Hydatid Disease caused by Echinococcus granulosus is endemic in different parts of India including West Bengal. Bilateral lung involvement without involving liver and other potential sites in children is rather uncommon, and is less often described in the literature.
We diagnosed a three and a half years old girl with multiple large hydatid cysts in both her lungs. It caused significant cardio-respiratory compromise in the child, necessitating urgent thoracotomy and cyst removal, followed by anthelminthics to save her life.
multiple primary hydatid cyst, young child, bilateral lung involvement, thoracotomy
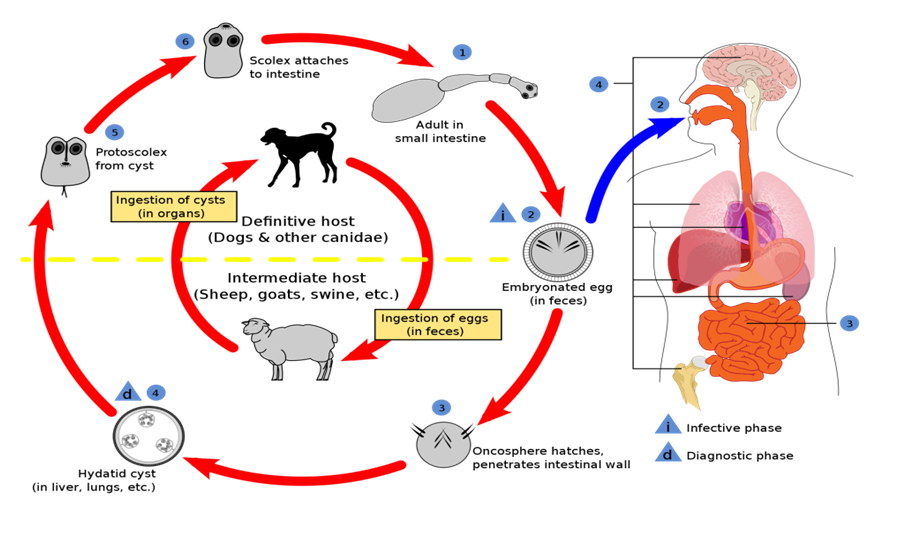
Hydatidosis is caused by larval stage (metacestode) of echinococci. It is a zoonosis with dog being definitive host and cattles (mainly sheep), the intermediate host [1-4]. Human beings acquire the disease only accidentally with the intermediate stage of the parasite. Food or water contaminated with eggs is the principal mode of infection whereas direct contact with dogs is implicated only rarely [2-5] (Figure 1).
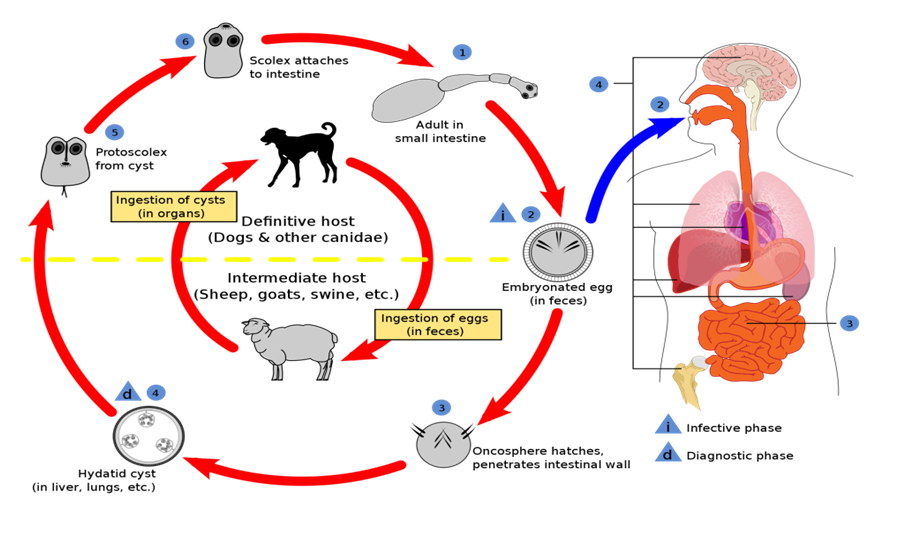
Figure 1. Life Cycle of Echinococcus
