Abstract
Sepsis is one of the leading causes of death in the United States. In order to decrease the morbidity and mortality associated with sepsis in patients, early detection is vital, and so screening protocols have been developed. The Surviving Sepsis Campaign has developed an evidence based screening guideline that has been adapted by various institutions. Having specific criteria in detecting a septic patient is the defining factor in screening for sepsis by nursing staff. In order for the sepsis protocol to be effective, it is necessary that nursing and other front line staff be educated. Institutional barriers regarding implementation of protocol is another factor that still needs to be effectively addressed. This review will explore the benefit of implementing sepsis protocols within hospitals and many of the challenges that have already been faced.
Keywords
sepsis, surviving sepsis campaign, nurses, screening
Introduction
Sepsis is a severe and life threatening systemic inflammatory response to an infection that can ultimately progress to severe sepsis and septic shock. The underlying infection can be attributed to many pathogens, but it is most commonly caused by gram-positive bacteria followed by gram-negative in hospitalized patients [1]. Sepsis is among one of the leading causes of admission to the hospital and is associated with significant morbidity and mortality among patients. In the United States alone it affects more than 750,000 patients and accounts for 215,000 deaths annually [2]. When compared to patients hospitalized for various conditions those with sepsis were found to have a 75% longer average length stay [3]. Due to the length of stay and attention that septic patients require it imposes significant financial costs. In 2008, it was estimated $14.6 billion was spent on treating patients who were hospitalized for sepsis [4]. It is the most costly treated condition among hospitalized patients and out of the total combined costs for all hospitalizations in the United States it accounted for 5.2 percent of the spending [5]. Despite recent medical advances the incidence rate of sepsis has been shown to be increasing over the previous twenty years [2]. In order to decrease this trend early identification by nursing and screening is crucial to see a decrease in patient mortality. Management should be focused on early fluid and antibiotic administration. It was shown that for every hour there was a delay in the administration of appropriate antibiotic medications resulting in a decreased survival rate of 7.6% during the 6-hour period following the documentation of hypotension [6]. Even with early intervention, patients who developed severe sepsis and survived are more likely to develop considerable neurocognitive and physical impairments [7].
Screening for sepsis by nursing
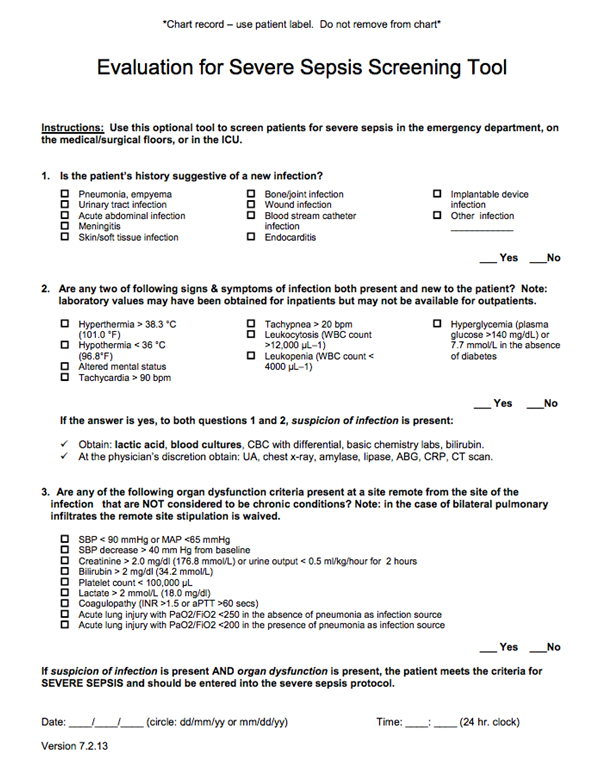
