioinguinal nerve, iliohypogastric nerve, groin pain, genital pain, regional anesthesia
Introduction
Ilioinguinal nerve block has shown great utility as a diagnostic, prognostic, and therapeutic maneuver in the evaluation and treatment of groin and genital pain thought to be mediated via the ilioinguinal nerve [1]. This nerve block is used most commonly to diagnose and treat the common entrapment neuropathy, ilioinguinal neuralgia [2]. Ilioinguinal neuralgia presents clinically as burning pain, paresthesias, and numbness over the lower abdomen that radiates into the scrotum or labia and occasionally into the upper inner thigh, but never below the knee. Ilioinguinal nerve block can also be utilized to provide surgical anesthesia for groin and genital surgery, when combined with iliohypogastric and genitofemoral nerve block. While ilioinguinal nerve block has traditionally been performed using an anatomic landmark guided technique, the addition of ultrasound guidance for needle placement will improve the accuracy of needle placement and decrease complications [3]. This article describes a simplified technique for performing ultrasound guided ilioinguinal nerve block that combines the use of the anatomic landmarks traditionally used when performing the anatomic landmark guided technique with ultrasound localization of the actual ilioinguinal nerve as it lies in the facial plane between the internal oblique and transversus abdominis muscles.
Clinically relevant anatomic considerations
The ilioinguinal nerve is comprised of fibers from the L1 nerve root with a contribution of fibers from the T12 nerve root in approximately 25% of patients [4]. Exiting from the lateral border of the psoas muscle, the ilioinguinal nerve follows a curvilinear course that takes it from the L1 and occasionally T12 somatic nerves to pass along the inside of the concavity of the ilium. The ilioinguinal nerve continues to pass anteriorly as it runs within a fascial plane between the internal oblique and transverse abdominius muscles. It is within this fascial cleft that the ilioinguinal nerve is identified with ultrasound scanning and it is at this point that the nerve is easily blocked using ultrasound guided needle placement.
At the level of the anterior superior iliac spine, the ilioinguinal nerve perforates anteriorly through the transverse abdominis muscle with the nerve’s terminal branches providing sensory innervation to the skin over the inferior portion of the rectus abdominis muscle. Interconnections often exist between the ilioinguinal nerve and the adjacent iliohypogastric nerve as the nerve continues to run medially and inferiorly, accompanying the genital branch of the genitofemoral nerve and the spermatic cord in men and the round ligament in women through the inguinal ring and into the inguinal canal. There is significant inter-patient variability of the sensory distribution of the ilioinguinal nerves secondary to this frequent overlap with the iliohypogastric, and occasionally the genitofemoral nerve. In the majority of patients, the distribution of the sensory innervation of the ilioinguinal nerve is to the upper portion of the skin of the inner thigh in men and women and the root of the penis and upper scrotum in men and the mons pubis and lateral labia in women.