Clinical presentation of hydatidosis is often vague and non-specific. Symptoms are due to pressure effect or by release of its contents in corresponding organs. Liver (75%) and lung (25%) are the most commonly involved sites, the less common sites being muscle (5%), bones (3%), kidney (2%), spleen (1%), pancreas (1%) and central nervous system (1%) [1-4]. Serology and imaging modalities establish the diagnosis in most of the clinically suspected cases . Pulmonary involvement is not uncommon in children, but bilateral involvement by such huge cysts destroying lung parenchyma without affecting liver is rare [2-5].
A three and half years old girl, resident of West Bengal; a state in eastern India, presented with fever and non-productive cough for three months. She resides in city with no pet dogs at home and her neighbourhood. Fever was high grade, intermittent and relieved partially with antipyretics. It was associated with anorexia and weight loss. She also complained of intermittent pain in her right back. There was no history of haemoptysis, nausea, vomiting, pain abdomen, icterus or coughing out of cystic material. She also developed mild respiratory distress on running, after few months of symptom onset.
She was treated with oral antibiotics on outpatient basis, which gave only partial relief, but episodes of fever continued. Chest x ray showed cystic lesions in both lungs and oral albendazole was started by her physician without any further investigation.
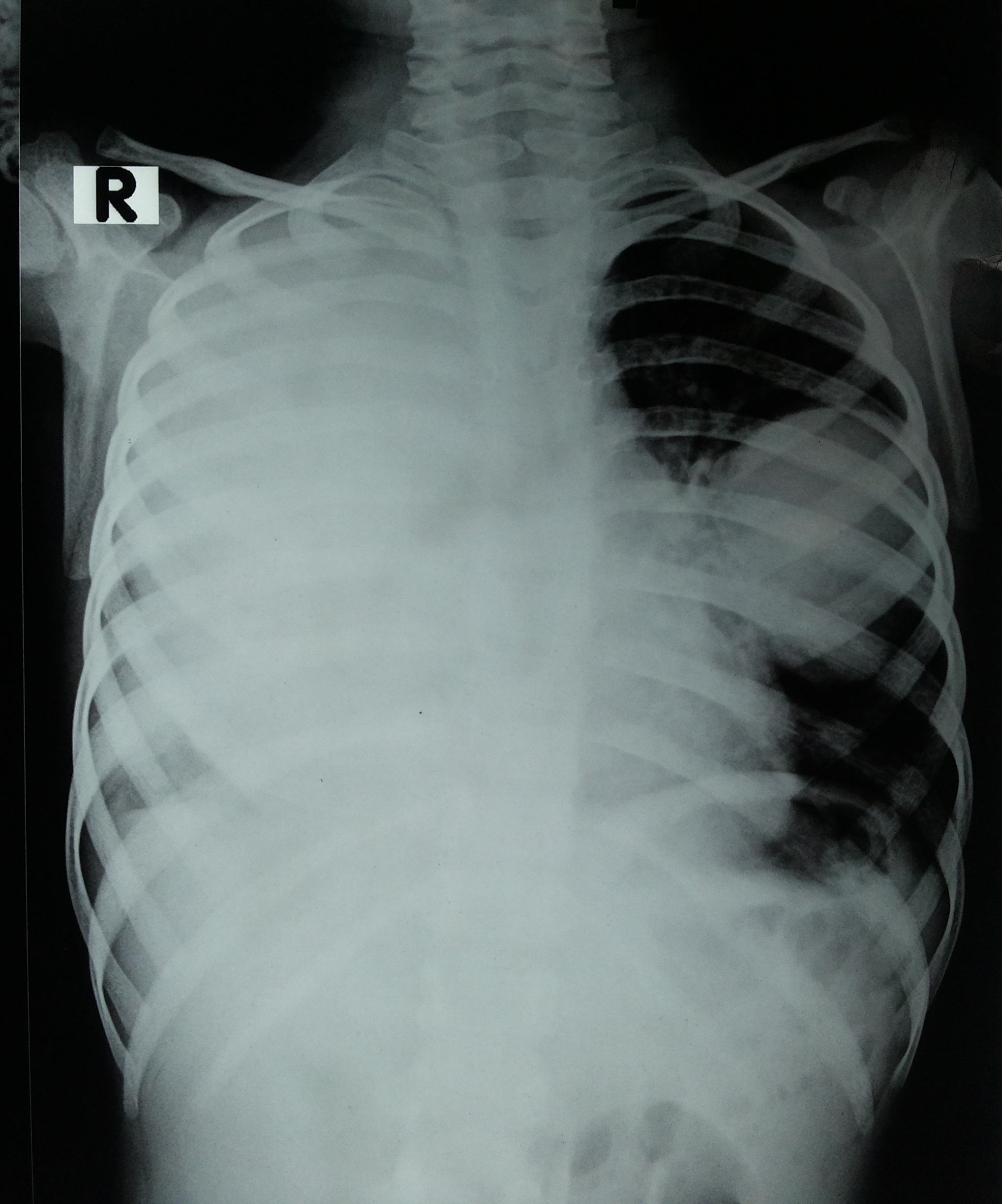