The increasing incidence of sepsis makes it an overall concern for hospital staff. As such, screening draws early detection to patients with potential to sepsis. Nurses are in a unique position of constant patient interaction; sepsis screening can be integrated to be a part of a nurse's daily routine. Nurses need to be adequately educated to identify and effectively treat sepsis. Unfortunately, identifying sepsis still poses big challenges[8]. First line healthcare staff needs to be properly educated on these symptoms and treatment to react effectively. Simple screening tools can be used to identify sepsis in patients. The Surviving Sepsis Campaign (SSC), has created evidence based guidelines to assist hospitals and staff in creating their own screening protocol (Figure 1). The latest update [1], brought together 68 international experts to assess the importance of various symptoms and treatments based on clinical evidence. The first step of the screening test identifies whether the patient has two or more features of Systemic inflammatory response syndrome (SIRS). SIRS is a group of reactions to nonspecific insult (Figure 2). Although SIRS can be due to multiple causes, when combined with an infection, it could indicate sepsis. At this point, patients should be monitored, particularly for signs of organ dysfunction. If at least one of the signs of hypoperfusion or organ dysfunction becomes present, the patient has progressed to severe sepsis. Furthermore, septic shock could occur if severe sepsis is associated with refractory hypotension (BP < 90/60) despite adequate fluid resuscitation and/or a serum lactate level > 4.0 mmol/L [1,9].
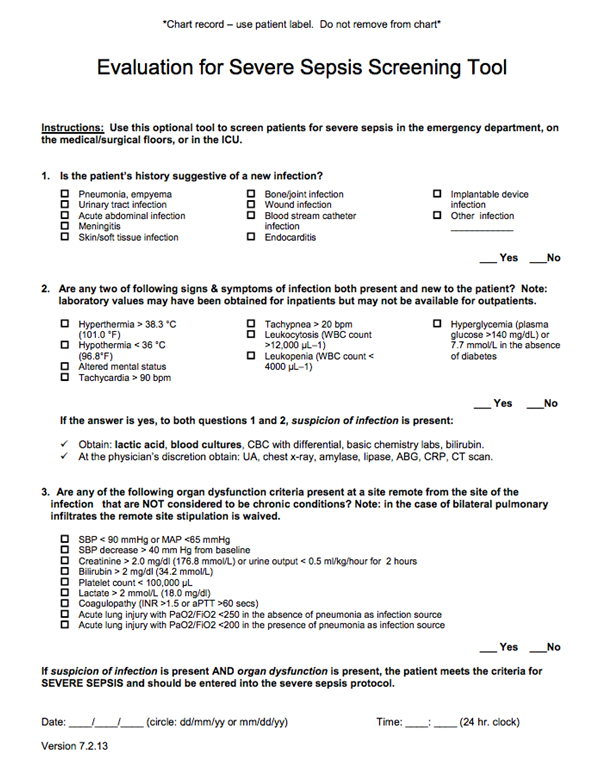
Figure 1: Evaluation for severe sepsis screening tool online at
http://www.survivingsepsis.org/sitecollectiondocuments/screeningtool.pdf
Systemic Inflammatory Response Syndrome |
Temperature >38.3°C, or <36°C
Heart Rate >90 bmp
Respiratory rate >20 breaths/min
White cell count <4 or >12 g/L
Blood glucose >7.7 mmol/L not diabetic
New altered mental state |
Figure 2: Criteria for Systemic Inflammatory Response Syndrome (SIRS). Adapted from McClelland H and Moxon A (2014) [9]
The goal is to prevent the patient from developing septic shock by immediate intervention of patients determined to have sepsis. Treatment generally involves collection of blood, for lactate, blood count and culture analysis, oxygen administration, fluids to prevent hypotension and antibiotics [1,9]. Two care bundles have been recommended by the SSC for management of severe sepsis, delivered within three hours and six hours of identification [1]. Daniels et al. 2010, created an alternative care bundle (The Sepsis Six Care Bundle), also endorsed by the SSC, as they felt certain elements in the previous bundle required critical-care skills that were not always available. The “Sepsis Six” was shown to improve care delivery in various clinical settings. It involves interventions that should be administered within one hour of identification, and can be started by nursing staff [10].
