Abstract
Objective: To explore the clinical application of modified bone splitting techniques combined with GBR in implantation.
Methods: A total of 40 patients admitted to the department of implantation in our hospital from January 2017 to September 2017 were selected as the research objects. 51 implants were implanted with the modified bone splitting technique, including 13 Nobel implants, 13 ICX implants, and 25 tengoma implants. CBCT was taken on the day, 6 months, 1 year, and 2 years after restoration, and bone resorption at the implant's neck margin was measured.
Results: The average horizontal width of the tongue and lip of the alveolar crest was (3.35±0.38)mm before the modified bone splitting and (6.27±0.46)mm during the second operation, with an average increase of (3.28±0.53) mm. 40 patients were followed up for 1 to 2 years after the completion of the restoration. During the follow-up period, there was no loss of implant and good exercise function. X-ray examination showed no translucence around the implant.
Conclusion: The application effect of the modified bone splitting technique combined with GBR in clinical implantation is excellent and worthy of clinical popularization.
Key words
alveolar ridge,the modified bone splitting technique, implantation
Preface
Implant prosthesis is a new field derived from oral and maxillofacial surgery and prosthodontics in recent years. Implant prosthesis has become a routine treatment for dentition defect or loss because it can directly transfer masticatory force to the maxillary bone through the implant and achieve a good repair effect. However, due to a long time of tooth loss and the severe absorption of alveolar bone in most patients, it has brought significant future implant and repair treatment challenges. At present, it is considered that conventional dental implant surgery requires the alveolar ridge lip lingual thickness > of the implant area to be 5.5mm. Also, alveolar bone with a thickness of more than 1-2mm on the implant lip's lingual side to achieve aesthetic restoration effect [1]. At present, the horizontal bone increment methods include bone splitting technology, Onlay bone grafting technology, guided bone regeneration technology, and distraction osteogenesis technology, among which bone splitting technology is widely used [2].
Simion first proposed the bone splitting technique in 1992, which lengthwise divided the alveolar ridge into two parts and used a bone chisel to make the appearance of green branch fracture increase the width of alveolar bone. This technique is beneficial for alveolar ridge > 3.5mm and is recommended for 3 or 4 types of bone, with the maxilla superior to the mandible [3]. However, due to the traditional bone splitting technique's complexity, it often brings additional risks to the implant operation. The bone expansion and cleavage method combined with GBR in this paper are to make a transverse cleavage on the alveolar crest. Only create a longitudinal cleavage at the weakest part of the buccal alveolar bone at the implant position to form a natural green branch broken end and reduce surgery's difficulty. This study used bone dilatation and cleavage combined with GBR to implant patients with alveolar ridge width between 4.5mm and 5.2mm. The clinical efficacy of bone expansion and dehiscence combined with GBR is reported as follows.
Materials and methods
Clinical data
A total of 40 patients treated in the Department of Implantology of our hospital from January 2017 to September 2017 were selected, including 23 males aged 34-60 years, with an average age of 41.9 years. A total of 28 Nobel implants, 5 ICX implants, and 15 Denten implants were implanted. There were 17 female patients aged 25-62 years old, with an average age of 50.6 years old. There were 23 Nobel implants, 8 ICX implants, and 10 Denten implants. The alveolar ridge height of all patients in this group was more than 8mm, but the width was only 4.5-5mm, with an average of (4.7±0.38) mm. The teeth were distributed in the anterior teeth, premolars, and lower molars. None of these subjects had severe hypertension, diabetes, heart disease, or blood disease. In the 40 patients, 51 implants were implanted, of which 35 were single implants, and 16 were consecutive implants. Who informed all patients that bone dilatation and cleavage would be used in combination with GBR, and this study was reviewed and approved by the ethics committee of our hospital.
Instruments and methods
Instrument: ICX Implant System and Tools. Thin bone chisel produced by Kohler Germany. Kohler Germany manufactured bone splitters. Bone substitutes: Bio-OSS bone meal or hydroxyapatite bio ceramics. Membrane guide bone tissue regeneration: BIO-GIDE periosteum or HIO collagen membrane.
Method: The specific surgical procedures are as follows:
- Who performed preoperative CBCT examination of jaw bone to determine the available bone volume in the horizontal and vertical directions of alveolar bone in the area to be implanted. Who preliminarily had chosen the implantation location of the implant.
- A median incision at the alveolar crest was selected under routine oral and facial disinfection and local infiltration anesthesia. Vertical relaxation incision was made on the labial and buccal mucosa in the operative area's near and distal directions. The gingival flap was opened to expose the alveolar crest fully.
- Used the ultrasonic bone cutter to split the alveolar ridge horizontally along the alveolar ridges top. The length was between the lacunae near-far, and the depth was at least up to the cancellous bone. The bone splitting tool was then used to hit the alveolar ridge step by step according to the ideal direction of implantation, and the depth was 0.5-1.0mm greater than that of the implant length.
- An additional longitudinal incision was made on the labiobuccal bone plate at the implant position.
