Abstract
This third part shows the other side of the coin. After explaining the factors that regulate endothelial and coronary microvascular function (part A and B), we describe different methods and aspects that can be integrated with conventional medicine with considerable impact in terms of therapeutic effectiveness and of health care costs. We talk about nutrition and herbal medicine, exercise, mind-body disciplines, attention to emotions and to the psycho-social background of patients. And this is the answer to the crisis of the Western therapeutic model suggested by a relatively new current of thought in medicine: the Integrative Medicine.
What can be concretely done to modulate endothelial function in a healthy way?
The search for circuits, diagrams of relationships between organs and cells, the drawing of functional maps in the human body that are detached from the fixity of the organ anatomy, lead the recognition of the importance of continuous cross-talk between cells, organs and systems in both physiological and pathological conditions, based on the fine regulation of the levels of a large number of interconnected messenger molecules. Thus, it is possible to interpret the pathological phenomenon as an alteration in the communication between the cells, an imbalance in intercellular signalling [1]. These alterations of signals and dialogues, determine, over time, new balances and compensations within the PNEI network, with the possible final appearance of symptoms and the state we call “disease”. Each symptom is, after all, a message in PNEI terms. Nowadays is possible and we should understand the different messages to provide care. We must continue our researches free, in order to learn how to read these messages properly, resisting, sometimes, the temptation to write before knowing how to read.
From what is described up to now, it appears clear that the endothelial function can be understood as an epiphenomenon of a cellular stress condition, more than a primitive pathological condition. The regulation of coronary flow reserve and endothelial function in general, clearly shows the importance of PNEI factors in physiological but also pathological conditions and suggests the need to explore new therapeutic horizons [2].
The key to preventing and treating many disease processes relates to the modulation of allostatic load of each individual. This strategy relates to the ordinary life of each person and is independent of any form of drug therapy.
It is important to underline the concept of stress management and not stress elimination. Obviously, the stress response is important in an acute objective danger scenario. Furthermore, a bit of chronic stress is healthy (for example, a positive stimulating stress or a moderate physical activity lead to the release of IGF-1, TNFα, IL-4, IFNγ and the production of Brain Derived Natriuretic Factor (BDNF), promoting neurogenesis and mnemonic capacities [3]).
Alimentation and Herbal Medicine
Results from recent researches indicate that the active ingredients of foodstuffs and herbs affect the expression of genes related with neurotransmitters, hormones and cytokines in the PNEI network [4,5]. Therefore, PNEI interaction network and its modulation by aliments and plants open out new mechanisms to understand clinical results on health achieved by nutrition and herbal medicine and enriches current research on complex diseases as well as systems biology.
Epidemiological and clinical studies have demonstrated that natural products, in daily diet or phytomedical preparations, may improve vascular function by enhancing NO production and bioavailability [6]. Phyto-ingredients in tea, cocoa, pomegranate and soy are known to positively influence eNOS activity and/or endothelial function, in vitro and in vivo and could be considered as valuable and low-cost tools for the prevention or treatment of cardiovascular diseases [7].
Foods that we introduce in the diet are not only a source of calories but are important modulators of the nervous system [8-12], the endocrine [13-16] and immune systems [17,18]. Some diets heighten the inflammatory state, promoting development of diseases, through perturbations of host-microbe interactions [19-21]. Berer et al. demonstrated that the commensal gut flora-in the absence of pathogenic agents-is essential in triggering immune processes, leading to a relapsing-remitting autoimmune diseases [22-25]. Thus, a proper diet (such as Mediterranean diet [26-29] and Vegan [30,31] or Vegetarian diets [32-38]), acting on the different axes of the PNEI network, have positive effects in terms of treatment and prevention of various diseases [39], including cardiovascular ones [40-42]. In particular, it has been shown that an intensive nutrition education intervention, brings in 6-12 months to a lasting change in the eating habits of the patients, being able to get good benefits in terms of cardiovascular prevention (improved glycemic control, dyslipidemia, obesity and reduction of major cardiovascular events, such as myocardial infarction and stroke) [43-45].
Finally, a recent meta-analysis by Schwingshackl et al. [46] showed that the Mediterranean diet is accompanied by a decrease of inflammation parameters with an improvement in endothelial function. Similar results seem to be achieved also with the use of certain plants used in traditional Chinese [47] or Ayrvedic medicine [48].
The example of the diet can also be applied to the world of herbal medicine. The purpose of this work is not to explain the complex therapeutic effect of individual herbal compound(for this purpose please consult Firenzuoli et al. [49], or any herbal medicine book). We only limit ourselves to provide a list of the main herbs that currently find a concrete clinical application in CVD prevention and treatment, regulating endothelial function: dark chocolate, coffee, cocoa, green and black tea, Vitis Vinifera, Salvia miltiorrhiza, Ginkgo Biloba, blueberry (Vaccinium myrtillus) and cranberries, Garlic (Allium sativum), nutmeg oil, curcumin, soy beans, Paeonia lactiflora, Papaverine, Ginseng (Panax notoginseng), Hypericum, Vinca minor, Selenium, Ephedra, Licorice, Mistletoe (Vischium album), Hawthorn (Crataegus monogyna or Crataegus oxycantha), olive leaves (Olea europea), Ligustium wallichii, Jatropha podagrica, Stephania tetrahedron, Salvia miltiorrhiza, Uncaria rhyncophylla, Artemisia capillaris, Peucedanium praeruptorin, the family of the Gentianaceae, Paeonia suffruticosa, Equisetum arvense, hawkweed (Hieracium pilosella), couch grass (Triticum repens) and ribes nigrum, birch (Betulla alba), Orthosiphon, Guarana, Rutaceae family (Citrus, Barosma betulina, Ruta graveolens), Horse chestnut (Aesculus hippocastanum), Cypress (Cupressus sempervirens) and Amamelide (Hamamelis virgininana), Centella asiatica, Sweet Clover (Melilotus officinalis), Birch sap, Bermuda grass (Cynodon dactylon), the Dandelion (Taraxacum officinale) and the Artichoke (Cynara scolymus) or Hawkweed (Hieracium pilosella) [49].
In future it will be important to study precisely the effects of herbs on the PNEI network; effects that will indirectly affect the cardiovascular system and its state of health [49].
Physical activity
The aerobic exercise has been widely shown to be an important factor in cardiovascular prevention, being able to reduce oxidative stress and inflammatory parameters, to improve blood pressure, glyco-metabolic and insulin control and to optimize the sympathetic/parasympathetic balance acting on endothelial function in positive terms [50]. Regular physical activity and normal weight are both important indicators for a decreased risk of mortality from all causes, cardiovascular diseases and cancer: in particular physical activity has a strong independent effect on mortality [51] according to the fitness level and physical activity patterns [52]. Nowadays also neurologists and immunologists are studying the effects of physical exercise on the psychoneuroimmunologic network’s modulation [53-55]. Walsh et al. demonstrated that physical training can maintain immune health, especially with low to moderate load volumes and intensity programmes [56]. In particular, it is important to employ a gradual and periodised increase in training volumes and loads, adding a variety to limit training monotony and stress, avoiding excessively heavy training loads that could lead to exhaustion, illness or injury [56]. The direct link between physical activity and immune activity has been demonstrated by some interesting works of Nieman et al. [57-64] . The Authors demonstrated that walking five days a week, 45 minutes at a time and for 15 weeks, halves sick days for respiratory infections and revealed that a moderate daily physical activity of 30-45 minutes, invigorates the immune system, while if it is prolonged to 90 -180 minutes, after initial stimulation, making the body more susceptible to infections [65]. Chronic diseases such as cardiovascular disease, type 2 diabetes and cancer are associated with persisting low-grade systemic inflammation. It has been demonstrated that regular exercise induces anti-inflammatory effects with elevated levels of anti-inflammatory cytokines and suppression of TNFα production [66].
Bergh et al. have recently shown that exercise, to be an effective advantage in terms of prevention and treatment of cardiovascular diseases, must be accompanied by a good psychological resistance ability to stress [67]. In fact,low-stress resilience in adolescence is associated with increased risk of CVD in middle age. The association remains after adjustment for physical fitness: higher physical fitness is inversely associated with CVD risk; however, this is significantly attenuated by low-stress resilience [67].
Mind-body therapies for the prevention and treatment of cardiovascular diseases
What is written in the DNA code could change its phenotypic expression in response to the environment [68,69,70], through PNEI network mediators. The cardiovascular balance is influenced by this network (stress response) [71], whose organization is then transmitted to the offspring through epigenetic signatures [72] explaining the familiarity of many cases of CVD or why migrants acquire the same CVD risk of the new region they are living in [73,74].
Thus, individual lifestyle and the surrounding environment are so important because can effectively modify the transgenerational inheritance of stress axis balance and/or its activation and function during our life (with all the consequences on our health) [75].
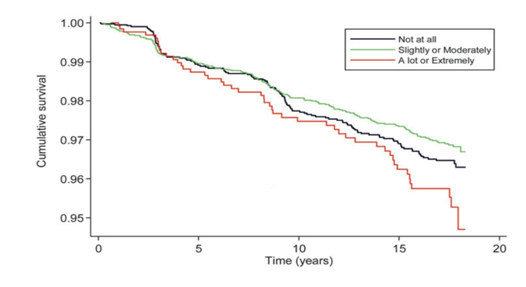
The effects of physical exercise, diet and smoking cessation on CVD prevention and treatment are well known. However, tests have shown that myocardial ischemia can be elicited by mental stress in a laboratory and in everyday life and that ischemia induced by mental stress is associated with an increased risk for future cardiac events in patients with coronary artery disease (Figure 1 shows the survival curves according to coronary heart disease related to perceived stress impact). Behavioral and stress management interventions offer additional benefit over and above standard medical care in cardiac patients with evidence of myocardial ischemia [76], especially considering the lack of efficacy of standard beta-blocker therapy on low heart rate-related ischemia during mental stress [77], or the inability of the standard ergometric tests (exercise or pharmacological stress) to exclude the presence of inducible ischemia because not able to detect the form of myocardial ischemia induced by mental stress [78].
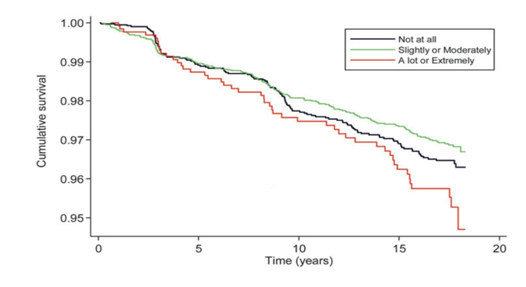
Figure 1. Kaplan-Meier survival curves showing the association between the perceived impact of stress and incident coronary heart disease adjusted for sociodemographics, health behaviors, biological cardiovascular disease risk factors, self-rated health, negative affect, psychological distress, social support and perceived levels of stress (Modified from [393]).
Our inner dialogue modulates cardiovascular function: At the same event, people experience different emotional reactions and a same person during his/her life and maturation could react differently in similar, specific situations. Between event and emotion there is no automatic link.
According to Rozanski et al. specific personalities and their characteristic psychological traits (depression, anxiety, character traits, social isolation, and chronic life stress) contribute significantly to the pathogenesis and expression of coronary artery disease (CAD) because of adverse health behaviors (such as poor diet and smoking) and direct biological mechanisms, such as immune, neuroendocrine and platelet activation [79].
Thus, the concept of “personality”(namely “the individual differences in characteristic patterns of thinking, feeling and behaving” [80]) represents a key factor in regulating the health of the cardiovascular system.
Emotions do not automatically take away from what happens in people's lives, but are derived from the type of internal dialogue that is done compared to what happens. Different personalities are more or less vulnerable to stress, with relationships exiting between different personalities and the function of the hypothalamic-pituitary-adrenal (HPA) axis [81-85] and immune [86,87] and nervous systems [88]. Different patterns of thinking, feeling and behaving essentially modulate the cross-talk between the nervous, endocrine and immune systems. It is just as true that the nervous, endocrine, immune and metabolic systems and their function could influence mental attitude [89].
In particular, “type D” personality or the “type A coronary-prone behavior”, according to Friedman and Rosenman-1974, are related to higher incidence of CVD [79,90].
Although with many nuances, it can be said that every human being can only try two great emotions in their lifetime: love (serenity, tranquillity) or fear. And never at the same time [91]. It oscillates constantly between these two poles. An inner dialogue oriented to the past or the future that is full of anxiety, distrust, jealousy, envy, ambition, regret etc. produces fear, in its various emotional colors. An inner dialogue turned to the present, concrete, confident, proactive, compassionate, conscious etc., produces feelings of "love" , serenity and tranquillity [91].
In general, as described by Stegagno et al. [91], right cerebral hemisphere activity is prevalent during emotion recognition or expression (in particular for negative emotions) and during “keeping away” reactions. The left hemisphere is dominant in positive affective states and when seeking reactions.