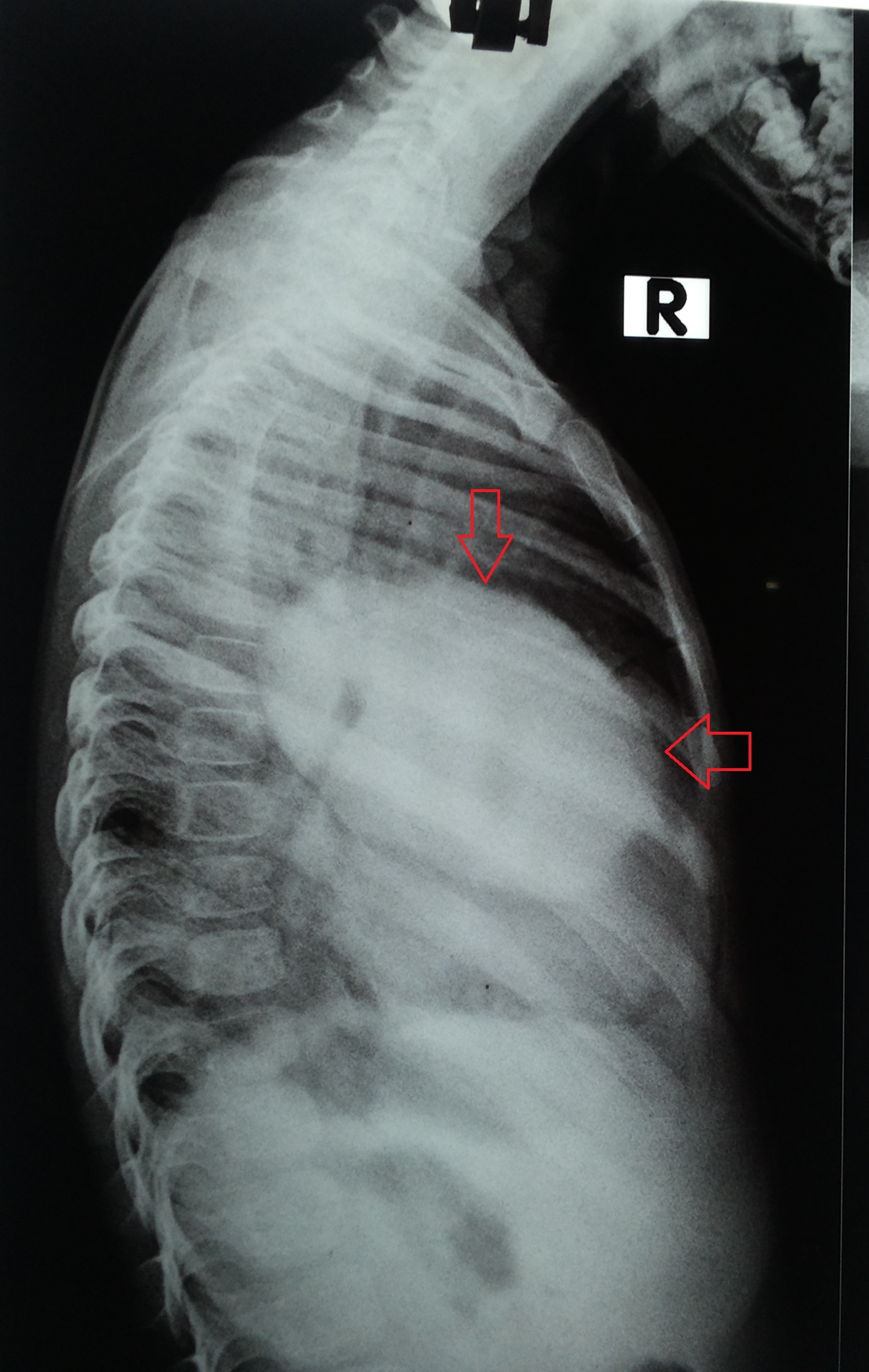
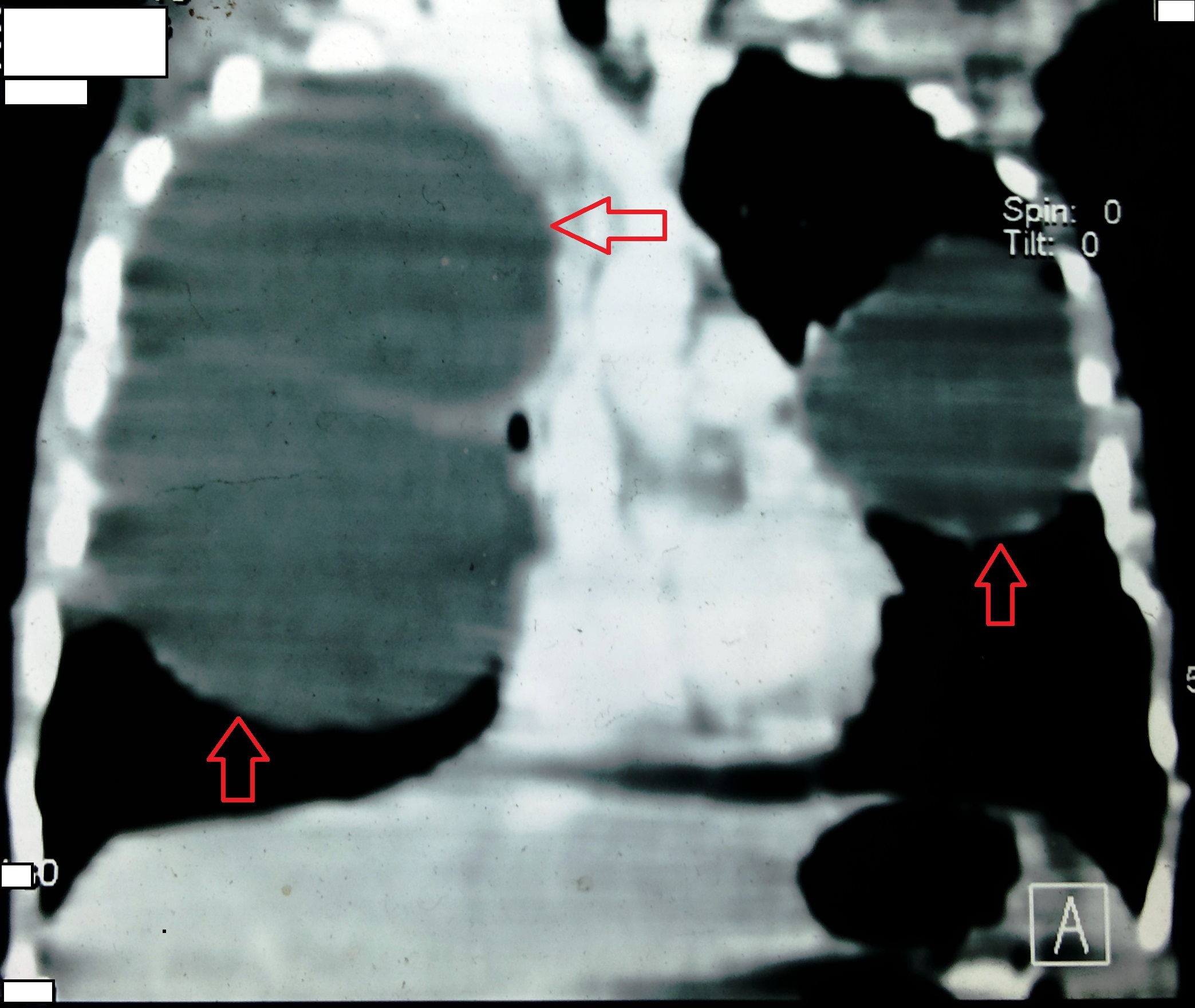
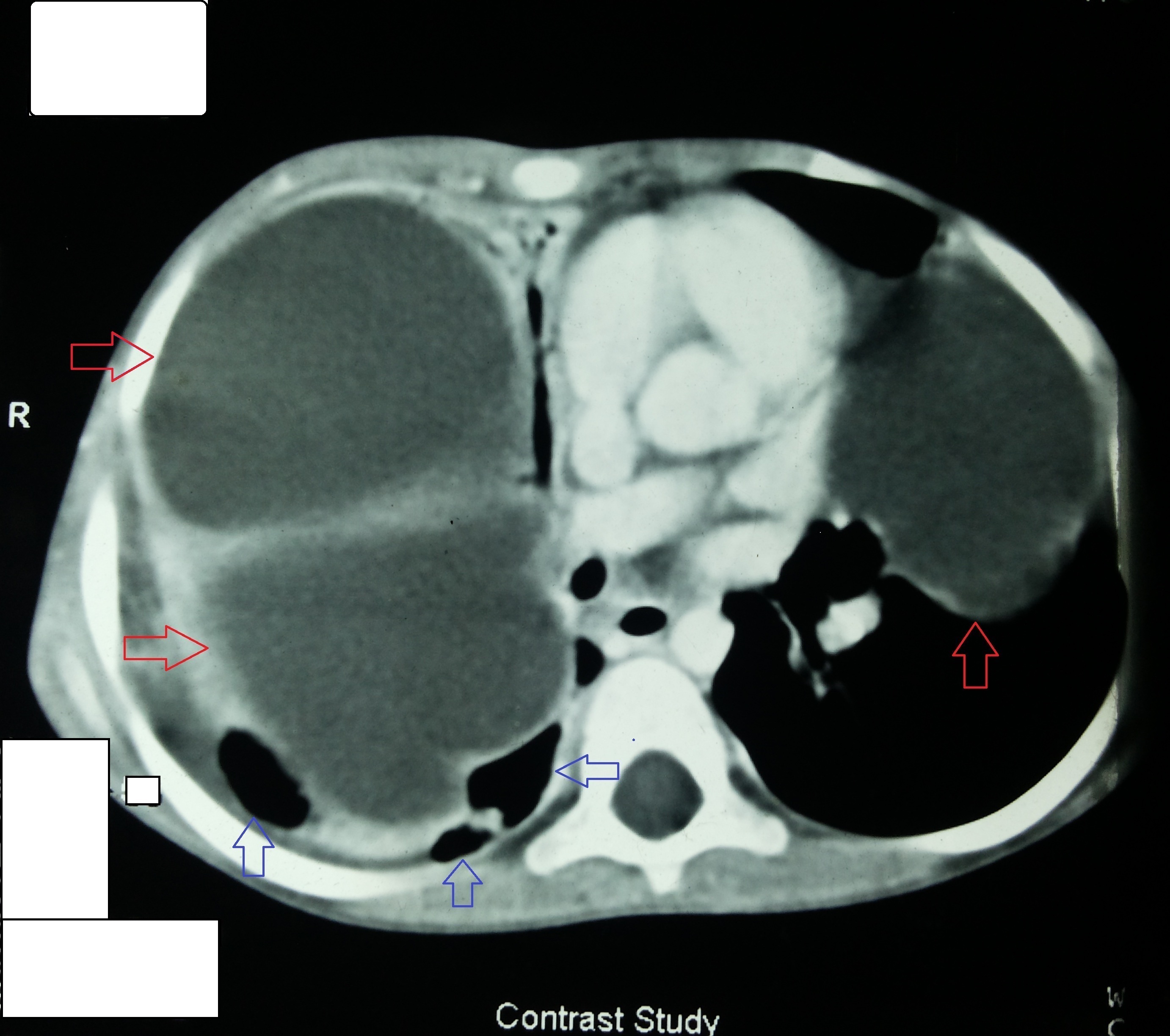
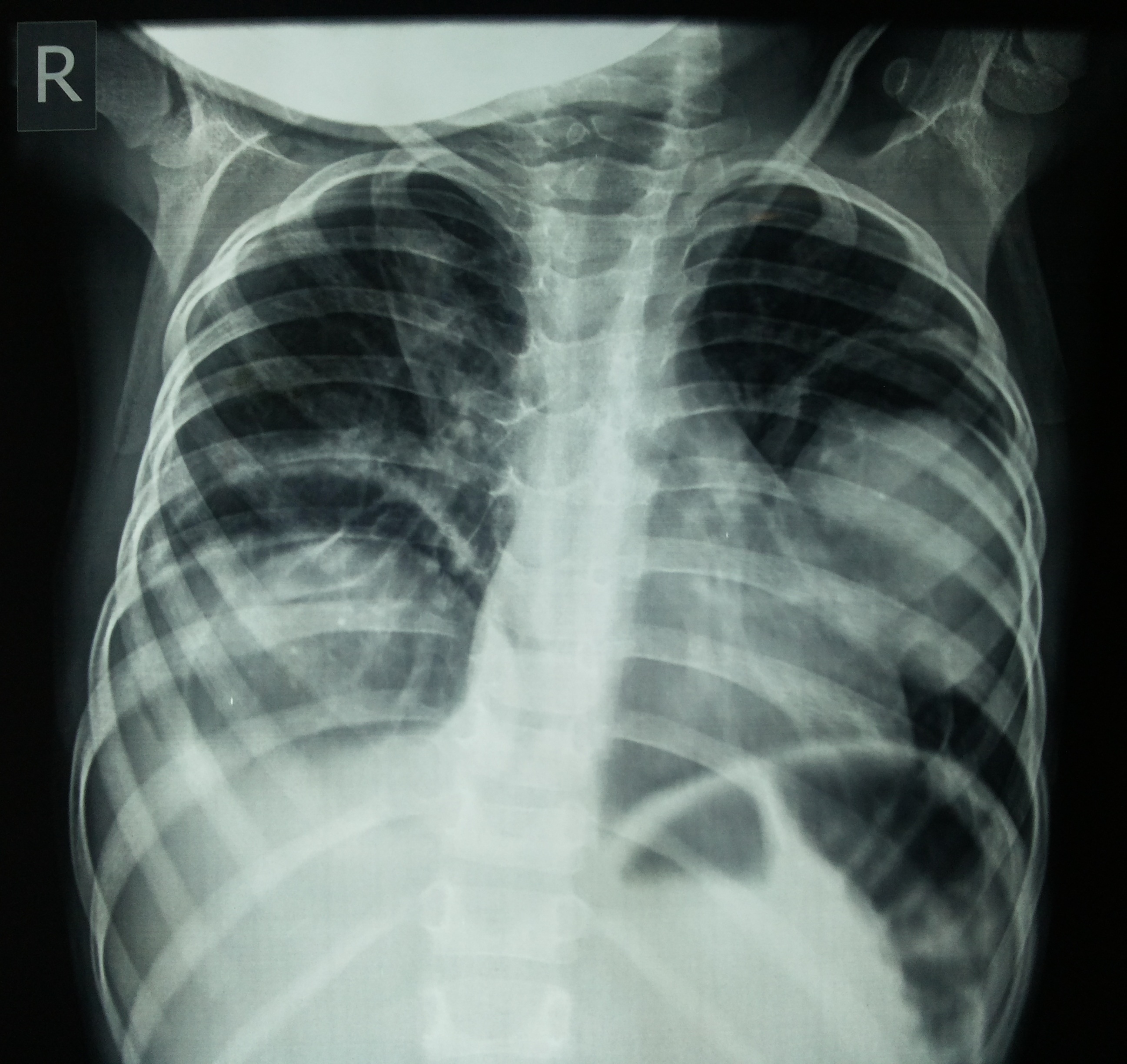
During admission we found her to be hypotensive, pulse was 117/min, very poor nutritional status, respiratory rate was 32/min. Chest examination showed diminished breath sound in right chest and left infrascapular, inframammary regions with occasional crepitations in left lung base. Her cardiovascular examination was unremarkable and abdominal examination revealed no organomegaly. There was no skin or soft tissue swelling anywhere in the body. Her blood picture showed lymphocytic leucocytosis (13900/cu mm). Chest X Ray on admission revealed homogeneous opacity in the right lung and a homogenous opacity with sharp borders in mid zone of left lung (Figures 2a and 2b). Thoracic and abdominal USG showed multiple cystic masses (the largest measured eleven cm) in right hemithorax and a cystic mass in left hemithorax without any abnormality in abdomen. Thoracic contrast enhanced CT showed cystic lesions in both lungs (Figures 3a and 3b) without any liver involvement (Figure 4). Serology for Echinococcus IgM was positive. HIV 1 & 2 (by rapid antibody card test, test kit batch no-4000012651, date of expiry-28.05.2015) , HBsAg, and Anti-HCV were non reactive.