- Implant, implant Bio-OSS bone meal, the surface is covered with Bio-IDE collagen membrane and soft tissue flap is sutured tightly without tension. (6) Antibiotics were routinely applied after surgery for 3 days and suture removal after 10 days.(Figure 1,2)

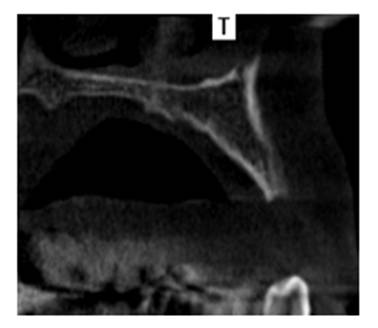
Figure 1.The modified bone splitting technique

Figure 2. Traditional bone splitting technique
Evaluation criteria
The implants' healing on X-ray radiographs was observed on the day after the second operation and 1 and 2 years after the crown and bridge repair.
Results
Clinical examination: Before bone cleavage, the mean horizontal width of the lip and tongue on the alveolar ridge's crest was (4.7±0.38)mm. During the second operation, the mean horizontal width of the lip and tongue on the anterior alveolar ridge's crest was (8.1±0.46) mm, and the mean width was increased by (3.4±0.53) mm.
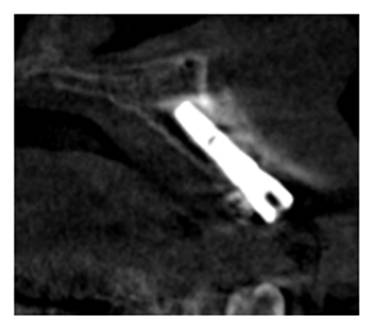
X-ray examination: The results showed that CBCT was taken on the day, 6 months, 1 year, and 2 years after completing the restoration (Figure 3, 4). There was no projection around all implants, and there was no statistical difference in the thickness of the labial-cheek bone plate measured on the neck of the implant (P > 0.05). The height of the labial and buccal bone plates measured by CBCT was decreased (0.72±0.12) mm in 1 year. This difference from the day and 6 months after the restoration was statistically significant (P= 0.021 and 0.018, respectively) but was not statistically significant from two years after the restoration (P= 0.072). (Table 1,2)
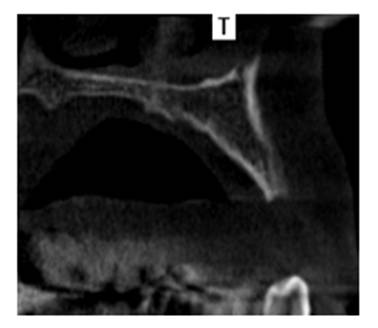
Figure 3. Preoperative alveolar ridge
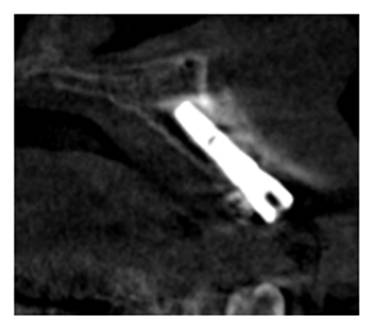
Figure 4. After implantation with modified bone splitting technique
Table 1. The thickness of labial bone plate of 51 implants(x(_)±s,mm)
Measuring Time |
The thickness of labial bone plate |
F |
P |
The day of restoration |
1.52±0.42 |
2.37 |
0.134 |
6 months after restoration |
1.48±0.51 |
|
|
1 year after restoration |
1.50±0.48 |
|
|
2 years after restoration |
1.47±0.53 |
|
|
Table 2. The reduction of height of labial bone plate of 51 implants(x(_)±s,mm)
Measuring Time |
The reduction of height of labial bone plate |
F |
P |
6 months afterrestoration |
0.28±0.05* |
4.61 |
0.016 |
1 year after restoration |
0.72±0.12 |
|
|
2 years after restoration |
0.81±0.15 |
|
|
Note: *Representatives compare with other groups snk-q test p < 0.05.
Conclusion
Due to long-time tooth loss, alveolar bone resorption has become the most common problem in implant surgery. According to Araujo,et al.[4], the horizontal absorption of the bone crest can reach 50%, and such absorption can occur in the horizontal or vertical direction. The lack of alveolar bone width will affect the implant's clinical design and is an essential factor influencing the implant's long-term success. Therefore, alveolar ridge broadening has always been the focus of implant research. At present, the horizontal bone increment methods include bone splitting technology, Onlay bone grafting technology, guided bone regeneration technology, and distraction osteogenesis technology, among which bone splitting technology is widely used. Bone splitting technology is considered to be a predictable method of high implant success. At present, bone splitting technology has been relatively mature with a high success rate. The traditional bone splitting technology also has some disadvantages, such as considerable trauma, easy bleeding, the labial bone plate easily absorbed by fracture, complicated operation. It is not easy for beginners to master, etc[2,5-7]. During bone cleavage, the buccal plate forms a fracture at the base of the bone, often resulting in a free fracture because the bone is hard to create, especially in the mandible. To increase the elasticity and activity of the bone, it usually needs to make longitudinal bone marks (bone groove) on the basal parts of the bone of the vestibular sulcus[8-11]. These bone marks need to be determined based on the bone condition of the mandible. They need to make a full-thickness flap to expose the bone of the vestibular sulcus' basal parts, which will inhibit microvascular perfusion between the mucoperiosteal flap the buccal plate. Thus affect the postoperative vitality of the buccal plate.