Description of ultrasound guided technique
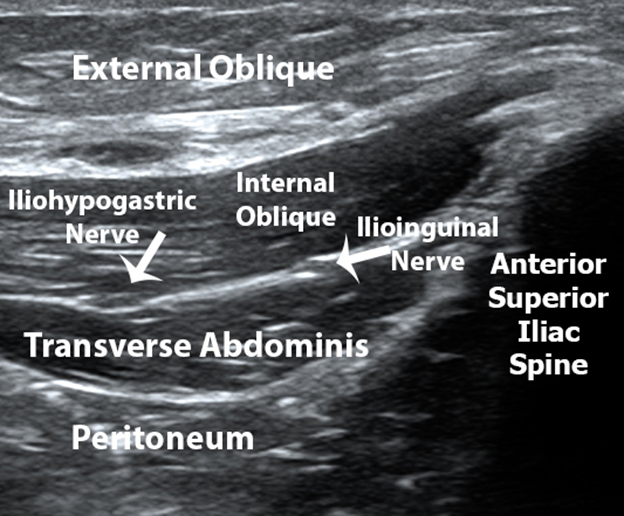
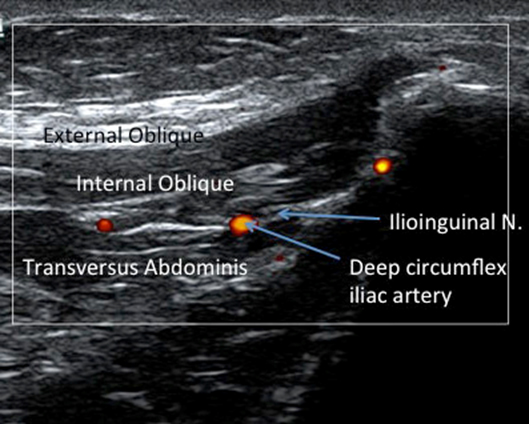
The anatomic landmarks of the anterior superior iliac spine and umbilicus are identified by visual identification and palpation. The inferior portion of linear high frequency ultrasound transducer is then placed over the previously identified anterior superior iliac spine with the superior margin of the transducer pointed directly in an oblique plane toward the umbilicus (Figure 1). The superior margin of the ultrasound transducer is then slowly rotated superiorly and inferiorly until the fascial plane between the internal oblique and transverse abdominis muscle is identified. The ovoid hypoechoic ilioinguinal nerve is then identified within this fascial plane (Figure 2). The iliohypogastric nerve may also be seen to be lying medial to the ilioinguinal nerve within this fascial plane. Color Doppler image is then utilized to identify the deep circumflex iliac artery which also lies within this fascial plane in close proximity to the ilioinguinal nerve so it can be avoided during ultrasound guided needle placement, decreasing bleeding complications associated with ilioinguinal nerve block (Figure 3) [5].

Figure 1. To perform ultrasound guided ilioinguinal nerve block, the inferior portion of linear high frequency ultrasound transducer is placed over the previously identified anterior superior iliac spine with the superior margin of the transducer pointed directly in an oblique plane at the ulbilicus.
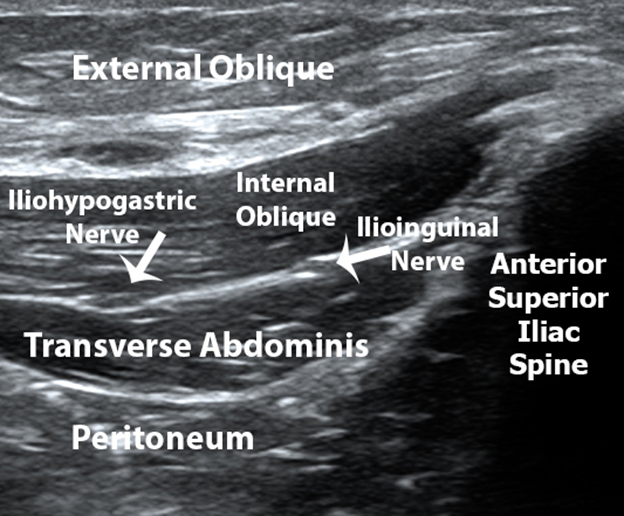
Figure 2. Oblique ultrasound image demonstrating the acoustic shadow of the anterior superior iliac spine and the muscles layers and facial plane containing the ilioinginal and iliohypogastric nerves.
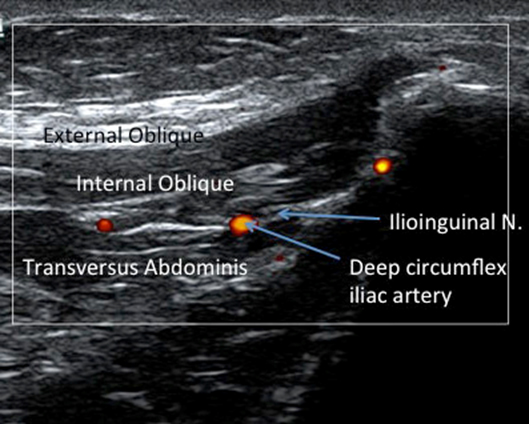
Figure 3. Color Doppler demonstration the relationship between the deep circumflex iliac artery and ilioinguinal nerve which both lie within the fascial plane between the internal oblique and transverse abdominis muscles.