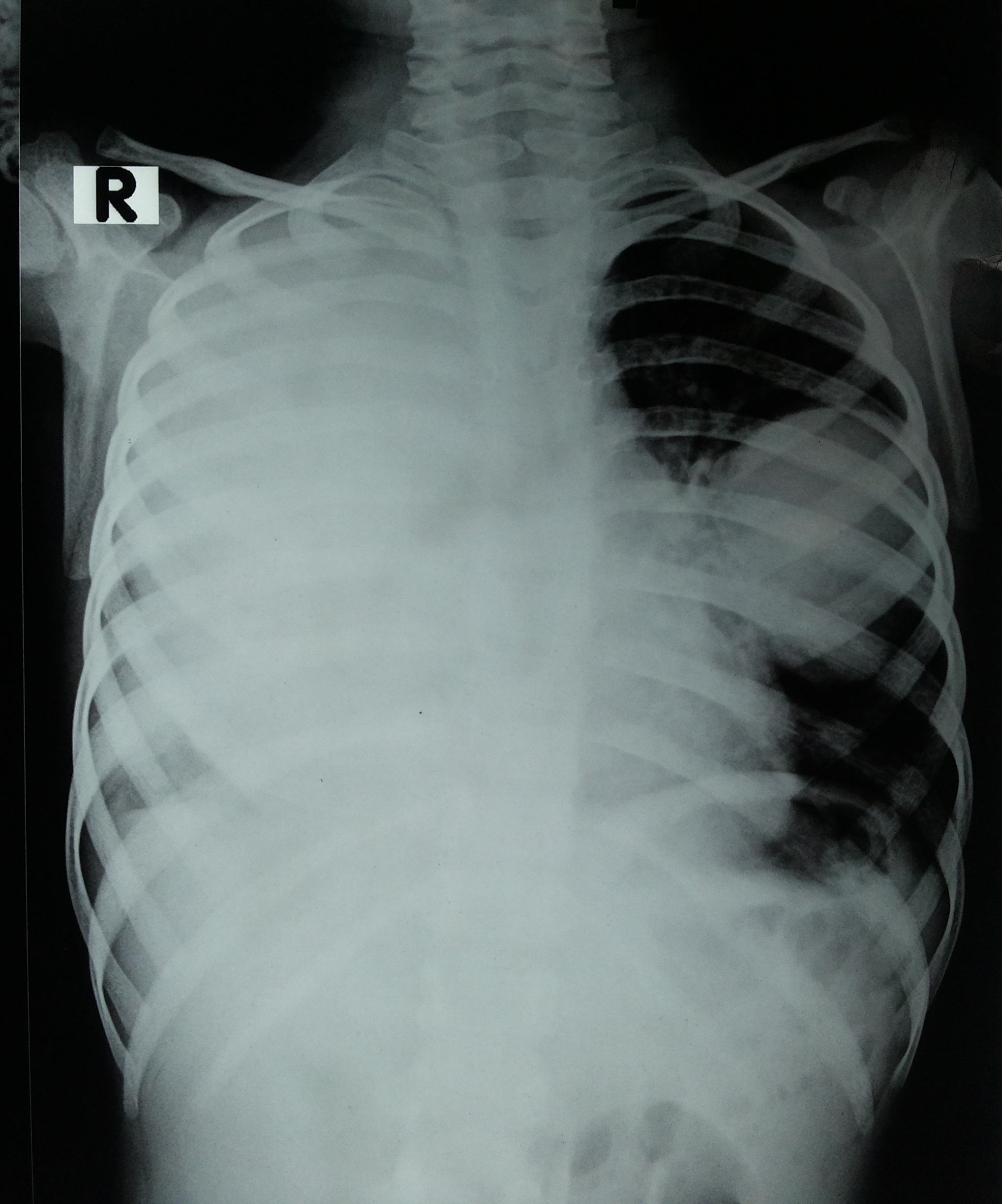
Figure 2a. Chest x ray PA view before treatment
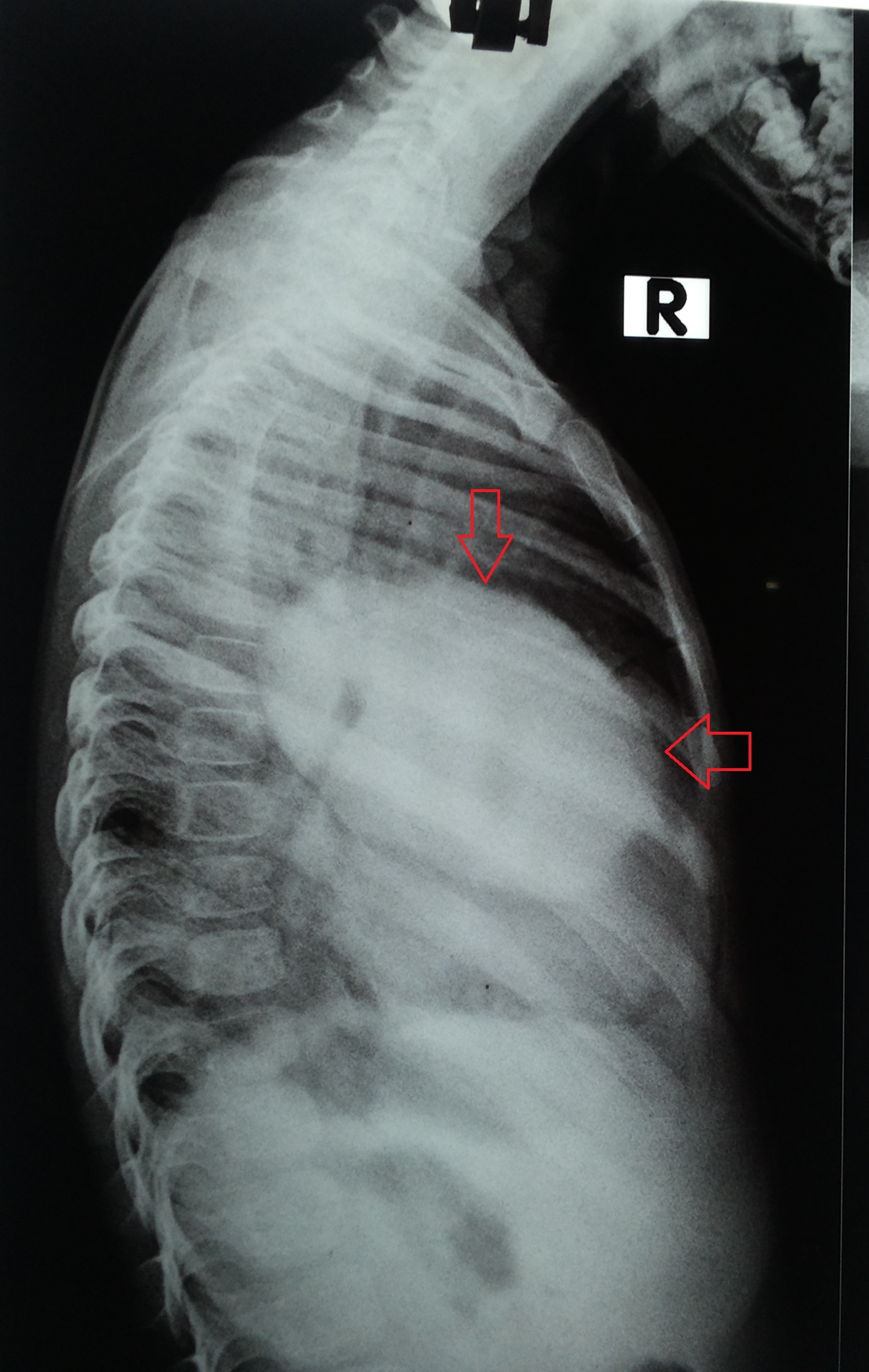
Figure 2b. Chest x ray lateral view before treatment showing cyst (red arrow)
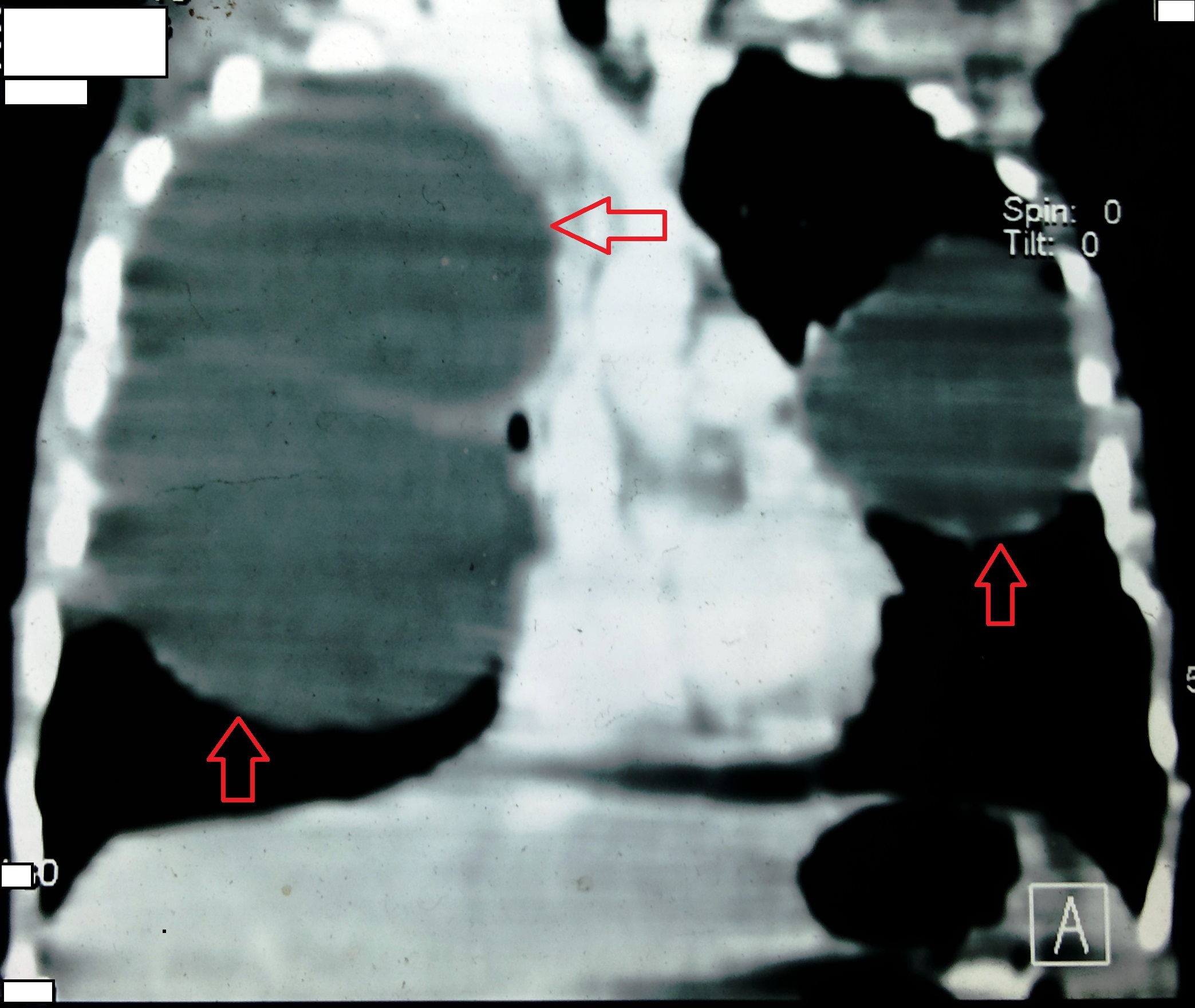
Figure 3a. CECT Thorax coronal section showing bilateral cysts (red arrow)
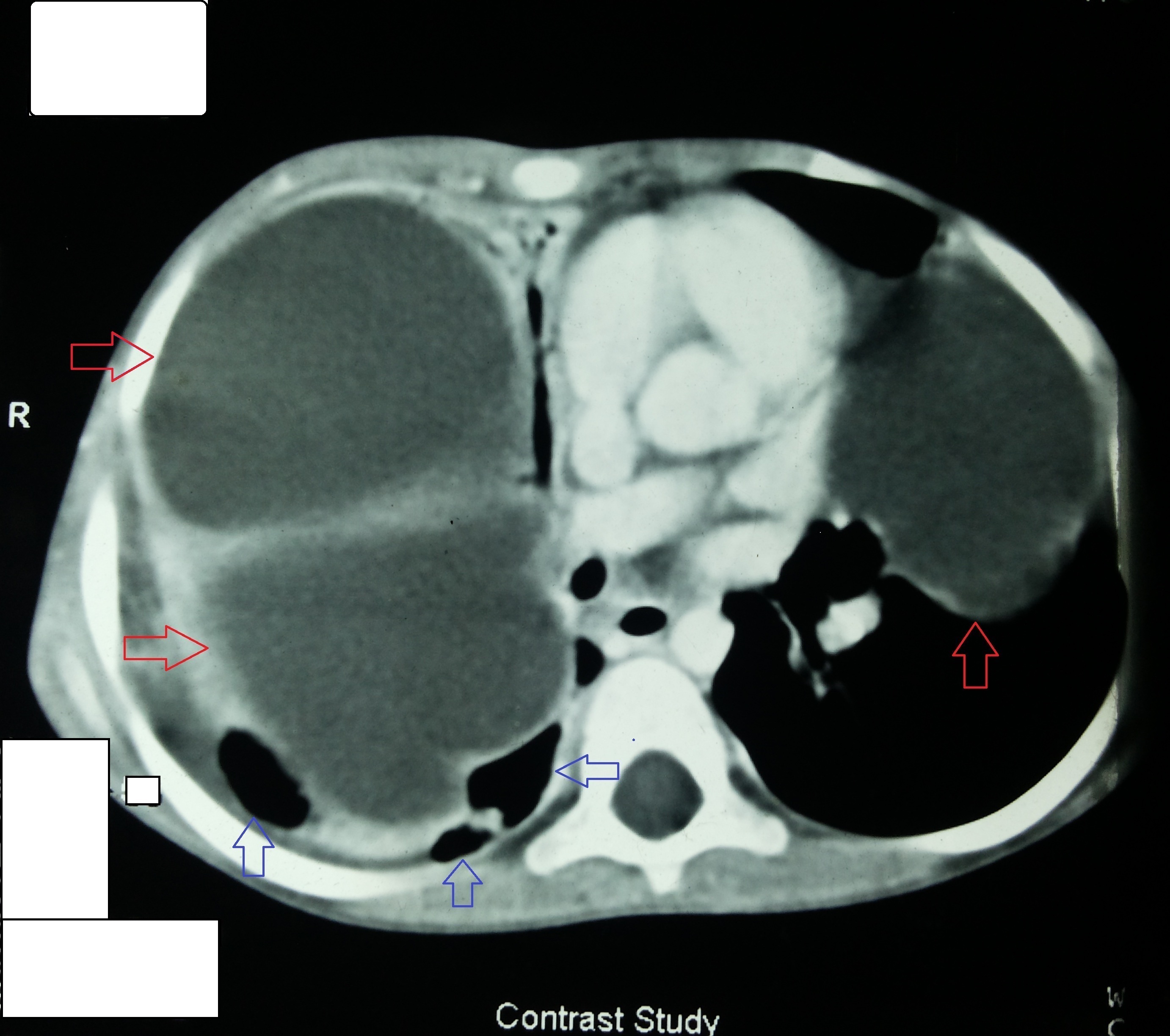
Figure 3b. CECT Thorax axial section showing bilateral cysts (red arrow), destroyed lung tissue (blue arrow)

Figure 4. Normal CT Abdomen