Certain populations are at a greater risk for sepsis, and need to be closely monitored. Paediatrics[11], the elderly, and those with comorbidities may have decreased capacity to fight infection compared to the general population. These populations may need more specific criteria when assessing for sepsis. By creating an easy to use sepsis screening tool, all nurses and healthcare staff should be adequately equipped to evaluate, diagnose and treat septic patients, decreasing the overall mortality rate of septic shock.
Although changes in protocols for sepsis screening by nurses are sometimes met with resistance [12], nurse driven implementation of sepsis protocols have shown to be highly effective in early identification and treatment of septic patients within the one hour goal [13].Tromp and colleagues performed a before-and-after intervention study (ED setting) in which compliance with the SSC care bundle improved significantly after the implementation of their nurse-driven program [14]. The completion of four of six individual elements improved significantly. These include measuring serum lactate (improved from 23% to 80%), taking a chest radiograph (from 67% to 83%), taking urine for urinalysis and culture (from 49% to 67%), and starting antibiotics within 3h (from 38% to 56%) [14]. According to Tromp et al., compliance with the SSC recommendations significantly improved after the introduction of a primarily nurse-driven, care bundle based, sepsis protocol followed by training and performance feedback [14]. Since nurses spend a significant amount of time at a patient’s bedside, they are most capable of recognizing, identifying and playing a critical role in early management of sepsis patients. Having nurses at the forefront of sepsis protocol implementation, has exponentially decreased sepsis mortality rate as previously discussed. As a result, nurses and physicians are able to collaboratively work together in order to implement effective patient care.
Development of nurse-driven sepsis protocol
When identifying a patient who fits all criteria of being septic, it is extremely important that nurses have a management plan implemented. As this is an on-going educational process for nurses all over the country, such management plans have been known to improve patient quality of care. According to Schell-Chapel and Lee, on the early detection and management of sepsis, there are two specific care bundles that management and care fall under, the 3 hour and the 6 hour bundle. It is expected that healthcare providers obtain blood lactate levels to identify tissue hypoperfusion, perform appropriate diagnostic tests including blood cultures prior to giving antibiotics in order to obtain an immediate diagnosis and lastly administering broad spectrum antibiotics to the patient within one hour of identifying that the patient is septic. Crystalloid IV fluids are then administered to the patient if the patient is hypotensive or has a persistent lactate level of 4mmol or higher. The patient makes a quick transition to a more advanced level of care during the 6 hour bundle. If hypotension persists, vasopressors are administered to the patient immediately. SSC guidelines recommend re-measuring lactate levels to evaluate the effects of fluid or vasopressor resuscitation, as well as measuring central venous pressure and central venous oxygen saturation in patients with septic shock to guide further interventions [15].According to Picard, O’Donoghue et al., a strong initiative toward improving patients quality of care was considered at the Beth Israel Deaconess Medical Center (BIDMC) in Boston, Mass. by implementing a sepsis protocol. The Multiple Urgent Sepsis Therapies Protocol was designed at BIDMC and it consisted of 8 treatment modalities [16].
Education for nursing staff was a vital component to establishing a highly functional protocol. It is extremely important that nursing staff are able to make a definitive sepsis diagnosis of a patient undergoing sepsis in order to decrease mortality. Not making accurate diagnosis posed to be a problem for many facilities as the protocol and educational awareness was being established. Therefore, educational modules and staff development workshops were put into place. Case based, high fidelity, hands on simulation sessions with interprofessional participation also posed as an option for clinicians to become educated on making a proper sepsis diagnosis [15]. Hospitals can have a significant impact on sepsis morbidity and mortality by developing policies and establishing evidence-based protocols as various initiatives have shown. According to the New York State Department Health (NYDOH), for example, since the implementation of Kaiser Permanente’s Northern California sepsis program mortality has been reduced for patients admitted to hospitals with sepsis, by more than 40 percent. It has saved more than 1,400 lives. Similarly, Regions Hospital in Minnesota reports that initiatives launched in 2005 led to more than a 60 percent drop in sepsis mortality by 2011, and Intermountain Health Care reports a reduction in its sepsis mortality rate from 25% to 9%, saving 85 lives and $38 million annually [17].