According to the same author [91], different neuromediators act on neural systems and circuits and their action could determine specific emotional, psychological and physiologic states. In particular: glucocorticoids, norepinephrine, gamma-amino butyric acid (GABA) and glutamate are the main players in fear reactions. They act on the amygdala and hippocampus, triggering fear–related memory and behavioral planning deficits. Moreover, reduced serotonin levels are related to unpleasant emotional states and the cocktail of low serotonin levels and testosterone excess is related to anger, aggressiveness and territorial defense behavior. Dopamine is the mediator of positive attitude: dopaminergic circuits in the limbic system are activated in case of satisfaction and they are the action site of many drugs and addictive substances.
Mind-body therapies (meditation, breathing and bioenergetics): Meditation, a complex process involving change in cognition, memory and social and emotional control, leads to improvement in various cardiovascular, neurological, autoimmune and renal pathologies.
The effects of stress are evident in each of the recognized mechanisms leading to cardiac events, including the clustering of traditional risk factors, sudden death, myocardial ischemia, plaque rupture, thrombosis and myocardial infarction as well as wall motion abnormalities, alterations in cardiac regulation as indexed by changes in sympathetic nervous system activity and homeostasis, endothelial dysfunction and malignant arrhythmias [92]. There is nonetheless overwhelming evidence both for the deleterious effects of stress on the heart and for the fact that vulnerability and resilience factors play a role in amplifying or dampening those effects. Numerous approaches are available for stress management that can decrease patient suffering and enhance their quality of life [93].
In general, studies on a range of stress reduction techniques have demonstrated significant decrease in cardiac events in patients with myocardial ischemia, stroke, atherosclerosis, hypertension and heart failure.
As we will see, the practice of meditation appears to be a fundamental method in stress management and CVD prevention. It has two advantages: it helps to purify the cognitive evaluation of all our experiences from a number of errors and distortions related to simple past conditioning; but at the same time facilitates the management of physical reactions to stress. It’s easily expected that the term "meditation" makes many people and scientists suspicious. Our western and classical medical cultures are full of prejudices and incorrect ideas about what meditation is and its real use. In the context of this review, we speak about "meditation" not aspiring to import a New Age lifestyle and impose it as a foreign body in the life of individuals; nor is equivalent to yearn civilizations and cultures distant in time and space. The term "meditation" is inflated and loaded with meanings and images, often incorrect. In this paper, "meditation" has a specific meaning: a mode of mental functioning based on the control of attention that has strong repercussions both in terms of cognitive and physiological standpoint. If we look to the East is not to emulate awkwardly folk aspects, but to learn with scientific respect their millennial experience and knowledge.
Jon Kabat-Zinn, founder and director of the Stress Reduction Clinic at the University of Massachusetts, calls "meditation", "the practice of keeping alive the attention from moment to moment" [94]. Wanting further clarity on the meaning of the term, that's what meditation is NOT [95]: it is not a mystical practice, although it has historically developed in religious contexts, mainly in the East. We must not forget that Eastern doctrines are not only a series of rites and ceremonies seemingly esoteric, but also a sophisticated and millennial mental functioning study. It is not a form of passivity or contemplative life but, on the contrary, something you can apply to the action, so much so that it was used to optimize the efficiency of samurai soldiers or rock climbers’ performance (please see http://warriorsway.com/the-rock-warriors-way-mental-training-for-climbers-2/). Although, often, the "meditation" is seen as an escape from the world. It is not another term for "relaxation". Meditation causes a feeling of well being and relaxation. But this is not its primary purpose. As it involves accepting all the moods that we live, it can also mean living feelings of anxiety and discomfort in order to change them. Meditation does not focus on content, but on the understanding of the content. It is not simply a technique that aims to enhance the attention, though its practice is focused on the use of attention and might result in a significant attentive capacity development. It is not a cognitive rebuilding technique, although its practice often allows to rethink and reformulate the meaning of situations. It's not a problem-solving technique, although it often allows to find appropriate solutions to real problems.
What then is meditation in its essence? What then remains of it, once purified of all mystical and religious aspects? It remains the fundamental teaching of not reacting to the contents of the mind as if they were reality [96]. We tend to confuse our thoughts about reality with reality itself. To use the psychological language, we tend to confuse the cognitive world with the real world.
No human being has a direct and objective perception of reality. We believe that thoughts arise in reaction to real events, but they are often linked to the latter only indirectly and in a distorted way. With the practice of meditation is possible to understand that thoughts are just thoughts, while the physical reaction is based on the belief that they are the reality with capital R. Meditating, we realize that thoughts come and go, and the problem is that often we react to them too early, emotionally and with behaviors or actions. Neutralizing the reaction, we distance ourselves from being drawn into the vortex of actions and reactions triggered mainly by "negative" thoughts. Behaviorally, when we feel bad, we tend to react distracting or looking for actions that goes to "cover" the discomfort: make a phone call, open the fridge and eat, read the paper, we immerse ourself in the social networks, turn on the television and we can go on until smoking and or alcoholism. We find hard to pay attention to what is not pleasant. We try to protect ourselves, and from moment to moment, we have to decide between the wonderful world inside our heads and the reality of the here and now, whatever it is. Cognitively negative thoughts, if not recognized consciously, trigger the production of automatic routines, judgments, emotions, physical reactions and moods that tend to feed thereself in a vicious cycle of judgment and compensation.
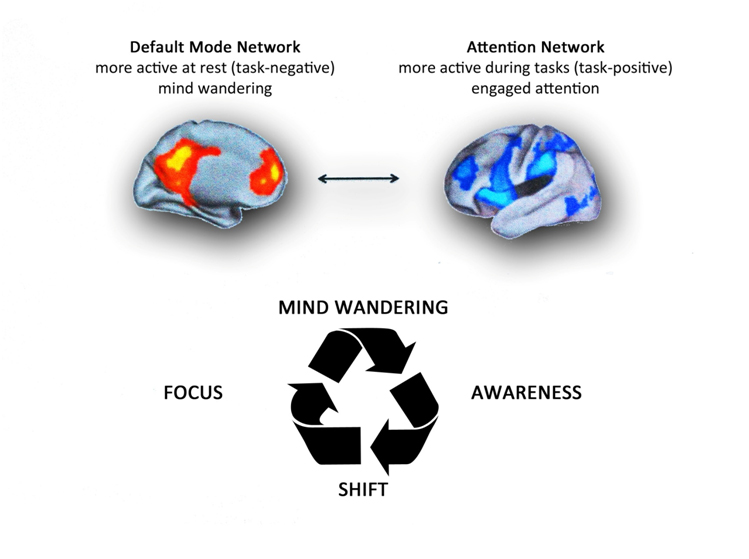
Esch describes [97]: “Meditation can be defined as willfully and purposefully regulating one’s own attention, either for the purpose of relaxation, exploring oneself or personal growth and trascedence. Mediation can operationally be divided into two categories. Either one is focusing attention on changing object such as physical sensations in the body scan, progressive muscle relaxation, autogenic training, or movements in yoga, thai chi, qigong, or mental content as in guided imagery, or mindfulness meditation proper. Or an unchanging or repetitive object is constantly held in focus, such as in mantra meditations like Transcendental Meditation ® (TM) or Benson meditation, breathing meditation like Zazen, ostinato drumming, rhythmic dancing, jogging/flow, etc. In practice both categories frequently overlap, and normally the ability to keep one’s attention focused on a steady object is the precondition for the capacity to constantly attend to moving objects. All techniques are usually conducted with an attitude of intentionally directed or focused concentration and attention, which is called “mindful awareness”. As a consequence, they have the potential to elicit the so-called “relaxation response”, whose property is responsible for some of the observed clinical, medical or therapeutic effects of meditation, particularly in stress-associated diseases, including cardiovascular, immune, proinflammatory or neuroendocrine diseases, including anxiety or depression” (Figure 2).
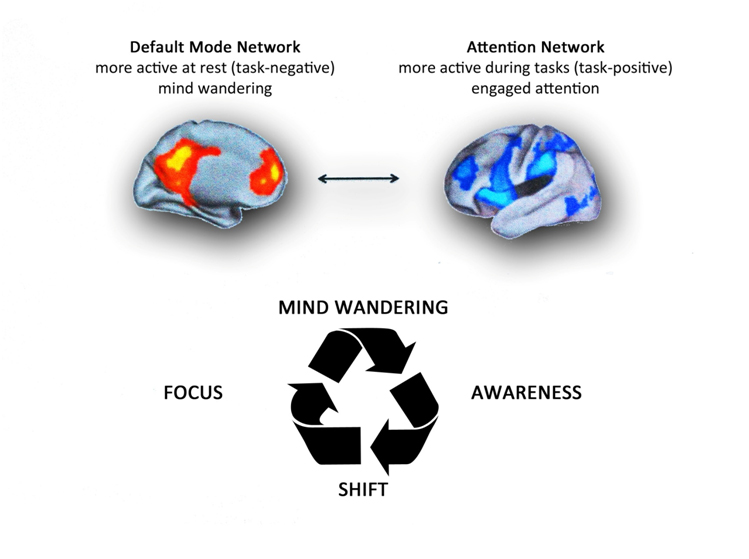
Figure 2. Top. Brain networks associated with mind wandering and attention. The brain can be divided into two-large scale distributed network: the default mode network, in which is associated mind-wandering activity, and the attention network that is associated with focused states demanding attentional resourses. Down. The process of attention during meditation. A theoretical model of dynamic cognitive states experienced by a non-expert practioner during a session of meditation. When attempting to sustain focus (FOCUS) on an object (breathing, mantra, images, etc.), an individual inevitably loses this focus and experiences wandering of attention (MIND WANDERING). At some time during mind wandering, the practitioner becomes aware that his/her mind is not on the object (AWARENESS), at which point he/she disengages from current train of thought and shifts attention back to the object (SHIFT), where it stays focused again for some period of time (FOCUS). Whith practice, the time spent during the focused and conscious thought increases. There are various methods of meditation with a common experiential goal. It 's like climbing a mountain: there are several trails, slopes, ascent velocities and path lengths, but the summit is the same. Modified from Schmidt et al. [97].
The Transcendental Meditation® (TM) program has been found to decrease coronary heart disease risk factors (hypertension, diabetes, atherosclerosis,use of cigarettes and alcohol) and associated cardiovascular morbidity and mortality [98,92,99] leading to angina symptom improvements due to the reduction of anxiety and depression-related, chronic sympathetic activation [100]. Furthermore, reduced health insurance claims were observed [92]. Moreover, an American Heart Association scientific statement provided a class of recommendation of Class IIB, Level of Evidence B for TM implementation in clinical practice, based on the available level of evidence from published literature [101]. The practice of meditation is accompanied by physiological peculiarities. We can observe a reduction in oxygen consumption, in the cardio-respiratory frequency of and blood pressure; the skin impedance increases and functional changes in brain activity happens (increasing in high-frequency, synchronized gamma waves in the electroencephalogram). It’s also possible to assess structural changes in the brain, with thickening of the areas delegated to the memory, attention, interoception, sensory processing as well as self-regulation and autoregulation [102,97]. Along with meditation practice, daytime secretion of pituitary hormones changes [103].
Mediation is associated with dopamine production regulation, and brain’s motivation and reward systems activation [97]; meditation reduces cortisol levels [104], increases peripheral melatonin levels [105], determines norepinephrine and epinephrine reduction and rise in vagal tone [106], with obvious consequences on blood pressure, heart rhythm and anxiety lowering, and with improvement in the quality of life in patients with optimally treated heart failure [107]. Serotonin and testosterone increase [108], and is possible to notice changes in growth hormone levels and thyroid stimulating hormone balance[109,110]. Acetylcholine and morphine levels augment in meditators increasing the activity of the constitutive nitric oxide-producing enzymes and determining and anti-inflammatory effect through NF-kB inhibition [97].
In summary, mediation can counteract stress at the mental [111], physical, physiological and molecular level [112], restoring and harmonizing the brain circuits [113,114], modifying the activity of the DMN [115] (Figure 2), and the neuro-immune-[116-118] endocrine [119] secretion.This particular state of consciousness induce temporal DNA transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways [120]. This counteracts mononuclear cell activation due to psychosocial stress [121,122]. Meditation has proven to be a factor that can greatly increase the positive effects of dietary control and exercise on cardiovascular health, being able to determine an initial regression of atherosclerotic disease [123,124].
The practice of meditation is often associated with breath control and breathing patterns are important for cardiovascular health [125]. Bernardi et al. studied this phenomenon showing how rhythmic formulas such as the rosary and yoga mantras can synchronize and reinforce inherent cardiovascular rhythms and modify baroreflex sensitivity improving prognosis in heart disease. Bernardi et al. demonstrated that recitation of yoga mantras and of the rosary (that was introduced in Europe after the Crusades, as a result of contact with Arabs who had been influenced by Tibetan and Indian traditions) slowed respiration to almost exactly 6/min, and enhanced heart rate variability and baroreflex sensitivity. They conclude that rosary recitation might be viewed as a religious practice as well as a health practice [125]. Greater religious fervor is not necessarily accompanied by benefits in terms of CVD and health [126], probably because of a continual sense of guilt, mortification, self-judgment etc., that constantly activate the stress axis. Moreover, the amount of carbohydrates or proteins we eat could change our breathing pattern, as commonly demonstrated by respiratory ratio variation, which is easily assessed during a standard cardiopulmonary test [127].