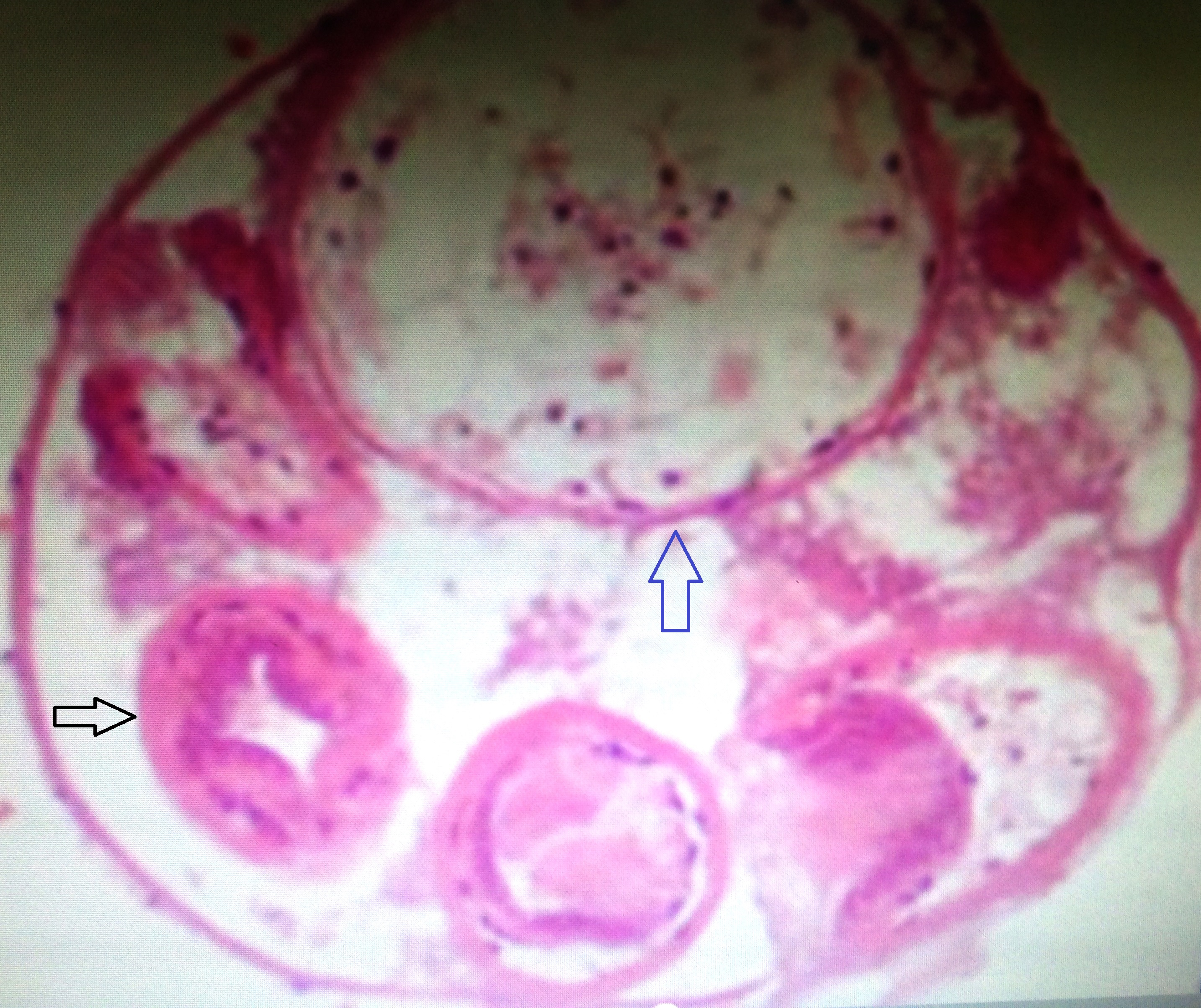
She received aldendazole again in a dose of 100 mg twice daily with nutritional support but her respiratory distress increased which necessitated urgent surgical intervention. Right posterolateral thoracotomy with removal of two huge cysts was done. Destroyed part of right lung was excised simultaneously. Histopathological examination of cysts confirmed the diagnosis of hydatid disease (Figure 5). Post operative phase was uneventful and she was shifted to general