According to NYDOH, development and implementation of these evidence-based protocols will promote early identification and treatment of sepsis in hospitals by focusing on 5 key areas [17].
- Recognitionof risk factors, signs and symptoms of sepsis.
- Resuscitationwith rapid intravenous fluids and administration of antibiotics upon diagnosis of sepsis.
- Referralto appropriate clinicians and teams as appropriate.
- Measurementand evaluation of current practices for purposes of informing future policy.
- Quality Improvement measures that will permit development and dissemination of best practices through clinical and administrative information sharing [17].
In order to successfully decrease mortality in sepsis cases, hospitals need to establish and implement these evidence-based protocols and recommendations. But how are these protocols and recommendations developed? What determines the quality of evidence and the factors determining strong versus weak recommendations? Tables 1 and 2, adapted from the SCC International Guidelines for Management of Severe Sepsis and Septic Shock, highlight these points [1].
Underlying methodology |
A (high) RCTs |
B (moderate) Downgraded RCTs or upgraded observational studies |
C (low) Well-done observational studies with control RCTs |
D (very low) Downgraded controlled studies or expert opinion based on other evidence |
Factors that may decrease the strength of evidence |
1. Poor quality of planning and implementation of available RCTs, suggesting high likelihood of bias |
2. Inconsistency of results, including problems with subgroup analyses |
3. Indirectness of evidence (differing population, intervention, control, outcomes, comparison) |
4. Imprecision of results |
5. High likelihood of reporting bias |
Main factors that may increase the strength of evidence |
1. Large magnitude of effect (direct evidence, relative risk > 2 with no plausible confounders) |
2. Very large magnitude of effect with relative risk > 5 and no threats to validity (by two levels) |
3. Dose-response gradient |
RCT = randomized controlled trial |
Table 1. Determination of the quality of evidence
What should be considered |
Recommended process |
High or moderate evidence |
The higher the quality of evidence, the more likely a strong recommendation. |
(Is there high or moderate quality evidence?) |
Certainty in or similar values |
The more certainty or similarity in values and preferences, the more likely a strong recommendation. |
(Is there certainty or similarity?) |
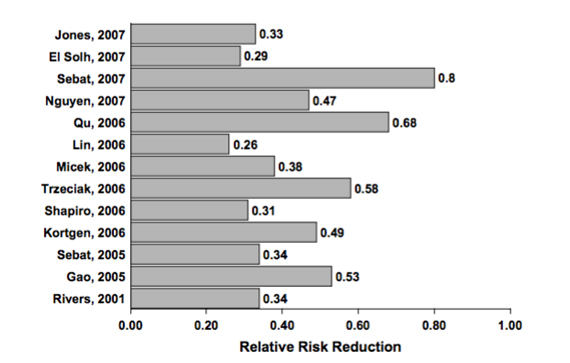
Figure 3: Sepsis protocol implementation reduces mortality risk [18]
Conclusion
Due to the increasing rate of sepsis amongst hospitalized patients, it was extremely important that proper screening protocols be implemented in hospitals nationwide as early as possible. The focus of the protocols should not only include proper screening and identification, but prevention as well. Educating the nursing staff, interdepartmental communication and collaboration in identifying patients who are septic has been the primary goal of these new protocols. As with any newly implemented protocol, there were initial roadblocks, however there has been significant improvement in the proper diagnosis of septic patients by proper education of all nursing staff which ultimately led to the decrease in patient mortality.