Some forms of meditation that aim to change individual inner dialogue, teaching emotional forgiveness to replace negative unforgiving emotions, show important health and well-being consequences [128] related to psychophysiological changes (anger or fear reaction control), and in DMN and stress axis balance.
There is a postural coding for emotions with precise muscular patterns associated with specific emotions (the so-called “Body Action Coding System”) [129]. Briefly,on the one hand, specific muscles are activated to express certain emotions, on the other, it was also found that the same muscles automatically responded to the perception of emotion, without any overt movement [130], and this could be part of a reflex starting from our mirror neurons [131]. In this way, our feelings draw in the body a rest or “usual” body posture through the repetition of expressed or perceived emotions. Many Yoga [132,133-152], Thai Chi, Pilates or rock climbing practices act in this scenario, combining breathing exercises, meditation and movement, releasing muscular tensions within particular body areas, with benefits in physical and mental health [139,153-157]. At cardiovascular level, the practice of yoga has proven useful in the control of arrhythmias [158].
As in the case of nutrition and exercise, the practice of meditation is accompanied with an improvement in endothelial function [142,159-163].
Recent studies revealed that massage therapy [164-166] attenuates production of inflammatory cytokines [167] and stress hormones [168-172], reducing endothelial dysfunction [173] and promoting angiogenesis [174,175].
An interesting perspective on the field of mind-body therapies concerns biofield. The National Institutes of Health (NIH) National Center for Complementary and Alternative Medicine (NCCAM) describes biofield therapies as ‘‘intended to affect energy fields that purportedly surround and penetrate the human body” [176]. Biofield therapies seek to work with the human body’s putative vital energy field, which has been described across cultures as chi, qi, ki, and prana, such that changes in the field interact with and lead to changes in physiology as well as mood [176]. This theory has its roots in traditional medical practices such as Ayurveda and Chinese Medicine.
While known physiological mechanisms appear to contribute to the beneficial effects of physical touch, a barrier to the acceptance of biofield therapies is the lack of a proven biological mechanism to explain non-contact healing [177]. Electromagnetic energy represents nowadays the bridge between atomic and cellular levels, and currently its therapeutic applications in oncology are under investigation [178]. Given the electrical charge inherent in all the molecules and atoms that make up our body, it is clear that every human being produces a magnetic field. We measure it continually in our clinical practice through electrocardiograms or magnetic resonances.
According to some scientists, the electromagnetic energy performs the function of a kind of mold that give shape to the physical body [179]. In the '40s, Harold S. Burr,a Professor of Anatomy at the Yale University School of Medicine, studied the shape of the magnetic fields (which he called "vital fields” or “energy fields") surrounding the plants and animals. He described quite surprising phenomena. According to Burr’s studies, the electric field of a bud or a salamander embryo does not reflect the original seed or embryo shapes, but rather resembles the adult plant or animal [179]. The same would occur in the human body. We know that if you spread iron filings on a piece of paper hanging above a magnet, iron filings spread according to the "lines of force" of the magnetic field of the magnet. If this filing is thrown away and we throw a new, this also take the same form. The molecules and cells that make up the human body seem to behave in a similar manner and their turnover would follow the lines of force of the individual electromagnetic field [179]. It would seem that a vibrational field precedes the appearance of dense matter and is not merely a reflection of the same. Burr provided evidence for this belief both with sophisticated electrical measurements, and also demonstrating the extraordinarily significant hypothesis that the appearance of physical illness (cancer, in his studies) occurs after a measurable change in the organism's electric field [179]. These findings have not been confirmed by other works; however, with the technology available today, it could be possible to design new studies aimed at confirming what was reported by Burr.
We have already seen that in quantum physics, the same DNA molecule oscillates and produces a small magnetic field that can be interested by outside influences [180]. Further studies are needed to determine what happens in the case of using biofield therapies [181]; studies that are likely to affect and be addressed to thinner layers of matter. Interestingly, even in order to see the activity of thought as a force field that can interact with matter, it has been described a correlation between brain electrical activity between two human beings separated in space [182,183,184-186]. Creath et al. demonstrated that sound vibrations (music and noise) as well as biofields (bioelectromagnetic and healing intention [187-190]) both directly affect living biologic systems, using a seed germination bioassay to detect the effects caused by various applied energetic conditions [191]. An interesting hypothesis that could biologically explain these work could address the molecular behavior of water contained in every human cell and plant. It’s known that the magnetized water changes its hexagonal structure leading to significant biologic and therapeutic effects at the level of blood glucose, lymphocyte DNA damage, antioxidant status, and lipid profiles [192]. Water seems to change shape according to electromagnetic influences of an observer/experimenter who manifests its “positive or negative intention” [193-195]. Is possible to measure the personal electromagnetic changing according to various psychological profiles using electroencephalography [111,196,197], electrocardiography [198,199,200], functional brain MRI [201-203] or electrical cutaneous resistance [204]. The studies about the therapeutic effect of magnetized water are limited and experimentally poorly designed [192]. Thus, further scientific analysis is required to confirm these intriguing data.
Currently, it has been found some anatomical and physiological correspondences between the energy current systems described in Traditional Chinese and Ayurvedic Medicine (called meridians or srotas) [181,193-196] , that reflect precise locations where the cutaneous electrical impedance varies, as well as endocrine, nervous and immune activity [197,198]. Finally, research is under way to explain the genetic basis of pathophysiological-energetic models theorized in Chinese and Ayurvedic Medicine [205,211,212].
We would like to make a clarification on the last part of this paragraph, related to bioenergetic medicine. We know that some references cited do not belong to newspapers of “high caliber” and have some methodological limitations. However, we think that the cited studies can still represent a starting point for further research and analysis in the light of what is expressed in this manuscript. We want to point out that the description of a phenomenon must be able to stand alone. Neither the fame of a scientist nor the fancy name of a magazine are necessarily synonymous of reliability or plausibility [213-215], but the scientific method by which the data of a study are produced. The theory of relativity is not less scientific if it is announced by Micky Mouse instead of Einstein.
Music
Acoustic studies conducted in the anechoic chamber (Orfield Laboratories, please visit https://www.youtube.com/watch?v=u_DesKrHa1U; https://www.youtube.com/watch?v=mXVGIb3bzHI;https://www.youtube.com/watch?v=dtZNjzeShYw) reveal how the sound is crucial to maintain neuronal and brain balance. Through the sound seems to be possible to regain sight [216,217], through the optimization of sound frequencies we can improve neuronal performance [218]; as explained and shown in the aforementioned videos, the prolonged sitting in an anechoic environment can cause serious psychological and physical imbalances.
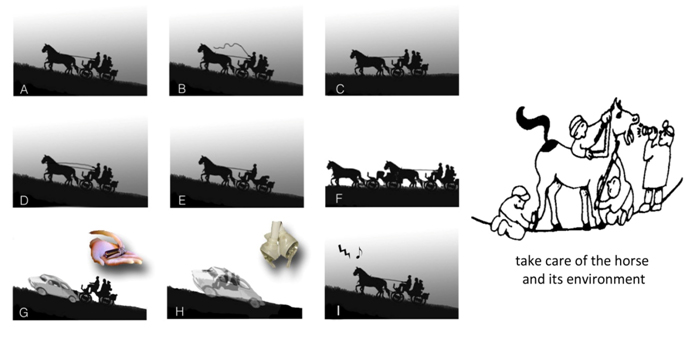
The sounds are formed by perceptible vibrations. From what has been described using the quantum physics look applied in molecular biology, if our ears were able to hear the full range of frequencies, then we could hear the music of the flowers and plants, mountains and valleys, the song of the sky and stars [219], as well as the symphony of our bodies: in absolute silence condition a man, in his being made of beats, breathing, yawning, becomes music (Figure 3 and please see https://www.youtube.com/watch?v=WhUKAx6QPP0).
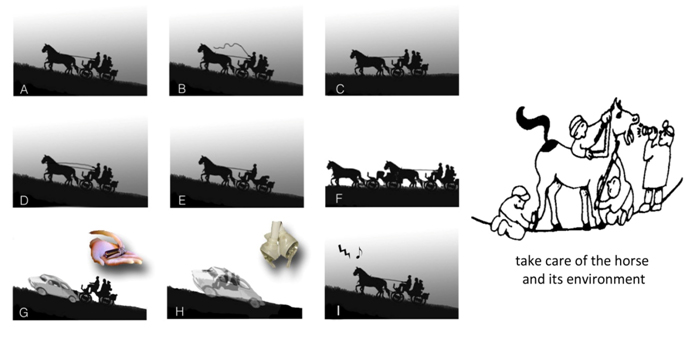
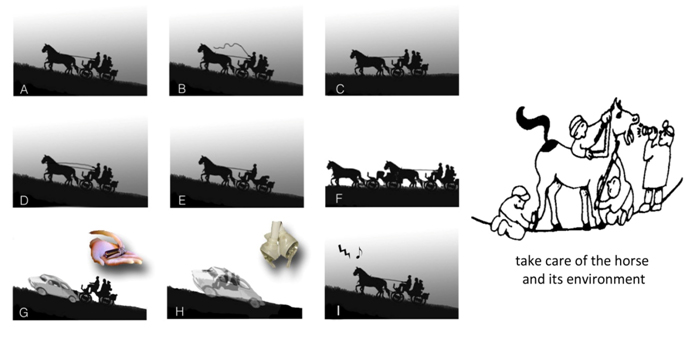
Figure 3. An example of Cardiovascular Integrative Medicine Approach. Thefigure depicts heart failure and the therapeutic options. At the left, in A is represented the problem: horses (the heart) have to carry a coach and its load (blood) along a climb (vascular resistances). A way to afford the problem is to whip horses (B) to make them do an harder work. This is the case of an acute decompensated heart, when we can use inotropic agents. Another way to solve the problem is to change the street (C): we can choose a longer way but less steep, so less work for our horses. We can reduce vascular resitances with vasodilator drugs. Another way to face the scenario is to curb horses (D): they will walk on the same climb but slower, thus with less fatigue and preserving energies. Betablockers are the agents we use for this reason. Obviously they are a mainstay for the chronic therapy of heart failure and are contraindicated in the acute setting. Another solution is to reduce the load of the coach (E). This is the role of diuretics and ultrafiltration. Nowadays, we can mechanically assist the heart function, in a partial way, with ventricular assistance devices (VAD) or with total artificial heart (G and H respectively). Moreover, as in the example I we can resynchronize the marching step (i.e., cardiac contraction) through a cardiac resynchronization therapy or CRT. Heart transplantation (F) remains the treatment of choice for many patients with end-stage HF with severely impaired functional capacity despite optimal medical therapy.
Next to all these solutions, we can integrate another one: we can take care of the horse before getting sick, keeping it healthy. If the horse becomes ill, we can associate to all pharmacological and surgical remedies a meticulous care of food, herbal medicine, adequate physical activity, a particular attention to emotions and to psychosocial stress, as well as methods of relaxation, meditation and music appreciation.
Beyond this consideration, like language, music is a human universal involving perceptually discrete elements organized into hierarchically structured sequences [220].
The scientific literature produced allows to state that music appreciation represents a good stress reduction technique: music comprehension is able to improve quality of life, and shapes the DMN [221,222]. Listening to music improves sports performance, heart rate and heart rate variability [223], decreases the level of anxiety [224] in coronary artery disease patients even to a greater extent than orally administered midazolam [225] and is able to lower cortisol, adrenocorticotropic hormone, prolactin, adrenaline, noradrenaline, atrial natriuretic peptide and tissue plasminogen activator (t-PA) levels [226]. Music efficacy has been also verified in the Emergency Department in order to reduce noise stress [227].
Classical music and meditation music show the greatest benefit on health, whereas other types of sound vibrations (such as heavy metal music or techno) are not only ineffective but possibly dangerous and can lead to stress and/or life-threatening arrhythmias [228,229,230,231]. Interestingly, as revealed by Sleight et al., these effects are independent from individual music taste [232].
The positive effects of classical and meditation music are related to a lower plasmatic levels of all the hormones involved in a stress reaction [226,233-235]. Furthermore,the immune system seems to appreciate and respond to sound vibrations of classical and meditative music,up-regulating anti-inflammatory cytokines and modifying the number and characteristics of circulating B and T cells [120,236].
Finally, we have to consider that the developing field of social epigenetics is now helping us to describe how communication and emotion, prime hallmarks of music, can be linked to a transmissible, biochemical change [237]. The response of a human being to voice and music begins during fetal life, as shown by Al-Qahtani [238].