After the ilioinguinal nerve and adjacent structures are identified, the overlying skin is prepared with antiseptic solution and a 11/2” 22 gauge needle is advanced using an in-plane approach from a point just below the inferior border of the ultrasound transducer toward the ilioinguinal nerve as it lies within the facial plane between the internal oblique and transverse abdominis muscle. When the needle tip is thought to be lying within the fascial plane adjacent to ilioinguinal nerve, a small amount of local anesthetic is injected under continuous ultrasound imaging to re-confirm the accurate placement of the needle tip. When proper needle tip placement is confirmed, gentle aspiration for blood is carried out, and if negative, 5 ml of local anesthetic is injected. Downward bowing of the transverse abdominis muscle will be observed on ultrasound imaging as the injectate enters the facial plane between the internal oblique and transverse abdominis muscles and spreads it apart. Minimal resistance to the injection should be encountered. If the painful condition being treated is thought to have an inflammatory component, 40-80 mg. of methylprednisolone may be added to the injectate. After the solution is injected, the needle is removed and pressure is placed at the injection site to decrease the incidence of needle-induced ecchymosis.
Conclusion
The use of the anterior superior iliac spine and the umbilicus as a guide when placing the ultrasound transducer simplifies the accurate placement of the ultrasound transducer when using ultrasound guidance to perform ilioinguinal nerve block. Furthermore, the use of ultrasound guidance when performing ilioinguinal nerve block will decrease the complications associated with this useful regional anesthesia technique when compared with complications associated with the traditional anatomic landmark guided technique [6]. The most dreaded complication of the anatomic landmark guided ilioinguinal nerve block is the inadvertent placement of the needle too deeply so the needle tip enters the peritoneal cavity which lies just beneath the transverse abdominis muscle [7]. Ultrasound guidance is able to clearly delineates the margin between the transverse abdominis muscle and the underlying peritoneal cavity, essentially eliminating the risk of improper needle tip placement into the peritoneal cavity. The ease of identification of the actual ilioinguinal nerve adds further accuracy to needle placement allowing for the use of smaller amounts of local anesthetic, which is especially beneficial when performing diagnostic or prognostic ilioinguinal nerve block where inadvertent spread of local anesthetic onto the adjacent iliohypogastric nerve may confuse the results and lead to incorrect interpretation [8].
References
- Waldman SD (2015) Chapter 86 – Ilioinguinal Nerve Block. In: Atlas of Interventional Pain Management (4thedn), W.B. Saunders, Philadelphia, 431-434.
- Waldman SD (2009) Chapter 175 - Ilioinguinal Neuralgia. In: Pain Review, W.B. Saunders, Philadelphia, 298-299.
- Chapman GA, Johnson D, Bodenham AR (2006) Visualisation of needle position using ultrasonography. Anaesthesia 61: 148-158. [Crossref]
- Mirjalili SA (2015) Chapter 45 - Anatomy of the Lumbar Plexus. In: Nerves and Nerve Injuries, edited by Tubbs RS, Rizk E, Shoja M, Loukas M, Barbaro N, et al. (Eds.), Academic Press, San Diego, 609-617.
- Vaisman J (2001) Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg 92: 1048-1049. [Crossref]
- Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B (2006) Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth 97: 238-243. [Crossref]
- McDermott G, Korba 2021 Copyright OAT. All rights reservet al. (2012) Should we stop doing blind transversus abdominis plane blocks? Br J Anaesth 108: 499-502. [Crossref]
- Demirci A, Efe EM, Türker G, Gurbet A, Kaya FN, et al. (2014) Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: comparison of the anatomical landmark and ultrasound guided techniques. Rev Bras Anestesiol 64: 350-356.