ward after three days stay in cardio thoracic intensive care unit. She is doing better now and is on oral albendazole (15 mg/kg). Post operative chest x ray shows significant improvement (Figure 6) of right lung field. She is now under regular follow up at our infectious disease OPD, and is awaiting second surgery for her left lung (Tables 1 and 2).
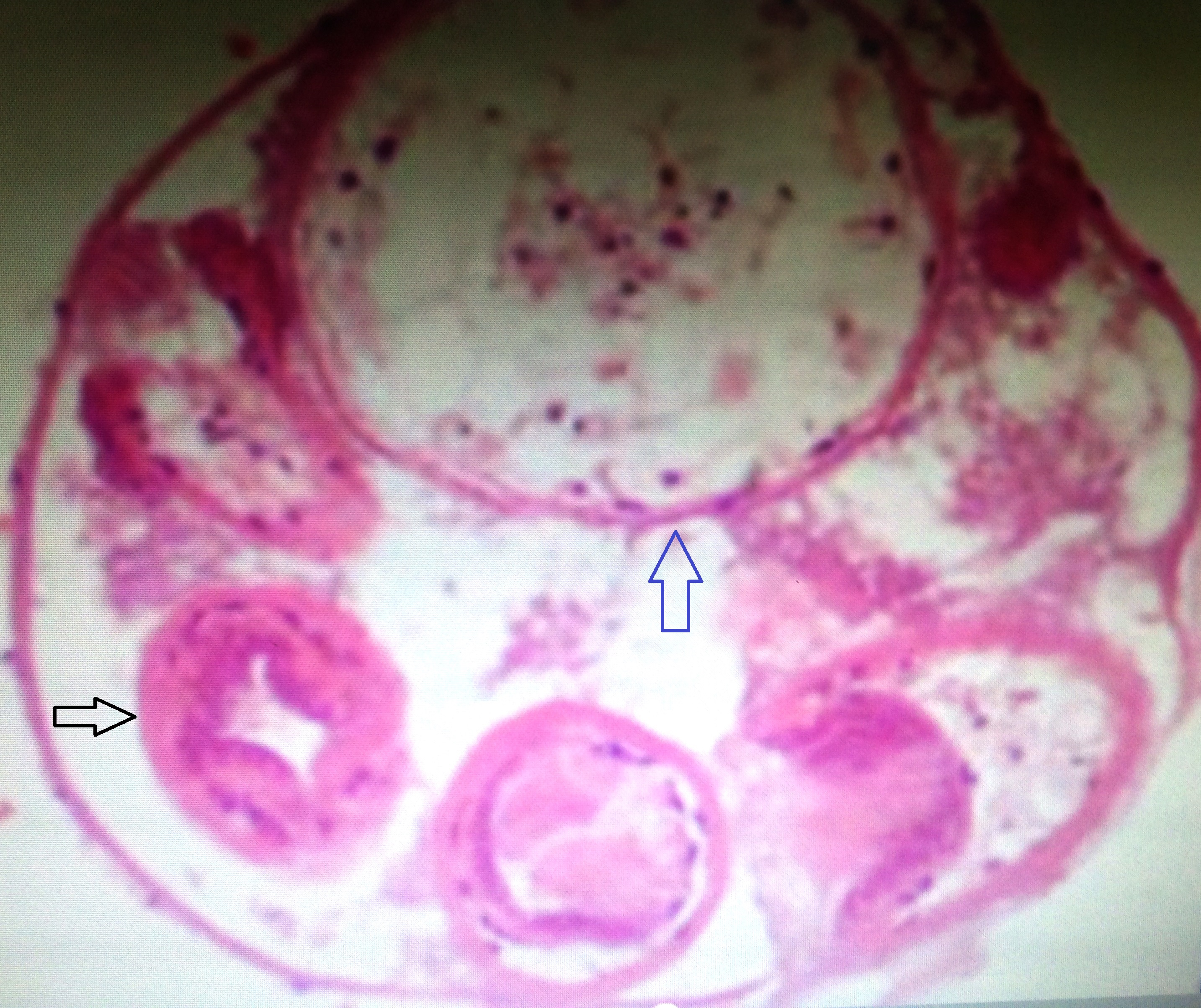
Figure 5. Histopathology of excised cyst (H & E stain) showing bronchiole (black arrow), cyst (blue arrow).