The benefits of music are accompanied by an improvement in endothelial function [239-241].
Pysical environment, society and economy
Cardiovascular morbidity and mortality are deeply influenced by the physical (for example by cold, hot, humid, sunny or windy climates [71] or by urban or rural environments [242]) and social environments. Considering the first factors, it is interesting to note the importance of the quality of the air we breathe. Indoor negatively-charged air conditions affects the human PNEI network [243] and the mere presence of fine pollution particles is associated with endothelial dysfunction [242], impacting cardiovascular health and beyond [244], related to chronic exposure to these elements. Again, these findings show that not exist, in nature, threshold values of safety, and that our body works, compensating, beyond alleged safety limits imposed by the laws relating to precise values of fine dust that "it is permitted" to circulate in the air. Another important consideration is the noise and the constant exposure to urban traffic that increase the incidence of myocardial infarction [245]. On the contrary, it has been shown to reside in a forest rule in a positive and healthy way the PNEI network (for example, reducing inflammation and oxidative stress) [246,247], so much to coin the term of “forest therapy”, with ongoing clinical trials [248-250]. Certainly, we can continue to ignore these factors. We can, for example, continue to pollute the air having faith in medicines to cure us from pollution or that genetic engineering will allow to infect us with artificial genes from whose expression we will become able to breathe polluted air . Or we will rely on the technology that will allow us to create machines able to clean up the air or make us live in futuristic diving suits able to filter it and make it healthy. But will this be “technological advancement”? Or a sad compensation?
According to the second factors, myocardial infarction ranges in case of social wild competitiveness and uncertainty [251,252], economic insecurity, social isolation and low social status [71]. In particular, among young post-myocardial infarction patients, higher levels of both cognitive and somatic depressive symptoms, especially regarding economic conditions, are associated with a higher propensity to develop myocardial ischemia with mental stress, but not with physical (exercise or pharmacological) stress [78]. Moreover, it is possible to observe higher mortality from circulatory diseases and ischemic heart disease according to unemployment condition either directly in the unemployed person [253], both in the family closer (such as the wives of the men seeking work [254]). Higher rates of myocardial infarction and stroke development have been described in married women with low social support [255].
Furthermore, cumulative exposure to psychological trauma was associated with an increased risk of recurrent cardiovascular events and mortality, independent of psychiatric comorbidities and health behaviors [256]. There’s a strict relation between outbursts of anger, dynamic that easily occurs in modern economic world, and risk of acute myocardial infarction [257,258].
Finally, high perceived stress is associated with greater risks of CVD and death for individuals with low but not high income [259] and the risk of coronary heart disease increases also among individuals reporting adverse impact of stress on their health (Whitehall II prospective cohort study, over 18 years of follow-up) [260]. Thus, international economic and health strategies should act in order to improve our surrounding environment, making it healthier.
Is 993 thousand billion dollars, the value of the global “wealth of paper " at the end of 2013, about 13 times the world gross product. Of those 993,000 billion dollars only 283,000 are primary finance, i.e., stocks, bonds and bank assets; all the rest, 710 000 billion dollars, are derivatives traded outside regulated markets, of which only a small portion is related to transactions that have to do with the real economy. (please visit: http://www.repubblica.it/economia/affari-e finanza/2014/10/27/news/finanza_un_trilione_di_dollari_che_soffoca_leconomia_reale-99097465/). This kind of economy, aimed solely at maximizing profit, undermines people's health, is not sustainable (as the global crisis has shown) and will not help to save the environment in which we live. The problem, as raised by Thomas Aquinas in his Summa Theologiae (please visit: http://www.treccani.it/enciclopedia/tommaso-d-aquino_(Il-Contributo-italiano-alla-storia-del-Pensiero:-Economia), is the “right” profit. In terms of public health this has been the subject of study by Pretty et al. who reported that increases in gross domestic product in western economic systems beyond a threshold of basic needs do not lead to further increases in well-being, demonstrating that material consumption often results in negative health externalities [261]. If environmentally sustainable consumption were increasingly substituted for material consumption, involving non-material consumption became more prevalent (healthy food, active body, healthy mind, community links, contact with nature and low attachment to possessions), then well-being would increase regardless of levels of gross domestic product [261]. It is possible to explain these considerations according to what we have seen so far about epigenetic modifications acting from the endothelial function to all the human being.
A last consideration is important in terms of public health: think of food waste. Our planet provides everything all people need: everyday a huge amount of food is thrown in the trash, as reported at the Expo 2015, currently under way. (Please visit: http://www.expo2015.org/it/rapporto-2014-sullo-spreco-alimentare--cosa-e-emerso).
The integrative medicine
The drugs and the actual western health organization aim to manage acute symptoms or to solve problems related to the “exhaustion phase”, as part of the broader reaction to stress described. This approach, however, as clearly pointed out by Marvasati et al. [262], it is not ideal in a chronic setting, and is economically unsustainable. In this view, Integrative Medicine (Figure 3) has emerged as a new therapeutic model that is patient centered, healing oriented [263]. Such patient care emphasizes the therapeutic relationship and uses therapeutic approaches originating from both conventional and alternative medicine such as meditation [142,162,265], music listening [225,239], alimentation [265,266] or physical exercises [161,267]. All these lifestyle and behavioral aspects, counteracting the stress response, have a positive effect on our health and on our cardiovascular system [268].
Integrated medicine is a humanistic and preventive medicine, that leverages the resources of the sick person, offering diagnostic and therapeutic plans that integrate modern tools of biomedicine with the ancient traditions of the East and West, providing a growing scientific verification [269]. It is a medicine "integrated" and not "alternative", because it is stupid and devoid of any foundation conceives an alternative medicine to the set of practices and knowledge emerged over the past centuries in the biomedicine field. It 's required, instead, an integration of those knowledge that, at the end of quotation, can make a difference (as widely reported in this paper) [270,271]. “It will be possible to maximize the efficiency of health services, reduce the consumption of drugs, and increase the level of prevention and the level of citizens’ participation in the management of their health. The integration must also be a scientific integration, making everything possible to assess the degree of evidence of effectiveness existing in the various medical practices, currently defined as "unconventional". It is to return to have, between the arrows available for the doctor’s bow, some ancient therapeutic tools but scientifically valid. The healthcare provider will recover wisdom and balance, will be a lifestyle teacher, master of prevention and not a simple prescriber. He will know deeply the body language, made of hormones, neuropeptides and cytokines; will master the powerful substances derived from scientific progress in course, but will be able to get the help of herbs, natural substances, his hands, his words, music and meditation techniques. He will be again a guardian and a maintainer of life” [71]. The doctor will know how to do therapy in the etymological sense of the term. The term "therapy" comes from the greek "therapeia" which literally means "to assist someone in his path."
In this work we have often used the term endothelial “dysfunction" to conform to the scientific literature produced up to now. In fact, considering the PNEI network, epigenetics and the concept of allostatic load, we should simply use the term endothelial “regulation". Indeed, it is as if we were observing an engine that can work, for example, from 1000 rpm to 10,000 rpm. If we look it at 2000 rpm or 8000 rpm, it is not "dis-functioning", but it’s simply working at those levels. And this, as we have seen, concerns a rich network of relationships, which can be modulated to "regulate" the functioning of the biological processes observed.
Given the influence of stress on endothelial function and the ease of instrumental measurement of this parameter, it will be possible to use it as a simple tool to determine if these or further alternative techniques have a real therapeutic effect [268]. Verify the effect of a medium such as meditation, mind-body therapies or music is particularly hard. Numerous subjective bias are lurking and difficult to measure or inevitable. Moreover, different meta-analyses of high-quality studies can arrive at different conclusions based on authors’ selection of studies [272]. Randomized clinical trials (RCTs) can only be done, by definition, with patients and individuals who are willing to be randomized. Thereby such trials are excluding the potentially most beneficial therapeutic agent: conscious choice and active engagement. Thus, by default, RCTs can only test and describe what is the minimum effect on people who use a certain intervention, as if it were delivered to them as a passive recipient, like a medication. However, music listening or playing is no medication. It requires active involvement and the decision to dedicate regularly a specific amount of time, over a larger period in order to change one's habits, attitudes and physiologic responses. This can only be assessed in long-term comparative cohort studies that in other conditions and occasions have shown reliable results comparable to RCTs [273]. In order to explore correctly many faces of the so called “alternative medicines”, the scientific inputs should conform to the basic ancient principles and philosophies of the considered remedies, investigating them “as they are”: such research will require the already discussed “whole system biology and physics approaches”, global participation with protocols evolved through intense interface with modern science, and regulatory reforms to eliminate cultural and economic barriers [274]. In Table 1 are reported many evidences about the therapeutic effect of the Integrative Medicine approach in different diseases. In Table 2 are presented some epigenetic mechanisms that can control chronic inflammation linked to endothelial dysfunction. These factors are related to the disciplines involved in Integrative Medicine paradigm.
Healing a tree taking care of its fruits, its roots, the grass and the forest surrounding it

|
|
Physical and Social Environment influence morbidity and mortality
(sleep, noise, music, social relatioship and socioeconomic occupation) |
[230,235,285-302] |
|
Alimentation and physical activity |
[303,304-318] |
|
Psychotherapy, Hypnosis, Meditation, Breething |
[101,123-125,319-336] |
|
Acupuncture, Phytotherapy, Yoga, Thai-Chi |
[49 277,337-350] |
|
Pharmacologic Therapies |
[351] |
Table 1. The Integrative Medicine approach.
Factors and Techniques |
Effects |
References |
Alimentation |
|
|
1) Toxins and pesticides |
- Modify epigenome of a somatic cell;
- promote disease in the individual and in the progeny;
- modulate IL4 production, Th1/Th2 balance and IgE production.
|
[352,353-355] |
2) Ambient particulate matter exposure |
- Increased incidence of thrombotic events due to higher IL-6 production by alveolar macrophages
|
[356] |
3) Excess of iodine |
- May trigger thyroid autoimmunity
|
[357,358] |
4) Calories intake |
- Calories restriction reduces the risk for atherosclerosis in humans involving an anti-inflammatory effect (lowering PCR and TNFα levels)
- high-fat or glucose meal or smoking contributes to a postprandial inflammatory state linked to atherosclerosis progression
- high calories intake is associated with NF-kB overexpression and inflammation
|
[303,359]
|
5) L-Glutamine, L-arginine, and omega-3 polyunsaturated fatty acids (PUFAs) |
- decrease the proinflammatory prostaglandin 2 (PGE2) levels and the number of T cells; ↑omega-3 intake prolongs life and decreases NF-kB levels
|
[303 ,360-362]
|
6) Vitamins:
- B complex and C vitamins and iron;
- Vitamin A deficiency
- Vitamin D
- selenium, copper, and zinc
|
- maintains an effective Th1 cytokine-mediated immune response and avoids a shift to an anti-inflammatory Th2 cell-mediated immune response
- impairs ability to counteract extracellular pathogens;
- relates with increasing in IL-4, IL-10 and TGFβ levels and protects against multiple sclerosis and influenza;
- may reduce the risk of cardiovascular disease and enhance immune status;
- regulates of redox-sensitive transcription factors and affects production of cytokines and prostaglandins
|
[363-367]
|
7) Probiotics |
- improve the intestine's immunologic barrier, through intestinal immunoglobulin A responses;
- mediate an immune regulation, through balance control of proinflammatory and anti-inflammatory cytokines
|
[368] |
8)
- Methionine-rich diet
- Diet that leads to
increasing S-adenosyl-methionine synthesis
|
- could worsen schizophrenia;
- counteracts unipolar depression
|
[369]
|
9) Male starving some days before fecundation |
- ↓ IGF-1 and glucocorticoids in the offspring
|
[370] |
Phytherapy (examples)
- narigenin and astragaloside IV
|
- promotes macrophages, polymorphonuclear leukocytes and natural killer cells activation in upper respiratory diseases;
- inhibit the path of TLR4-NF-KB
|
[348,371]
|
Physical activity |
- increases levels of BDNF, IGF-I and other GF;
- stimulates neurogenesis;
- increases resistance to brain insult;
- improves learning and mental performance;
- induces analgesia and sedation through the endocannabinoid system’s activation;
- induces elevated levels of anti-inflammatory cytokines and suppression of proinflammatory cytokines and TNFα production;
- regular practice of Tai Chi augments resting and vaccine-stimulated levels of cell-mediated immunity to varicella zoster virus in older adults
|
[75,53 ,296,372,373] |
Society and emotions:
- anger and depression
- stressors or trauma
- chronic psychosocial stressors (job stress, low socioeconomic status, childhood adversities, life events, caregiver stress)
- paternal experience across a lifespan
|
- activates of NF-kappaB gene in mononuclear cells stimulating inflammation;
- accelerates the course of HIV disease progression altering the pituitary-adrenal hormones regulation;
- interfere with wound healing;
- high concentrations of cytokines, chemokines, and DAMPs;
- causes relaxation in infants;
- reduces allergic skin wheal responses in atopic patients;
- increases the levels of breast-milk melatonin;
- alters GF, IGF-1 and substance P levels, improves symptoms in patients with rheumatoid arthritis;
- are associated with gains in functional status after stroke
- reduces immune system activity;
- may alleviate allergic symptoms by decreasing allergen-specific IgE production, changing the Th1/Th2 balance of our immune system, increasing INFγ and IL-12 levels while decreasing IL-4 and IL-13 Th2 cytokines;
- enhance the performance of the endocrine
systems; ↑levels of breast-milk melatonin in both mothers with atopic eczema and healthy mothers.