References
- Dellinger RP, Levy MM, Rhodes A(2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock 2012. Crit Care Med41:580-637.
- Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, et al. (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29: 1303-1310. [Crossref]
- Hall MJ, Williams SN, DeFrances CJ, Golosinskiy A (2011) Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief1-8.[Crossref]
- Wier LM, Levit K, Stranges E, Ryan K, Pfuntner A, et al. (2010) HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2008. Rockville, MD: Agency for Healthcare Research and Quality.
- Torio CM, Andrews RM (2013) National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160. Agency for Healthcare Research and Quality, Rockville, MD.
- Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, et al. (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34: 1589-1596.[Crossref]
- Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304: 1787-1794. [Crossref]
- Slade E, Tamber PS, Vincent JL (2003) The Surviving Sepsis Campaign: raising awareness to reduce mortality. Crit Care 7: 1-2. [Crossref]
- McClelland H, Moxon A (2014) Early identification and treatment of sepsis. Nurs Times 110: 14-17. [Crossref]
- Daniels R, Nutbeam T, McNamara G, Galvin C (2011) The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J 28: 507-512. [Crossref]
- Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. PediatrCrit Care Med 6: 2-8.[Crossref]
- Fowle E, Bettielou C (2011) Implementing a nurse driven sepsis protocol in the emergency department Registry of Nursing Research Conference Abstracts.
- Coates E, Villarreal A, Gordanier C, Pomernacki L (2015) Sepsis Power Hour: A Nursing Driven Protocol Improves Timeliness of Sepsis Care. J Hosp Med10.
- Tromp M, Hulscher M, Bleeker-Rovers CP, Peters L, van den Berg DT, et al. (2010) The role of nurses in the recognition and treatment of patients with sepsis in the emergency department: a prospective before-and-after intervention study. Int J Nurs Stud 47: 1464-1473.[Crossref]
- Schell- Chaple (2014) Reducing Sepsis deaths: A systems approach to early detection and management. American Nurse Today9:26-31.
- Picard KM, O'Donoghue SC, Young-Kershaw DA, Russell KJ (2006) Development and implementation of a multidisciplinary sepsis protocol. Crit Care Nurse 26: 43-54.[Crossref]
- New York State Department of Health. (n.d.) (2015).
- Rivers EP, Ahrens T (2008) Improving outcomes for severe sepsis and septic shock: tools for early identification of at-risk patients and treatment protocol implementation. Crit Care Clin 24: S1-47. [Crossref]
Editorial Information
Editor-in-Chief
Article Type
Review Article
Publication history
Received date: February 02, 2016
Accepted date: March 03, 2016
Published date: March 07, 2016
Copyright
©2016McCaffery M.This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
McCaffery M, Onikoyi O, RodrigopulleD, Syed Ali, Jones S, et al. (2016) Sepsis-review of screening for sepsis by nursing, nursedriven sepsis protocols and development of sepsis hospitalpolicy/protocols. NursPalliat Care 1: doi: 10.15761/NPC.1000109
Corresponding author
Murali G Krishna
MD, Division of Pulmonary, CriticalCare and Sleep Medicine, Orange Regional Medical Center (ORMC), 75 Crystalrun road, Suite 135, Middletown, NY -10941, USA, Tel: 1-917-951-9661; Fax:1-917-210-4307.