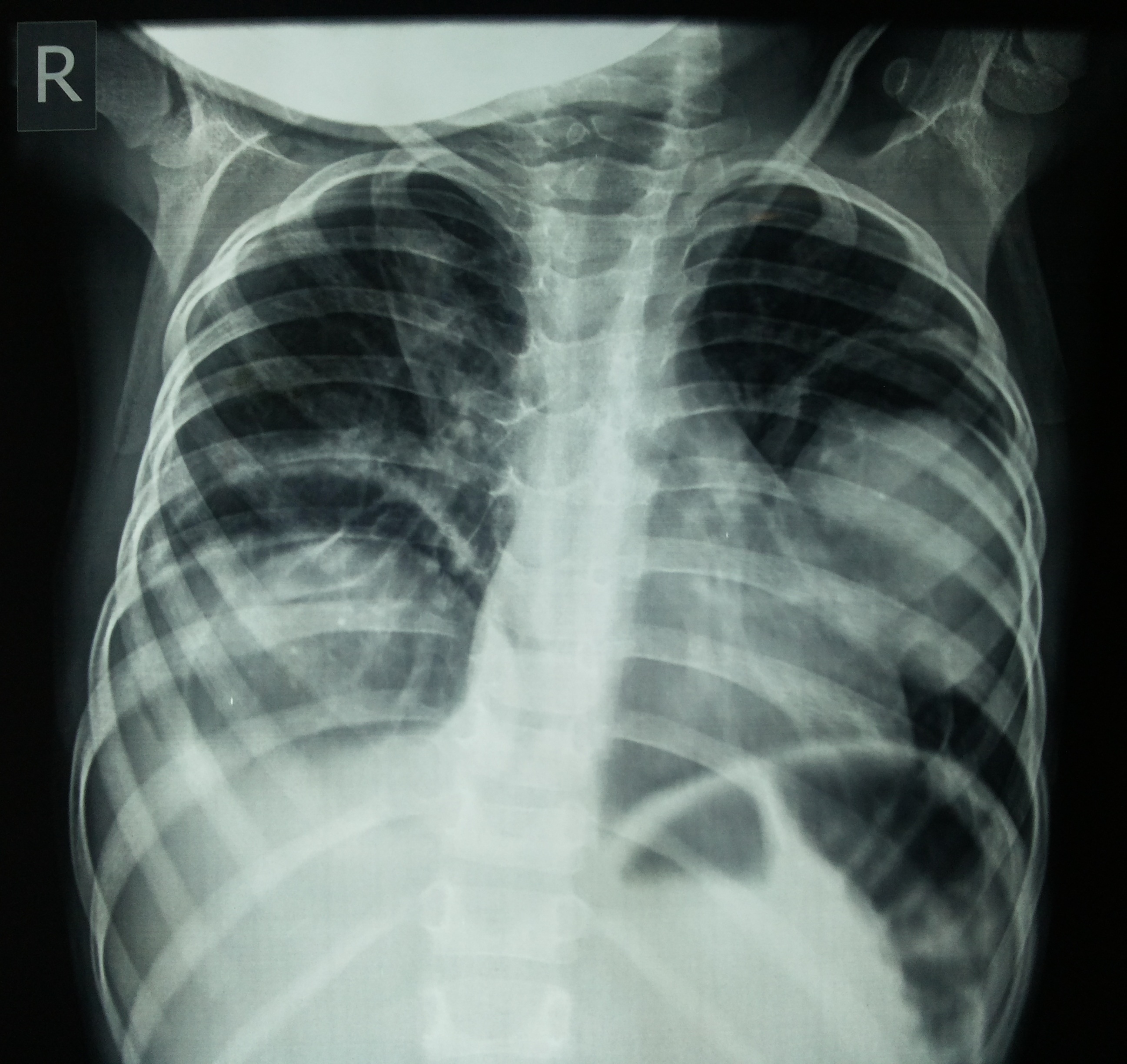
Figure 6. Chest x ray PA view after treatment
Table 1. Medical management of hydatid cyst
Indications |
Contraindications |
Inoperable primary liver or lung cysts
Cysts in two or more organs,
Peritoneal cyst and intraoperative cyst rupture |
Early pregnancy
Bone marrow suppression
Chronic Hepatic disease
Large cyst with risk of rupture
Inactive or calcified cyst
Bone cyst(Relative contraindication) |
Chemotherapeutic agents: |
Aldendazole - (10-15 mg/kg/day) for monthly cycles separated by 14 days interval. 3-6 total cycles.
Mebendazole - three to six months orally in dosage of 40-50 mg/kg/day.
Praziquantel, an isoquinoline derivative at dose of 40 mg/kg/day especially in cases where intraoperative spillage has occurred (limited data) [6]. |
Table 2. Surgical management of lung hydatid cyst
Procedure of choice: Complete excision of the cyst with maximum preservation of lung tissue.
Conservative surgical procedures: Enucleation
Pericystectomy
Cystostomy
Lobectomy
Segmentectomy
Principle of surgery: Evacuation of the cyst with removal of the endocyst, avoidance of contamination and management of residual cavity by drainage or capitonnage .Studies show that conservative surgeries achieve complete removal of cyst along with early mobilization. These simple procedures are safe, reliable and successful.
Radical procedures are undertaken in selected patients with specific indications.
Percutaneous aspiration method should not be performed in lungs.
Post operative albendazole 400 mg twice daily for three months is generally given in case of pre or intraoperative cyst rupture [7].
|
Hydatid disease is a helminthic infection caused by Echinicoccus granulosus and other Echinococci species. Dog is the definitive host and human being is infected only accidentally. The most common site for hydatid cyst in children is the lungs while in adults; it is liver [8]. Bilateral large multiple pulmonary cysts in a very young child as found in our case is relatively rare [9,10].
Because of the structure of the lungs allows expansion, hydatid cysts can attain a very large size [11,12]. In the studies done by Ali et al. [13] and Sehitogullari [14], the finding is that there is higher incidence of pulmonary than hepatic hydatid cysts in children and adolescents. The explanation given is that; the liver is a compact organ and the hepatobiliary capsule limits the cyst growth whereas the low resistance of lung tissue provides an excellent medium for rapid growth of hydatid cysts. Another study done by Abdol Hassan et al. [15] states that in children scolices have more ability to pass from liver barriers than in adults and it is due to less density of liver in them.
In the literature, no one collectively agreed on precise definition of a giant pulmonary hydatid cyst size. Lung hydatid cyst measuring more than 10 cm, in the largest diameter, is defined as giant [16]. Giant hydatid cysts of the lung; a distinct clinical entity, can be found in adolescents and children older than ten years in comparison to adults [11,17]. This predominance is explained by the immature immune system and relatively higher elasticity of the lung tissue in children and adolescents allowing rapid growth of cysts [18]. Giant hydatid cysts of the lung have been retrieved in 15% of 122 cases of childhood hydatid lung cyst in the study of Celic et al. [19] and in 26.7 % of 60 cases of childhood pulmonary hydatid cysts in the study of Kosar et al. [20]. Our study reports a case of giant primary bilateral multiple hydatid cysts of the lung in a three and a half year old female child.