- ↑ serum testosterone levels;↓ serum estradiol levels in patients with erectile dysfunction
- ↑catecholamines; mark epigenetically the offspring’s brain and function; ↑CRH
- ↑Th2 responses and↓ Th1 responses (reducing resistance to viral infections)
- methylation of the BDNF gene, bringing on a depressant effect; ↑CRH levels
- influences neuropsychiatric disease risk in the offspring; induces germ cell epigenetic reprogramming and impact the offspring's hypothalamic-pituitary-adrenal (HPA) stress axis regulation through specific non-coding microRNAs
|
[374,72 ,375,121,248,376,377-387]
|
Alcohol and cigarettes:
|
- increases neuroinflammation through Toll-like receptors signaling that correlates with adult neurocognitive dysfunction;
- induce TLR-4 expression and its inflammatory pathway
|
[388, 389,390]
|
Relaxation response
- meditation; music listening
|
- determines changes in cerebral cortex, prefrontal area, cingulate gyrus, neurotransmitters, white matter, autonomic nervous system, limbic system, cytokines, endorphins, hormones;
- is associated with a rapid time-dependent genomic expression changing of genes associated with energy metabolism, mitochondrial function, insulin secretion and telomere maintenance, and reduces expression of genes linked to inflammatory response
|
[119,155,302,336,337,391] |
Table 2. Epigenetic mechanisms that regulate chronic inflammation linked to endothelial dysfunction.
Conclusion: pay attention to the roots. It is really possible to heal a tree ignoring the forest surrounding it? What you sow grows, what grew was sown
We are living in a delicate moment for medicine and science in general: unsustainable costs, poor outcomes, frequent medical errors, poor patient satisfaction and worsening health disparities, all point to the need for transformation [275,276]. For more than ten years now, it is known that most of the population (2/3 of adults), also in Western countries, resort to “natural, complementary and alternative remedies” to keep their health [277].
In 2005, the United States spent an estimated 5.6% of its total health expenditures on biomedical research, more than any other country, but less than 0.1% on research in health services. From an economic perspective, biotechnology and medical device companies were most productive, as measured by new diagnostic and therapeutic devices per dollar of research and development cost. Productivity declined for new pharmaceutical drugs [278].
Furthermore a lot of drug therapy studies are built with the bias of important economic interests leading to a “selling sickness” behavior in the public and private health systems [279,280].
A recent study by Hutchins et al .[281] revealed that one in three Americans said they would prefer to risk living less long than to take a pill daily to prevent CVD. In addition, about 21% of the participants to this study, also would pay $ 1,000 or even more if this would allow to avoid the pill daily. These data show that, even ignoring entirely the aspect relating to the side effects, the simple act of having to take a pill every day can have a strong impact on the quality of life of a person and his perceived stress. Considering the fact that many adults take multiple medications every day, the effect is likely staff multiplied; at the population level, even a small reduction in quality of life such as the one highlighted in this way, multiplied by millions of people, it can have a very important effect on the cost / benefit ratio of a drug.
Is it really possible to heal a tree without curing the grass and the forest that surround it? Fruit depends on the branch, the branch on the trunk and the trunk on the roots and the soil in which they are planted [282]. What we are comes from our roots and from what we are rooted in. Choose the roots and you will decide the fruits.
What is the answer for patients asking us if it is possible in their future to discontinue beta-blocker therapy after an acute coronary syndrome or the onset of arrhythmia? They are asking about what kind of change is necessary to restore health, not just a way to get back into balance!
Sometimes, during the days I work in hospital, I am under the impression that the therapies that have been scientifically demonstrated as a valid method are somehow and sometimes like taking a yellowed apple and painting its peel red. We have to continue the therapy because we are focused on its color and on the mechanisms that regulate it, without considering the roots, the soil and the surrounding area in which the tree is planted. By changing these elements, the color of the apple will change by itself.
Let us think about what we described so far and the results of psychological and behavioral therapies, the effects of music and meditation and all the “alternative therapies“ that are emerging nowadays (the scientific evidence of their results is shown in Table 1 and 2) and that our patients often ask us about. What are we supposed to tell them? Standard of care drugs may not always protect our patients during their lives [77]! As well, some established diagnostic practices are not effective to properly stratify the risk of a patient [78], or lead to overdiagnosis and overtreatments [283].
Integrative medicine has emerged as a potential solution to the crisis in the healthcare of the US and western countries. It provides care that is patient-centered, healing-oriented, emphasizes therapeutic relationship and uses therapeutic approaches originating from conventional and alternative medicine. Initially driven by consumer demand, the attention that integrative medicine places on understanding persons as a whole and assisting with lifestyle change is now being recognized as a strategy to address the epidemic of chronic diseases bankrupting our economy. For integrative medicine to flourish in our countries, new providers, new provider models, a realignment of incentives and a commitment to health promotion and disease management will be required [270]. The contemporary doctor must take into account the physical, psychological and social environment of each patient. It is not so sure that life expectancy will continue to grow, if we continue to ignore these factors. The World Health Organization has declared, since 1946, that "health is a state of complete physical, mental and social welfare and not merely the absence of disease or infirmity", asking the governments to work responsibly, through a program of health education suitable for achieving that aim. Such concept was subsequently repeated and integrated in the Ottawa Charter of 1986 during the first International Conference on Health Promotion.
This work aims to be an opportunity to invite anyone interested in building an international task-force involving cardiologists, neurologists, immunologists, endocrinologists, psychologists and psychiatrists, sociologists, geneticists, biologists, physicists and bio-engineers to organize research on those factors that are effective in modulating the psycho-neuro-endocrine-immune network that constitutes a human being.
As sir William Osler said [284]: “the good physician treats the disease; the great physician treats the patient who has the disease. Medicine is the science of uncertainty and the art of probability. One of the first duties of the physician is to educate the masses not to take medicine. It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has. The value of experience is not in seeing much, but in observing wisely. He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all. Observe, record, tabulate and communicate. Use the five senses. Learn to see, learn to feel, learn to smell, and know that only through practice you become expert. Acquire the art of detachment, the virtue of the method, the accuracy and quality, but above all the grace of humility. In truth, there are not specializations in medicine, since to fully know many of the most important diseases you must be familiar with their manifestations in many organs. The desire to take medicine is perhaps what most distinguishes human beings from animals. Patients need rest, food, fresh air and exercise - the so called “quadrangle of health”. The young doctor starts with 20 medications for each disease, the old one ends up with a single medicine for 20 diseases. The more one is ignorant, the more it is dogmatic”.
References
- Fioranelli M (2014) Journal of Integrative Cardiology. J Integr Cardiol 1: 1.
- Dal Lin C, Tona F, Osto E (2015) Coronary Microvascular Function and Beyond: The Crosstalk between Hormones, Cytokines, and Neurotransmitters. Int J Endocrinol.
- Ziv Y, Schwartz M (2008) Immune-based regulation of adult neurogenesis: implications for learning and memory. Brain Behav Immun 22: 167-176. [Crossref]
- Ma T, Tan C, Zhang H, Wang M, Ding W, et al. (2010) Bridging the gap between traditional Chinese medicine and systems biology: the connection of Cold Syndrome and NEI network. Mol Biosyst 6: 613-619. [Crossref]
- WangD, Lu C-Y, Teng L-S, Guo Z-H, Meng Q-F, et al. (2014) Therapeutic effects of Chinese herbal medicine against neuroendocrinological diseases especially related to hypothalamus-pituitary-adrenal and hypothalamus-pituitary-gonadal axis. Pak J Pharm Sci 27: 741–754. [Crossref]
- Dias P, Joshi M. (2012) Endothelial dysfunction as a risk factor for cardiovascular disease; its modulation by phyto-ingredients and implication in better cardiovascular health. Oxid Antioxid Med Sci 1: 1.
- Brown AA, Hu FB (2001) Dietary modulation of endothelial function: implications for cardiovascular disease. Am J Clin Nutr 73: 673-686. [Crossref]
- Stein PK, Soare A, Meyer TE, Cangemi R, Holloszy JO, et al. (2012) Caloric restriction may reverse age-related autonomic decline in humans. Aging Cell 11: 644-650. [Crossref]
- Dai J, Lampert R, Wilson PW, Goldberg J, Ziegler TR, et al. (2010) Mediterranean dietary pattern is associated with improved cardiac autonomic function among middle-aged men: a twin study. Circ Cardiovasc Qual Outcomes 3: 366-373. [Crossref]
- Grassi G, Dell'Oro R, Facchini A, Quarti Trevano F, Bolla GB, et al. (2004) Effect of central and peripheral body fat distribution on sympathetic and baroreflex function in obese normotensives. J Hypertens 22: 2363-2369. [Crossref]
- Gentile CL, Orr JS, Davy BM, Davy KP (2007) Modest weight gain is associated with sympathetic neural activation in nonobese humans. Am J Physiol Regul Integr Comp Physiol 292: R1834-1838. [Crossref]
- Lips MA, de Groot GH, De Kam M, Berends FJ, Wiezer R, et al. (2013) Autonomic nervous system activity in diabetic and healthy obese female subjects and the effect of distinct weight loss strategies. Eur J Endocrinol 169: 383-390. [Crossref]
- Sullivan EL, Riper KM, Lockard R, Valleau JC (2015) Maternal high-fat diet programming of the neuroendocrine system and behavior. Horm Behav. [Crossref]
- Salas-Salvado J, Bullo M, Estruch R, Ros E, Covas MI, et al. (2014) Original Research Prevention of Diabetes With Mediterranean Diets. Ann Intern Med 160: 1–11 [Crossref]
- Koloverou E, Esposito K, Giugliano D, Panagiotakos D (2014) The effect of Mediterranean diet on the development of type 2 diabetes mellitus: a meta-analysis of 10 prospective studies and 136,846 participants. Metabolism 63: 903-911. [Crossref]
- Poutahidis T, Kleinewietfeld M, Smillie C, Levkovich T, Perrotta A, et al. (2013) Microbial reprogramming inhibits Western diet-associated obesity. PLoS One 8: e68596. [Crossref]
- Gostner JM, Becker K, Ueberall F, Fuchs D (2015) The good and bad of antioxidant foods: An immunological perspective. Food Chem Toxicol 80: 72-79. [Crossref]
- Becker K, Schroecksnadel S2, Gostner J, Zaknun C2, Schennach H3, et al. (2014) Comparison of in vitro tests for antioxidant and immunomodulatory capacities of compounds. Phytomedicine 21: 164-171. [Crossref]
- Huang EY, Devkota S, Moscoso D, Chang EB, Leone VA (2013) The role of diet in triggering human inflammatory disorders in the modern age. Microbes Infect 15: 765-774. [Crossref]
- Thorburn AN, Macia L, Mackay CR (2014) Diet, metabolites, and "western-lifestyle" inflammatory diseases. Immunity 40: 833-842. [Crossref]
- Manzel A, Muller DN, Hafler DA, Erdman SE, Linker RA, et al. (2014) Role of "Western diet" in inflammatory autoimmune diseases. Curr Allergy Asthma Rep 14: 404. [Crossref]
- Vieira SM, Pagovich OE, Kriegel MA (2014) Diet, microbiota and autoimmune diseases. Lupus 23: 518-526. [Crossref]
- Berer K, Mues M, Koutrolos M, Rasbi ZA, Boziki M, et al. (2011) Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 479: 538-541. [Crossref]
- Maslowski KM, Mackay CR (2011) Diet, gut microbiota and immune responses. Nat Immunol 12: 5-9. [Crossref]