E-mail : murali.krishna.md@gmail.com
Underlying methodology |
A (high) RCTs |
B (moderate) Downgraded RCTs or upgraded observational studies |
C (low) Well-done observational studies with control RCTs |
D (very low) Downgraded controlled studies or expert opinion based on other evidence |
Factors that may decrease the strength of evidence |
1. Poor quality of planning and implementation of available RCTs, suggesting high likelihood of bias |
2. Inconsistency of results, including problems with subgroup analyses |
3. Indirectness of evidence (differing population, intervention, control, outcomes, comparison) |
4. Imprecision of results |
5. High likelihood of reporting bias |
Main factors that may increase the strength of evidence |
1. Large magnitude of effect (direct evidence, relative risk > 2 with no plausible confounders) |
2. Very large magnitude of effect with relative risk > 5 and no threats to validity (by two levels) |
3. Dose-response gradient |
RCT = randomized controlled trial |
Table 1. Determination of the quality of evidence
What should be considered |
Recommended process |
High or moderate evidence |
The higher the quality of evidence, the more likely a strong recommendation. |
(Is there high or moderate quality evidence?) |
Certainty in or similar values |
The more certainty or similarity in values and preferences, the more likely a strong recommendation. |
(Is there certainty or similarity?) |
The larger the difference between the desirable and undesirable consequences and the certainty around that difference, the more likely a strong recommendation. The smaller the net bene t and the lower the certainty for that bene t, the more likely a weak recommendation. |
Table 2. Factors determining strong vs. weak recommendation
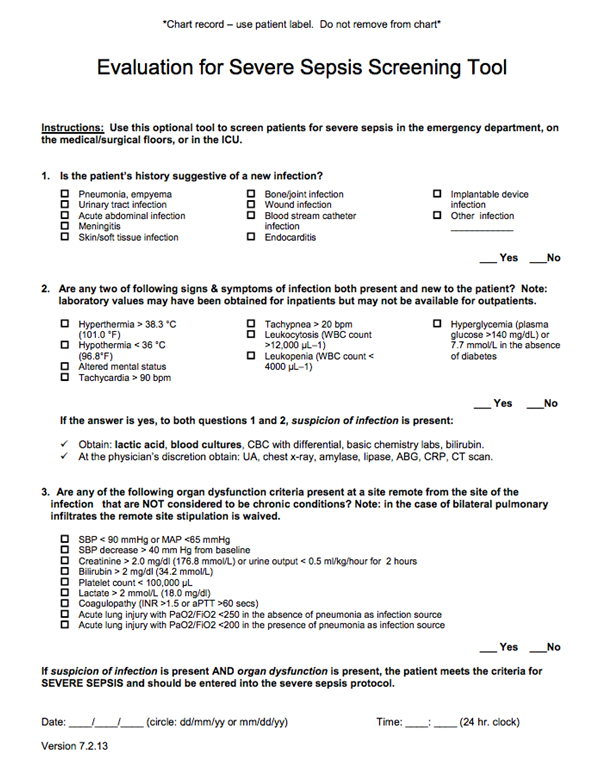
Figure 1: Evaluation for severe sepsis screening tool online at
http://www.survivingsepsis.org/sitecollectiondocuments/screeningtool.pdf
Systemic Inflammatory Response Syndrome |
Temperature >38.3°C, or <36°C
Heart Rate >90 bmp
Respiratory rate >20 breaths/min
White cell count <4 or >12 g/L
Blood glucose >7.7 mmol/L not diabetic
New altered mental state |
Figure 2: Criteria for Systemic Inflammatory Response Syndrome (SIRS). Adapted from McClelland H and Moxon A (2014) [9]
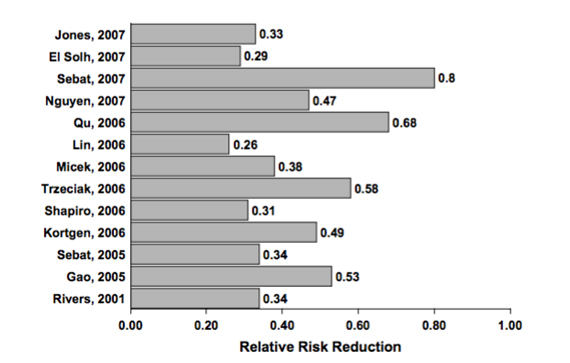
Figure 3: Sepsis protocol implementation reduces mortality risk [18]
Articles
 
|