In this study, we changed some surgical methods based on the traditional bone splitting technology. Only a longitudinal additional incision was made on the labio-buccal bone plate at the implant site to make full use of the viscoelastic characteristics of the alveolar bone to form a natural green branch broken end to maximize the preservation of the alveolar bone. Compared with the two longitudinal incisions on the buccal side, the trauma was reduced, the free fracture of the labio-buccal bone plate was avoided, and the blood supply of the labio-buccal bone plate was ensured. From the point of view of the object of this study, the indication of bone expansion and splitting method is more suitable for 3-4 types of alveolar bone,with a certain height and width of 4.5-5mm, which is suitable for the area of anterior teeth, premolars, and mandibular molars. In cases with slightly better conditions, only one longitudinal incision was selected,compared with traditional bone cleavage, bone expansion and detachment combined with GBR reduced the risk of bone resorption and even necrosis due to the deterioration of blood supply caused by the longitudinal partition of alveolar bone[12-13]. Besides, the sensitivity of bone expansion and dehiscence combined with the GBR technique is also relatively low, increasing beginners' confidence. The observation results showed that the alveolar ridge's width was significantly widened after the modified bone cleavage, there was no projection around the implant, and there was no statistical difference in the thickness of the labio-buccal bone plate on the neck of the implant. The application effect was worthy of recognition. The paper on the bone split technology improved based on the traditional bone split changed the original bilateral longitudinal incision. It made only one single longitudinal additional incision on the lip buccal bone plate of the planting site. Make full use of the viscoelastic characteristics of the alveolar bone to form a natural green branch broken end, thus save the alveolar bone, avoid lip buccal bone plate free fractures. However, this surgical method takes advantage of the spatial expansion of the labio-buccal alveolar bone to some extent. To prevent the buccal alveolar bone's rupture due to excessive tension, the width of the case should be no less than 4.5mm. This surgical method has specific clinical feasibility and is worth popularizing.
In summary, in selecting suitable indications, bone expansion and dehiscence methods combined with the GBR technique are compared.
Reference
- Zehong G, Shulan X, Chunping Z (2018) Application of ultrasonic osteotome in modified osteotomy of mandibular posterior teeth. Journal of practical medicine3: 765-768.
- Elnayef B, Monje A, Lin GH, Gargallo-Albiol J, Hsun-Liang C, et al. (2015) Alveolar Ridge Split on Horizontal Bone Augmentation: A Systematic Review. Int J Oral Maxillofac Implants30: 596-606.[Crossref]
- Simion M, Baldoni M, Zaffe D (1992) Jawbone enlargement using immediate implant placement associated with a split-crest technique and guided tissue regeneration. Int J Periodontics Restorative Dent12: 462-473.[Crossref]
- Araújo MG,Sukekava F, Wennström JL, Lindhe J (2006) Tissue modeling following implant placement in fresh extraction sockets. Clin Oral Implants Res 17:615-624.[Crossref]
- Liu S (2017) Study on the application of osteotomy in oral implant bone augmentation. Systems medicine2: 136-139.
- Yamada M, Egusa H (2017) Current bone substitutes for implant dentistry. J Prosth Research 12: 1-11.
- Tolstunov L, Hicke B (2013) Horizontal augmentation through the ridge-split procedure:A predictable surgical modality in implant reconstruction. J Oral Implantol39: 59-68.[Crossref]
- Hang X, Zhigang X (2015) Application progress of osteotomy in dental implant. Journal of Clinical Stomatology31: 51-53.
- Hui X,Jinshuang W, Sefei Y (2017) Short term clinical observation of modified bone splitting technique in narrow alveolar ridge implant. Journal of oral and maxillofacial prosthodontics 18: 257-261.
- Xu Pu, Li Xiaoni, Xu Xing Huanyu (2016)Application of new technique of alveolar mucoperiosteal bone flap in dental implantation. Chinese Journal of Stomatology51: 688-689.
- Yang Yi, Zhu Zhijun, Li Ming, Ming S (2017) Application of secondary osteotomy in dental implantation for patients with severe mandibular bone insufficiency. Journal of Nanjing Medical University: Natural Science Edition37: 1668-1670.
- Yue Xilong, Xu Sheng, Liu Zhonghao, Zhou Wenjuan (2018) Comparative study on the clinical effect of bone splitting technique and onlay bone grafting technique in the aesthetic area of maxillary anterior teeth. Chinese Journal of dental implant23: 61-65.
- Wenbai Z, Xu Pu (2017) Research progress of secondary osteotomy in dental implant surgery. Journal of Modern Stomatology31: 357-360.