- Belkaid Y, Hand TW (2014) Role of the microbiota in immunity and inflammation. Cell 157: 121-141. [Crossref]
- Salas-Salvadó J, Garcia-Arellano a, Estruch R, Marquez-Sandoval F, Corella D, et al. (2008) Components of the Mediterranean-type food pattern and serum inflammatory markers among patients at high risk for cardiovascular disease. Eur J Clin Nutr 62: 651–659. [Crossref]
- MenaM-P, Sacanella E, Vazquez-Agell M, Morales M, Fitó M, et al. (2009) Inhibition of circulating immune cell activation: a molecular antiinflammatory effect of the Mediterranean diet. Am J Clin Nutr 89: 248–256. [Crossref]
- Ramon Estruch, Emilio Ros, Jordi Salas-Salvad, Maria-Isabel Covas, Dolores Coreila, et al. (2013) Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N Engl J Med 368: 1279. [Crossref]
- Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, et al. (2004) Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 292: 1440-1446. [Crossref]
- Woo KS, Kwok TC, Celermajer DS (2014) Vegan diet, subnormal vitamin B-12 status and cardiovascular health. Nutrients 6: 3259-3273. [Crossref]
- Sanders TA (2014) Plant compared with marine n-3 fatty acid effects on cardiovascular risk factors and outcomes: what is the verdict? Am J Clin Nutr 100 Suppl 1: 453S-8S. [Crossref]
- Shridhar K, Dhillon PK, Bowen L, Kinra S, Bharathi AV, et al. (2014) The association between a vegetarian diet and cardiovascular disease (CVD) risk factors in India: the Indian Migration Study. PLoS One 9: e110586. [Crossref]
- Shridhar K, Dhillon PK, Bowen L, Kinra S, Bharathi AV, et al. (2014) Nutritional profile of Indian vegetarian diets--the Indian Migration Study (IMS). Nutr J 13: 55. [Crossref]
- Singh PN, Arthur KN, Orlich MJ, James W, Purty A, et al. (2014) Global epidemiology of obesity, vegetarian dietary patterns, and noncommunicable disease in Asian Indians. Am J Clin Nutr 100 Suppl 1: 359S-364S. [Crossref]
- Dominique Ashen M (2013) Vegetarian diets in cardiovascular prevention. Curr Treat Options Cardiovasc Med 15: 735-745. [Crossref]
- Yokoyama Y, Nishimura K, Barnard ND, Takegami M, Watanabe M, et al. (2014) Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med 174: 577-587. [Crossref]
- Kwok CS, Umar S, Myint PK, Mamas MA, Loke YK (2014) Vegetarian diet, Seventh Day Adventists and risk of cardiovascular mortality: a systematic review and meta-analysis. Int J Cardiol 176: 680-686. [Crossref]
- Martínez-González M, Sánchez-Tainta A, Corella D, Salas-Salvadó J, Ros E, et al. (2014) A provegetarian food pattern and reduction in total mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am J Clin Nutr 100: 320–329. [Crossref]
- Brown K, DeCoffe D, Molcan E, Gibson DL (2012) Diet-induced dysbiosis of the intestinal microbiota and the effects on immunity and disease. Nutrients 4: 1095-1119. [Crossref]
- Mangge H, Becker K, Fuchs D, Gostner JM (2014) Antioxidants, inflammation and cardiovascular disease. World J Cardiol 6: 462-477. [Crossref]
- Soory M (2012) Nutritional antioxidants and their applications in cardiometabolic diseases. Infect Disord Drug Targets 12: 388-401. [Crossref]
- EstruchR, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al. (2013) Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368: 1279–1290. [Crossref]
- ZazpeI, Sanchez-Tainta A, Estruch R, Lamuela-Raventos RM, Schröder H, Salas-Salvado J, et al. (2008) A Large Randomized Individual and Group Intervention Conducted by Registered Dietitians Increased Adherence to Mediterranean-Type Diets: The PREDIMED Study. J Am Diet Assoc 108: 1134–1144. [Crossref]
- Salas-Salvadó J, Fernández-Ballart J, Ros E, Martínez-González MA, Fitó M, et al. (2008) Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: one-year results of the PREDIMED randomized trial. Arch Intern Med 168: 2449-2458. [Crossref]
- Agnoli C, Krogh V, Grioni S, Sieri S, Palli D, et al. (2011) A priori-defined dietary patterns are associated with reduced risk of stroke in a large Italian cohort. J Nutr 141: 1552-1558. [Crossref]
- Schwingshackl L, Hoffmann G (2014) Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis 24: 929-939. [Crossref]
- Zhao QT, Li BF, Kong H (2014) Roles of Chinese medicine bioactive ingredients in the regulation of cellular function of endothelial progenitor cells. Chin J Nat Med 12: 481-487. [Crossref]
- Aggarwal BB, Ichikawa H, Garodia P, Weerasinghe P, Sethi G, et al. (2006) From traditional Ayurvedic medicine to modern medicine: identification of therapeutic targets for suppression of inflammation and cancer. Expert Opin Ther Targets 10: 87–118. [Crossref]
- FabioFirenzuoli. Fitoterapia. Guida all’uso clinico delle piante medicinali. 4th ed. Milano: Elsevier, 2009: 231-268.
- Camm AJ, Luscher TF, Serruys PW (2009) ESC Textbook of Cardiovascular Medicine Second Edition. Oxford Med: 1-1398.
- Hu G, Tuomilehto J, Silventoinen K, Barengo NC, Peltonen M, et al. (2005) The effects of physical activity and body mass index on cardiovascular, cancer and all-cause mortality among 47 212 middle-aged Finnish men and women. Int J Obes (Lond) 29: 894-902. [Crossref]
- Myers J, Kaykha A, George S, Abella J, Zaheer N, et al. (2004) Fitness versus physical activity patterns in predicting mortality in men. Am J Med 117: 912-918. [Crossref]
- Cotman CW, Berchtold NC (2002) Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci 25: 295-301. [Crossref]
- Teri L, Gibbons LE, McCurry SM, Logsdon RG, Buchner DM, et al. (2003) Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 290: 2015-2022. [Crossref]
- Mattson MP (2012) Energy intake and exercise as determinants of brain health and vulnerability to injury and disease. Cell Metab 16: 706-722. [Crossref]
- Walsh NP, Gleeson M, Pyne DB, Nieman DC, Dhabhar FS, et al. (2011) Position statement. Part two: Maintaining immune health. Exerc Immunol Rev 17: 64-103. [Crossref]
- Nieman DC, Luo B, Dréau D, Henson DA, Shanely RA, et al. (2014) Immune and inflammation responses to a 3-day period of intensified running versus cycling. Brain Behav Immun 39: 180-185. [Crossref]
- Nieman DC (1994) Exercise, infection, and immunity. Int J Sports Med 15: S131-141. [Crossref]
- Nieman DC (2008) Regular moderate exercise boosts immunity. Agro Food Ind Hi Tech 19: 8–10.
- Nieman DC (2000) Is infection risk linked to exercise workload? Med Sci Sports Exerc 32: S406-411. [Crossref]
- Nieman DC (2011) Moderate Exercise Improves Immunity and Decreases Illness Rates. Am J Lifestyle Med 5: 338–345.
- Pedersen BK, Nieman DC (1998) Exercise immunology: Integration and regulation. Immunol Today 19: 204–206. [Crossref]
- Luo B, Xiang D2, Nieman DC3, Chen P4 (2014) The effects of moderate exercise on chronic stress-induced intestinal barrier dysfunction and antimicrobial defense. Brain Behav Immun 39: 99-106. [Crossref]
- Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, et al. (2011) Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc 43: 1334–1359.
- Bottaccioli F. Il sistema immunitario: la bilancia della vita. 2nd ed. Milano: Tec. Nuove, 2008: 1-428.
- Petersen AM, Pedersen BK (2006) The role of IL-6 in mediating the anti-inflammatory effects of exercise. J Physiol Pharmacol 57 Suppl 10: 43-51. [Crossref]
- Bergh C, Udumyan R, Fall K, Almroth H, Montgomery S (2015) Stress resilience and physical fitness in adolescence and risk of coronary heart disease in middle age. Heart 101: 623-629. [Crossref]
- Mehler MF (2008) Epigenetic principles and mechanisms underlying nervous system functions in health and disease. Prog Neurobiol 86: 305–341. [Crossref]
- Berdasco M, Esteller M (2013) Genetic syndromes caused by mutations in epigenetic genes. Hum Genet 132: 359-383. [Crossref]
- Wang X, Gulbahce N, Yu H (2011) Network-based methods for human disease gene prediction. Brief Funct Genomics 10: 280-293. [Crossref]
- Bottaccioli F (2005) Psiconeuroendocrinoimmunologia. I fondamenti scientifici delle relazioni mente-corpo. Le basi razionali della medicina integrata Red! Il Castello Group 1-507.
- Rodgers AB, Morgan CP, Bronson SL, Revello S, Bale TL (2013) Paternal stress exposure alters sperm microRNA content and reprograms offspring HPA stress axis regulation. J Neurosci 33: 9003–9012. [Crossref]
- Miranda JJ, Gilman RH, Smeeth L (2011) Differences in cardiovascular risk factors in rural, urban and rural-to-urban migrants in Peru. Heart 97: 787-796. [Crossref]
- Liem SS, Oemrawsingh PV, Cannegieter SC, Le Cessie S, Schreur J, et al. (2009) Cardiovascular risk in young apparently healthy descendents from Asian Indian migrants in the Netherlands: the SHIVA study. Neth Heart J 17: 155-161. [Crossref]
- Nakajima K, Takeoka M, Mori M, Hashimoto S, Sakurai A,et al.(2010) Exercise effects on methylation of ASC gene. Int J Sports Med 31: 671–675. [Crossref]
- Blumenthal JA, Jiang W, Babyak MA, Krantz DS, Frid DJ, et al. (1997) Stress management and exercise training in cardiac patients with myocardial ischemia. Effects on prognosis and evaluation of mechanisms. Arch Intern Med 157: 2213-2223. [Crossref]
- Bairey CN, Krantz DS, DeQuattro V, Berman DS, Rozanski A (1991) Effect of beta-blockade on low heart rate-related ischemia during mental stress. J Am Coll Cardiol 17: 1388-1395. [Crossref]
- Wei J, Pimple P, Shah AJ2, Rooks C, Bremner JD3, et al. (2014) Depressive symptoms are associated with mental stress-induced myocardial ischemia after acute myocardial infarction. PLoS One 9: e102986. [Crossref]
- Rozanski A, Blumenthal JA, Kaplan J (1999) Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 99: 2192-2217. [Crossref]
- Balestri M, Calati R, Serretti A, De Ronchi D (2014) Genetic modulation of personality traits: a systematic review of the literature. Int Clin Psychopharmacol 29: 1-15. [Crossref]
- Rademaker AR, Kleber RJ, Geuze E, Vermetten E (2009) Personality dimensions harm avoidance and self-directedness predict the cortisol awakening response in military men. Biol Psychol 81: 177-183. [Crossref]
- Dimopoulou C, Ising M, Pfister H, Schopohl J, Stalla GK, et al. (2013) Increased prevalence of anxiety-associated personality traits in patients with Cushing’s disease: a cross-sectional study. Neuroendocrinology 97: 139–145. [Crossref]
- Yoda N, Yamashita T, Wada Y, Fukui M, Hasegawa G, et al. (2008) Classification of adult patients with type 2 diabetes using the Temperament and Character Inventory. Psychiatry Clin Neurosci 62: 279-285. [Crossref]
- Joyce PR, Mulder RT, Cloninger CR (1994) Temperament and hypercortisolemia in depression. Am J Psychiatry 151: 195-198. [Crossref]
- Wang S, Mason J, Charney D, Yehuda R, Riney S, et al. (1997) Relationships between hormonal profile and novelty seeking in combat-related posttraumatic stress disorder. Biol Psychiatry 41: 145–151. [Crossref]
- Simic I, Adzic M, Maric N, Savic D, Djordjevic J, et al. (2013) A preliminary evaluation of leukocyte phospho-glucocorticoid receptor as a potential biomarker of depressogenic vulnerability in healthy adults. Psychiatry Res 209: 658–664. [Crossref]
- Capitanio JP, Abel K, Mendoza SP, Blozis SA, McChesney MB, et al. (2008) Personality and serotonin transporter genotype interact with social context to affect immunity and viral set-point in simian immunodeficiency virus disease. Brain Behav Immun 22: 676–689. [Crossref]
- Carnevali L, Sgoifo A (2014) Vagal modulation of resting heart rate in rats: the role of stress, psychosocial factors, and physical exercise. Front Physiol 5: 118. [Crossref]
- Ader R (2011) Psychoneuroimmunology, Two-Volume Set. Elsevier: 1-1269
- Mittleman MA, Maclure M, Sherwood JB, Mulry RP, Tofler GH, et al. (1995) Triggering of acute myocardial infarction onset by episodes of anger. Determinants of Myocardial Infarction Onset Study Investigators. Circulation 92: 1720–1725. [Crossref]
- Luciano S. Psicofisiologia (2009) Dalla genetica comportamentale alle attività cognitive. Zanichelli: 1-224.
- Walton KG, Schneider RH, Nidich S (2004) Review of controlled research on the transcendental meditation program and cardiovascular disease. Risk factors, morbidity, and mortality. Cardiol Rev 12: 262-266. [Crossref]
- Dimsdale JE (2008) Psychological stress and cardiovascular disease. J Am Coll Cardiol 51: 1237–1246. [Crossref]
- Kabat-Zinn J (2005) Bringing mindfulness to medicine: an interview with Jon Kabat-Zinn, PhD. Interview by Karolyn Gazella. Adv Mind Body Med 21: 22-27. [Crossref]
- Paulson S, Davidson R, Jha A, Kabat-Zinn J (2013) Becoming conscious: the science of mindfulness. Ann N Y Acad Sci 1303: 87-104. [Crossref]
- Ludwig DS, Kabat-Zinn J (2008) Mindfulness in medicine. JAMA 300: 1350-1352. [Crossref]
- Schmidt S., Meditation – Neuroscientific Approaches and Philosophical Implications. Ed. Spinger, 2014.