The clinical manifestations of hydatid cysts depend on the site and size of the cyst. Usually hydatid cysts of lung are small or medium in size and are hardly symptomatic. Larger cysts may manifest with cough, breathlessness and symptoms of compression of adjacent organs. Commonest symptoms of patients with giant hydatid cysts reported, were cough (68–83%), chest pain (37–55%) and dyspnea (52%) [11]. Other symptoms encountered were fever (15%), haemoptysis (26%) and hydatoptysis (12%). In children with giant hydatid cysts additional symptoms found were chest deformity, expansion of involved hemithorax and growth retardation [11,16]. Our case presented with symptoms were fever, cough and weight loss.
Radiology is the investigation of choice for lung hydatids [16]. The commonest finding on the chest X-ray of patients with uncomplicated giant hydatid cysts is a smoothly outlined, dense spherical opacity with a largest diameter of more than 10 cm, occupying a part of an hemithorax or the entire hemithorax [16,21]. Usluer et al. [22] found that right lung is involved more than left lung and also right lower lobe is the most common location for cysts. In our case, dense opacity was seen in most of right hemithorax along with opacity in middle and upper part of left lung. Giant hydatid cyst of the lung is mostly seen as solitary and less commonly as multiple. [11,20]. The described case had multiple cysts in right lung. Inclusion of abdominal ultrasonography in the protocol of investigation is necessary because of the coexistence of hepatic cysts. The rate of coexisting hepatic and pulmonary hydatid cysts vary between 7% and 18% [24,25]. Topcu et al. [26] have reported a 13-year-old girl with a giant hydatid cyst of the lung associated to a giant hydatid cyst of the liver. In our case there was no involvement of liver.
Principal mode of treatment in pulmonary hydatid disease is surgery. The current treatment is complete excision of disease process with maximum preservation of the lung tissue [19,24,27]. Parenchyma - saving operations is more suitable for the patients with giant cysts [19,27]. Halezeroglu et al. [16] in their study of 47 patients with giant hydatid cysts applied surgical procedure preserving the lung parenchyma in 45 cases, only three patients required lobectomy. In our study, the two giant cysts were removed by thoracotomy along with pericyctectomy and removal of destroyed part of right lung.
Hydatid cyst of lung not being an uncommon disease in tropics can present with unusual clinical patterns. Our case depicts such an interesting and rare presentation in a three and half year’s old girl. Firstly, such a young age of onset is rarely found in the literature after extensive search. Secondly, bilateral, multiple, extensive, giant lung hydatid cysts had caused severe lung damage in this child. Urgent surgical intervention was needed to save the child. Thirdly, no other potential sites including liver are involved. Thus from our case it is evident that hydatid cyst should be considered as a differential diagnosis of congenital lung cysts in paediatric age group.
2021 Copyright OAT. All rights reserv
- Marla NJ, Marla J, Kamath M, Tantri G, Jayaprakash C (2012) Primary Hydatid Cyst of the Lung: A review of Literature: 2453
- Basavana GH, Siddesh G, Jayaraj BS, Krishnan MG (2007) Ruptured hydatid cyst of lung. J Assoc Physicians India 55: 141-145. [Crossref]
- Tekinbas C, Turedi S, Gunduz A, Erol MM (2009) Hydatid cyst disease of the lung as an unusual cause of massive hemoptysis: a case report. J Med Case Rep 3: 21. [Crossref]
- Shukla S, Singh SK, Pujani M (2009) Multiple disseminated abdominal hydatidosis presenting with gross hydatiduria: a rare case report. Indian J Pathol Microbiol 52: 213-214. [Crossref]
- Gupta RK, Gupta R: Bilateral Pulmonary cyst in a child. JK Science. Vol.10 no.2, April-June 2008
- Dr. Ashok Surybhanyi Gaybhiye et al. IOSR Journal of Dental & Medical Sciences. Vol-6, Issue-2(March-April 2013) 59-64.
- Yalcinkaya I, Er M, Ozbay B, Ugras S (1999) Surgical treatment of hydatid cyst of the lung: review of 30 cases. Eur Respir J 13: 441-444. [Crossref]
- Dogan R, Yuksel M, Cetin G, Suzer K, Alp M, et al. (1989) Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax 44: 192-199. [Crossref]
- Kuzucu A, Soysal O, Ozgel M, Yologlu S (2004) Complicated hydatid cysts of the lung: clinical and therapeutic issues. Ann Thorac Surg 77: 1200-1204. [Crossref]
- Balci AE, Eren N, Eren S, Ulkü R (2002) Ruptured hydatid cysts of the lung in children: clinical review and results of surgery. Ann Thorac Surg 74: 889-892. [Crossref]
- Karaoglanoglu N, Kurkcuoglu IC, Gorguner M, Eroglu A, Turkyilmaz A (2001) Giant hydatid lung cysts. Eur J Cardiothorac Surg 19: 914-917. [Crossref]
- Kurkcuoglu IC, Eroglu A, Karaoglanoglu N, Turkyilmaz A, Tekinbas C, et al. (2005) Surgical approach of pulmonary hydatidosis in childhood. Int J Clin Pract 59: 168-172. [Crossref]
- Ali R, Sajad R, Sina S (2009) Surgical Treatment of Pulmonary Hydatid Cystin in Children, Tanaffos 8: 56-61.
- Sehitogullari (2007) Our results in surgical treatment of hydaid cyst of the lungs. Euro J Gen Med 4: 5-8.
- Abdol Hassan Talaiezadeh, Sharif Maraghi. Hydatid disease in children: A different pattern than adults.
- Halezeroglu S, Celik M, Uysal A, Senol C, Keles M, et al. (1997) Giant hydatid cysts of the lung. J Thorac Cardiovasc Surg 113: 712-717. [Crossref]
- Arroud M, Afifi MA, El Ghazi K, Nejjari C, Bouabdallah Y (2009) Lung hydatic cysts in children: comparison study between giant and non-giant cysts. Pediatr Surg Int 25: 37-40. [Crossref]
- Symbas PN, Aletras H (2000) Hydatid disease of the lung. In: Shieds TW, Lociero J, Ponn RB, editors. General thoracic surgery. Philadelphia: Lippincott, Williams and Wilkins: 1113–1122.
- Celik M, Senol C, Keles M, Halezeroglu S, Urek S, et al. (2000) Surgical treatment of pulmonary hydatid disease in children: report of 122 cases. J Pediatr Surg 35: 1710-1713. [Crossref]
- Kosar A, Orki A, Haciibrahimoglu G, Kiral H, Arman B (2006) Effect of capitonnage and cystotomy on outcome of childhood pulmonary hydatid cysts. J Thorac Cardiovasc Surg 132: 560-564. [Crossref]
- Beggs I (1985) The radiology of hydatid disease. AJR Am J Roentgenol 145: 639-648. [Crossref]
- Usluer O, Ceylan KC, Kaya S, Sevinc S, Gursoy S (2010) Surgical management of pulmonary hydatid cysts: is size an important prognostic indicator? Tex Heart Inst J 37: 429-434. [Crossref]
- Lamy AL, Cameron BH, LeBlanc JG, Culham JA, Blair GK, et al. (1993) Giant hydatid lung cysts in the Canadian northwest: outcome of conservative treatment in three children. J Pediatr Surg 28: 1140-1143. [Crossref]
- Dogan R, Yuksel M, Cetin G, Suzer K, Alp M, et al. (1989) Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax 44: 192-199. [Crossref]
- Ulku R, Onen A, Onat S (2004) Surgical treatment of pulmonary hydatid cysts in children: report of 66 cases. Eur J Pediatr Surg 14: 255-259. [Crossref]
- Topcu S, Kurul IC, Altinok T, Yazici U, Demir A (2003) Giant hydatid cysts of lung and liver. Ann Thorac Surg 75: 292-294. [Crossref]
- Solak H, Yeniterzi M, Yuksek T, Anil N, Goktogan T, et al. (1990) The hydatid cyst of the lung in children and results of surgical treatment. Thorac Cardiovasc Surg 38: 45-47. [Crossref]