- Schneider RH, Grim CE, Rainforth M V, Kotchen T, Nidich SI, et al.(2012). Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in blacks. Circ Cardiovasc Qual Outcomes 5: 750–758. [Crossref]
- Castillo-Richmond A, Schneider RH, Alexander CN, Cook R, Myers H, et al. (2000) Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke 31: 568-573. [Crossref]
- Cunningham C, Brown S, Kaski JC (2000) Effects of transcendental meditation on symptoms and electrocardiographic changes in patients with cardiac syndrome X. Am J Cardiol 85: 653-655. [Crossref]
- Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, et al. (2013) Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association. Hypertension 61: 1360–1383.
- Wallace RK (1970) Physiological effe2021 Copyright OAT. All rights reservp; Science 167: 1751-1754. [Crossref]
- Infante JR, Peran F, Martinez M, Roldan A, Poyatos R, et al. (1998) ACTH and beta-endorphin in transcendental meditation. Physiol Behav 64: 311-315. [Crossref]
- Carlson LE, Speca M, Patel KD, Goodey E (2004) Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology 29: 448–474. [Crossref]
- Nagendra RP, Maruthai N, Kutty BM (2012) Meditation and its regulatory role on sleep. Front Neurol 3: 54. [Crossref]
- Emani S, Binkley PF (2010) Mind-body medicine in chronic heart failure: a translational science challenge. Circ Heart Fail 3: 715-725. [Crossref]
- Curiati JA, Bocchi E, Freire JO, Arantes AC, Braga M, et al. (2005) Meditation reduces sympathetic activation and improves the quality of life in elderly patients with optimally treated heart failure: a prospective randomized study. J Altern Complement Med 11: 465–472. [Crossref]
- Walton KG, Schneider RH, Nidich SI, Salerno JW, Nordstrom CK, et al. (2002) Psychosocial stress and cardiovascular disease Part 2: effectiveness of the Transcendental Meditation program in treatment and prevention. Behav Med 28: 106-123. [Crossref]
- MacLean CR, Walton KG, Wenneberg SR, Levitsky DK, Mandarino JP, et al. (1997) Effects of the Transcendental Meditation program on adaptive mechanisms: changes in hormone levels and responses to stress after 4 months of practice. Psychoneuroendocrinology 22: 277–295. [Crossref]
- Stigsby B, Rodenberg JC, Moth HB (1981) Electroencephalographic findings during mantra meditation (transcendental meditation). A controlled, quantitative study of experienced meditators. Electroencephalogr Clin Neurophysiol 51: 434–442. [Crossref]
- Gaylord C, Orme-Johnson D, Travis F (1989) The effects of the transcendental mediation technique and progressive muscle relaxation on EEG coherence, stress reactivity, and mental health in black adults. Int J Neurosci 46: 77-86. [Crossref]
- Jevning R, Wallace RK, Beidebach M (1992) The physiology of meditation: a review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev 16: 415-424. [Crossref]
- Campanella F, Crescentini C, Urgesi C, Fabbro F (2014) Mindfulness-oriented meditation improves self-related character scales in healthy individuals. Compr Psychiatry 55: 1269-1278. [Crossref]
- Butler LD, Waelde LC, Hastings TA, Chen XH, Symons B, et al. (2008) Meditation with yoga, group therapy with hypnosis, and psychoeducation for long-term depressed mood: a randomized pilot trial. J Clin Psychol 64: 806-820. [Crossref]
- Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, et al. (2011) Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci U S A 108: 20254-20259. [Crossref]
- Niles H, Mehta DH, Corrigan AA, Bhasin MK, Denninger JW (2014) Functional genomics in the study of mind-body therapies. Ochsner J 14: 681-695. [Crossref]
- Reig-Ferrer A, Ferrer-Cascales R, Santos-Ruiz A, Campos-Ferrer A, Prieto-Seva A, et al. (2014) A relaxation technique enhances psychological well-being and immune parameters in elderly people from a nursing home: a randomized controlled study. BMC Complement Altern Med 14: 311. [Crossref]
- Kox M, van Eijk LT, Zwaag J, van den Wildenberg J, Sweep FC, et al. (2014) Voluntary activation of the sympathetic nervous system and attenuation of the innate immune response in humans. Proc Natl Acad Sci U S A 111: 7379-7384. [Crossref]
- Jindal V, Gupta S, Das R (2013) Molecular mechanisms of meditation. Mol. Neurobiol 48: 808–811. [Crossref]
- Bhasin MK, Dusek JA, Chang BH, Joseph MG, Denninger JW, et al. (2013) Relaxation Response Induces Temporal Transcriptome Changes in Energy Metabolism, Insulin Secretion and Inflammatory Pathways. PLoS One 8.
- Bierhaus A, Wolf J, Andrassy M, Rohleder N, Humpert PM, et al. (2003) A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci U S A 100: 1920-1925. [Crossref]
- Dusek JA, Otu HH, Wohlhueter AL, Bhasin M, Zerbini LF, et al. (2008) Genomic counter-stress changes induced by the relaxation response. PLoS One 3: e2576. [Crossref]
- Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, et al. (1990) Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet 336: 129-133. [Crossref]
- Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, et al. (1998) Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280: 2001-2007. [Crossref]
- Bernardi L, Sleight P, Bandinelli G, Cencetti S, Fattorini L, et al. (2001) Effect of rosary prayer and yoga mantras on autonomic cardiovascular rhythms: comparative study. BMJ 323: 1446-1449. [Crossref]
- Matthew Feinstein, Kiang Liu, PhD, Hongyan Ning, MD MS, George Fitchett, PhD, and Donald M. Lloyd-Jones MS (2011) Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: the multi-ethnic study of atherosclerosis (MESA). Circulation 121: 659–666. [Crossref]
- Wasserman K, Mcilroy Mb (1964) Detecting the threshold of anaerobic metabolism in cardiac patients during exercise. Am J Cardiol 14: 844-852. [Crossref]
- Worthington EL, Witvliet CVO, Pietrini P, Miller AJ (2007) Forgiveness, health, and well-being: a review of evidence for emotional versus decisional forgiveness, dispositional forgivingness, and reduced unforgiveness. J Behav Med 30:291–302. [Crossref]
- Huis In 't Veld EM, Van Boxtel GJ, de Gelder B (2014) The Body Action Coding System I: muscle activations during the perception and expression of emotion. Soc Neurosci 9: 249-264. [Crossref]
- Huis In 't Veld EM, van Boxtel GJ, de Gelder B (2014) The Body Action Coding System II: muscle activations during the perception and expression of emotion. Front Behav Neurosci 8: 330. [Crossref]
- Brass M, Muhle-Karbe PS1 (2014) More than associations: an ideomotor perspective on mirror neurons. Behav Brain Sci 37: 195-196. [Crossref]
- Mason H, Vandoni M, Debarbieri G, Codrons E, Ugargol V, et al. (2013) Cardiovascular and respiratory effect of yogic slow breathing in the yoga beginner: what is the best approach? Evid Based Complement Alternat Med: 743504. [Crossref]
- Madanmohan, Udupa K, Bhavanani AB, Shatapathy CC, Sahai A (2004) Modulation of cardiovascular response to exercise by yoga training. Indian J Physiol Pharmacol 48: 461-465. [Crossref]
- Bhavanani AB (2012) Bridging yoga therapy and personal practice: the power of sadhana. Int J Yoga Therap: 89-90. [Crossref]
- Kay A (2007) Yoga and Meditation: An Adjunct to Nutrition Counseling in Weight Management: Program Rationale and Design. J Am Diet Assoc 107:A98.
- Yeung A, Kiat H, Denniss AR, Cheema BS, Bensoussan A, et al. (2014) Randomised controlled trial of a 12 week yoga intervention on negative affective states, cardiovascular and cognitive function in post-cardiac rehabilitation patients. BMC Complement Altern Med 14: 411. [Crossref]
- Thomas J, Jamieson G, Cohen M (2014) Low and then high frequency oscillations of distinct right cortical networks are progressively enhanced by medium and long term Satyananda Yoga meditation practice. Front Hum Neurosci 8: 197. [Crossref]
- Manocha R, Marks GB, Kenchington P, Peters D, Salome CM (2002) Sahaja yoga in the management of moderate to severe asthma: a randomised controlled trial. Thorax 57: 110-115. [Crossref]
- Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, et al. (2004) Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med 10: 261-8. [Crossref]
- Saatcioglu F (2013) Regulation of gene expression by yoga, meditation and related practices: a review of recent studies. Asian J Psychiatr 6: 74-77. [Crossref]
- Madanmohan, Bhavanani AB, Dayanidy G, Sanjay Z, Basavaraddi IV (2012) Effect of yoga therapy on reaction time, biochemical parameters and wellness score of peri and post-menopausal diabetic patients. Int J Yoga 5: 10-15. [Crossref]
- Sivasankaran S, Pollard-Quintner S, Sachdeva R, Pugeda J, Hoq SM, et al. (2006) The effect of a six-week program of yoga and meditation on brachial artery reactivity: do psychosocial interventions affect vascular tone? Clin Cardiol 29: 393-398. [Crossref]
- Bhavanani AB, Ramanathan M, Balaji R, Pushpa D (2014) Comparative immediate effect of different yoga asanas on heart rate and blood pressure in healthy young volunteers. Int J Yoga 7: 89-95. [Crossref]
- Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, et al. (2000) Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord 57: 255-259. [Crossref]
- Bhavanani AB, Udupa K, Madanmohan, Ravindra P (2011) A comparative study of slow and fast suryanamaskar on physiological function. Int J Yoga 4: 71-76.
- Dinesh T, Gaur G, Sharma V, Madanmohan T, Harichandra Kumar K, et al. (2015) Comparative effect of 12 weeks of slow and fast pranayama training on pulmonary function in young, healthy volunteers: A randomized controlled trial. Int J Yoga 8: 22–26. [Crossref]
- Bhavanani AB, Madanmohan, Sanjay Z (2012) Immediate effect of chandra nadi pranayama (left unilateral forced nostril breathing) on cardiovascular parameters in hypertensive patients. Int J Yoga 5: 108–111. [Crossref]
- Sharma VK, Trakroo M, Subramaniam V, Rajajeyakumar M, Bhavanani AB, et al. (2013) Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int J Yoga 6: 104-110. [Crossref]
- Bhavanani AB, Sanjay Z, Madanmohan (2011) Immediate effect of sukha pranayama on cardiovascular variables in patients of hypertension. Int J Yoga Therap: 73-76. [Crossref]
- Trakroo M, Bhavanani AB, Pal GK, Udupa K, Krishnamurthy N (2013) A comparative study of the effects of asan, pranayama and asan-pranayama training on neurological and neuromuscular functions of Pondicherry police trainees. Int J Yoga 6: 96-103. [Crossref]
- Bhavanani AB, Ramanathan M, Balaji R, Pushpa D (2013) Immediate effects of Suryanamaskar on reaction time and heart rate in female volunteers. Indian J Physiol Pharmacol 57: 199-204. [Crossref]
- Bhavanani AB, Madanmohan, Sanjay Z, Basavaraddi IV (2012) Immediate cardiovascular effects of pranava pranayama in hypertensive patients. Indian J Physiol Pharmacol 56: 273-278. [Crossref]
- Gallagher B. Tai Chi Chuan, Qigong (2003) Top Geriatr Rehabil 19: 172–82.
- Martins-Meneses DT, Antunes HKM, de Oliveira NRC, Medeiros A (2015) Mat Pilates training reduced clinical and ambulatory blood pressure in hypertensive women using antihypertensive medications. Int J Cardiol 179: 262–8. [Crossref]
- Jago R, Jonker ML, Missaghian M, Baranowski T (2006) Effect of 4 weeks of Pilates on the body composition of young girls. Prev Med 42: 177-180. [Crossref]
- Guimarães GV, Carvalho VO, Bocchi EA, d'Avila VM (2012) Pilates in heart failure patients: a randomized controlled pilot trial. Cardiovasc Ther 30: 351-356. [Crossref]
- Williams ES, Taggart P, Carruthers M (1978) Rock climbing: observations on heart rate and plasma catecholamine concentrations and the influence of oxprenolol. Br J Sports Med 12: 125-128. [Crossref]
- Gunda S, Kanmanthareddy A, Atkins D, Bommana S, Pimentel R, et al. (2015) Role of yoga as an adjunctive therapy in patients with neurocardiogenic syncope: a pilot study. J Interv Card Electrophysiol 43: 105-110. [Crossref]
- Prakhinkit S, Suppapitiporn S, Tanaka H, Suksom D (2014) Effects of Buddhism walking meditation on depression, functional fitness, and endothelium-dependent vasodilation in depressed elderly. J Altern Complement Med 20: 411–416. [Crossref]
- Vaccarino V, Kondwani KA, Kelley ME, Murrah NV, Boyd L, et al. (2013) Effect of meditation on endothelial function in Black Americans with metabolic syndrome: a randomized trial. Psychosom Med 75: 591-599. [Crossref]
- Cheng TO (2007) Effect of Tai Chi on endothelial function. Clin Cardiol 30: 150. [Crossref]
- Paul-Labrador M, Polk D, Dwyer JH, Velasquez I, Nidich S, et al. (2006) Effects of a randomized controlled trial of transcendental meditation on components of the metabolic syndrome in subjects with coronary heart disease. Arch Intern Med 166: 1218-1224. [Crossref]
- Shiina Y, Funabashi N, Lee K, Toyoda T, Sekine T, et al. (2008) Relaxation effects of lavender aromatherapy improve coronary flow velocity reserve in healthy men evaluated by transthoracic Doppler echocardiography. Int J Cardiol 129: 193–197. [Crossref]
- Basler AJ (2011) Pilot study investigating the effects of Ayurvedic Abhyanga massage on subjective stress experience. J Altern Complement Med 17: 435-440. [Crossref]
- Dhuri KD, Bodhe PV, Vaidya AB (2013) Shirodhara: A psycho-physiological profile in healthy volunteers. J Ayurveda Integr Med 4: 40-44. [Crossref]
- Anderson PG, Cutshall SM (2007) Massage therapy: a comfort intervention for cardiac surgery patients. Clin Nurse Spec 21: 161-165. [Crossref]
- von Andrian UH (1997) A massage for the journey: keeping leukocytes soft and silent. Proc Natl Acad Sci U S A 94: 4825-4827. [Crossref]
- Baldini S, Restani L, Baroncelli L, Coltelli M, Franco R, et al. (2013) Enriched early life experiences reduce adult anxiety-like behavior in rats: a role for insulin-like growth factor 1. J Neurosci 33: 11715–11723. [Crossref]
- Guzzetta A, Baldini S, Bancale A, Baroncelli L, Ciucci F, et al. (2009) Massage accelerates brain development and the maturation of visual function. J Neurosci 29: 6042-6051. [Crossref]
- Guzzetta A, D'Acunto MG, Carotenuto M, Berardi N, Bancale A, et al. (2011) The effects of preterm infant massage on brain electrical activity. Dev Med Child Neurol 53 Suppl 4: 46-51. [Crossref]
- Field T (2014) Massage therapy research review. Complement Ther Clin Pract 20: 224-229. [Crossref]
- Field T, Diego M, Hernandez-Reif M (2010) Moderate pressure is essential for massage therapy effects. Int J Neurosci 120: 381-385. [Crossref]
- Franklin NC, Ali MM, Robinson AT, Norkeviciute E, Phillips SA (2014) Massage therapy restores peripheral vascular function after exertion. Arch Phys Med Rehabil 95: 1127-1134. [Crossref]
- Best TM, Gharaibeh B, Huard J (2013) Stem cells, angiogenesis and muscle healing: a potential role in massage therapies? Postgrad Med J 89: 666-670. [Crossref]
- Andrzejewski W, Kassolik K, Dziegiel P, Pula B, Ratajczak-Wielgomas K, et al. (2014) Effects of synergistic massage and physical exercise on the expression of angiogenic markers in rat tendons. Biomed Res Int 2014: 878095. [Crossref]
- Mills PJ, Jain S (2010) Biofield therapies and psychoneuroimmunology. Brain Behav Immun 24: 1229-1230. [Crossref]
- Baldwin AL, Hammerschlag R (2014) Biofield-based therapies: a systematic review of physiological effects on practitioners during healing. Explore (NY) 10: 150-161. [Crossref]
- Tofani S (2015) Electromagnetic energy as a bridge between atomic and cellular levels in the genetics approach to cancer treatment. Curr Top Med Chem 15: 572-578. [Crossref]
- Matthews RE (2007) Harold Burr's biofields measuring the electromagnetics of life. Subtle Energies & Energy Medicine Journal Archives 18: 55-61.
- Montagnier L, Aissa J, Del Giudice E, Lavallee C, Tedeschi A, et al. (2010) DNA waves and water. J Phys Conf Ser 306: 1–10.
- Rosch PJ (2009) Bioelectromagnetic and subtle energy medicine: the interface between mind and matter. Ann N Y Acad Sci 1172: 297-311. [Crossref]
- Muehsam D, Ventura C (2014) Life rhythm as a symphony of oscillatory patterns: electromagnetic energy and sound vibration modulates gene expression for biological signaling and healing. Glob Adv Health Med 3: 40–55. [Crossref]
- Thaheld FH (2005) An interdisciplinary approach to certain fundamental issues in the fields of physics and biology: towards a unified theory. Biosystems 80: 41-56. [Crossref]
- Thaheld F (2003) Biological nonlocality and the mind-brain interaction problem: comments on a new empirical approach. Biosystems 70: 35-41. [Crossref]
- Thaheld FH (2004) A method to explore the possibility of nonlocal correlations between brain electrical activities of two spatially separated animal subjects. Biosystems 73: 205–216. [Crossref]
- Thaheld F (2004) Comments on the paper ‘Correlations between brain electrical activities of two spatially separated human subjects’, by J. Wackermann, C. Seiter, H. Keibel, H. Walach, Neurosci. Lett., 336 (2003) 60-64. Neurosci Lett 360: 178–179.
- Radin D, Yount G (2004) Effects of healing intention on cultured cells and truly random events. J Altern Complement Med 10: 103-112. [Crossref]
- Radin D, Stone J, Levine E, Eskandarnejad S, Schlitz M, et al. (2008) Compassionate Intention As a Therapeutic Intervention by Partners of Cancer Patients: Effects of Distant Intention on the Patients’ Autonomic Nervous System. Explor J Sci Heal 4: 235–243. [Crossref]
- Schlitz M, Radin D, Malle BF, Schmidt S, Utts J, et al. (2003) Distant healing intention: Definitions and evolving guidelines for laboratory studies. Altern Ther Health Med 9: A31-A43. [Crossref]
- Schlitz M, Hopf HW, Eskenazi L, Vieten C, Radin D (2012) Distant healing of surgical wounds: an exploratory study. Explore (NY) 8: 223-230. [Crossref]
- Creath K, Schwartz GE (2004) Measuring effects of music, noise, and healing energy using a seed germination bioassay. J Altern Complement Med 10: 113-122. [Crossref]
- Lee HJ, Kang MH (2013) Effect of the magnetized water supplementation on blood glucose, lymphocyte DNA damage, antioxidant status, and lipid profiles in STZ-induced rats. Nutr Res Pract 7: 34-42. [Crossref]
- Emoto M (2004) Healing with water. J Altern Complement Med 10: 19-21. [Crossref]
- Radin D, Hayssen G, Emoto M, Kizu T (2006) Double-blind test of the effects of distant intention on water crystal formation. Explore (NY) 2: 408-411. [Crossref]
- Radin D, Lund N, Emoto M, Kizu T, Sciences N, et al. (2008) Effects of Distant Intention on Water Crystal Formation? A Triple-Blind Replication. J Sci Explor 22: 481–493.
- Chiesa A, Serretti A (2010) A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med 40: 1239-1252. [Crossref]
- Sokhadze EM (2007) Effects of music on the recovery of autonomic and electrocortical activity after stress induced by aversive visual stimuli. Appl Psychophysiol Biofeedback 32: 31–50. [Crossref]
- Kop WJ, Krantz DS, Nearing BD, Gottdiener JS, Quigley JF.et al(2004) Effects of acute mental stress and exercise on T-wave alternans in patients with implantable cardioverter defibrillators and controls. Circulation 109: 1864–1869. [Crossref]
- Lampert R, Shusterman V, Burg M, McPherson C, Batsford W, et al. (2009) Anger-induced T-wave alternans predicts future ventricular arrhythmias in patients with implantable cardioverter-defibrillators. J Am Coll Cardiol 53: 774–778. [Crossref]
- Taggart P, Sutton P, Redfern C, Batchvarov VN, Hnatkova K, et al. (2005) The effect of mental stress on the non-dipolar components of the T wave: modulation by hypnosis. Psychosom Med 67: 376-383. [Crossref]
- Yan C, Liu D, He Y, Zou Q, Zhu C, et al. (2009) Spontaneous brain activity in the default mode network is sensitive to different resting-state conditions with limited cognitive load. PLoS One 4: e5743. [Crossref]
- Mars RB, Neubert FX, Noonan MP, Sallet J, Toni I, et al. (2012) On the relationship between the "default mode network" and the "social brain". Front Hum Neurosci 6: 189. [Crossref]
- Jang JH, Jung WH, Kang DH, Byun MS, Kwon SJ, et al. (2011) Increased default mode network connectivity associated with meditation. Neurosci Lett 487: 358-362. [Crossref]
- Puissant C, Abraham P, Durand S, Humeau-Heurtier A, Faure S, et al. (2014) Assessment of endothelial function by acetylcholine iontophoresis: impact of inter-electrode distance and electrical cutaneous resistance. Microvasc Res 93: 114–118. [Crossref]
- Hankey A (2005) A test of the systems analysis underlying the scientific theory of Ayurveda's Tridosha. J Altern Complement Med 11: 385-390. [Crossref]
- Hankey A (2010) Establishing the Scientific Validity of Tridosha part 1: Doshas, Subdoshas and Dosha Prakritis. Anc Sci Life 29: 6-18. [Crossref]
- Lakhotia SC (2014) Translating Ayurveda's Dosha-Prakriti into objective parameters. J Ayurveda Integr Med 5: 176. [Crossref]
- Patwardhan B (2014) Bridging Ayurveda with evidence-based scientific approaches in medicine. EPMA J 5: 19. [Crossref]
- Omura Y (1987) Meridian-like networks of internal organs, corresponding to traditional Chinese 12 main meridians and their acupuncture points as detected by the ‘Bi-Digital O-Ring Test imaging method’: search for the corresponding internal organ of Western medicine for. Acupunct Electrother Res 12: 53–70. [Crossref]
- Omura Y (1989) Connections found between each meridian (heart, stomach, triple burner, etc.) & organ representation area of corresponding internal organs in each side of the cerebral cortex; release of common neurotransmitters and hormones unique to each meridian and co. Acupunct Electrother Res 14: 155–186.
- Pal M (1991) The tridosha theory. Anc Sci Life 10: 144-155. [Crossref]
- Shilpa S, Murthy CG (2011) Development and standardization of Mysore Tridosha scale. Ayu 32: 308-314. [Crossref]
- Gollogly L, Momen H (2006) Ethical dilemmas in scientific publication: pitfalls and solutions for editors. Rev Saude Publica 40 Spec no. [Crossref]
- Seife C (2015) Research misconduct identified by the US Food and Drug Administration: out of sight, out of mind, out of the peer-reviewed literature. JAMA Intern Med 175: 567-577. [Crossref]
- Seife C (2012) Is drug research trustworthy? The pharmaceutical industry funnels money to prominent scientists who are doing research that affects its products--and nobody can stop it. Sci Am 307: 56-63. [Crossref]
- Striem-Amit E, Cohen L, Dehaene S, Amedi A (2012) Reading with sounds: sensory substitution selectively activates the visual word form area in the blind. Neuron 76: 640-652. [Crossref]
- Striem-Amit E, Dakwar O, Reich L, Amedi A (2012) The large-scale organization of "visual" streams emerges without visual experience. Cereb Cortex 22: 1698-1709. [Crossref]
- Ronsse LM, Wang LM (2013) Relationships between unoccupied classroom acoustical conditions and elementary student achievement measured in eastern Nebraska. J Acoust Soc Am 133: 1480–1495. [Crossref]
- Adak A, Robinson AP, Singh PK, Chatterjee G, Lad AD, et al. (2015) Terahertz acoustics in hot dense laser plasmas. Phys Rev Lett 114: 115001. [Crossref]
- Patel AD (2003) Language, music, syntax and the brain. Nat Neurosci 6: 674-681. [Crossref]
- Kay BP, Meng X, Difrancesco MW, Holland SK, Szaflarski JP (2012) Moderating effects of music on resting state networks. Brain Res 1447: 53-64. [Crossref]
- Blood AJ, Zatorre RJ, Bermudez P, Evans AC (1999) Emotional responses to pleasant and unpleasant music correlate with activity in paralimbic brain regions. Nat Neurosci 2: 382-387. [Crossref]
- Szmedra L, Bacharach DW (1998) Effect of music on perceived exertion, plasma lactate, norepinephrine and cardiovascular hemodynamics during treadmill running. Int J Sports Med 19: 32-37. [Crossref]
- Koelsch Sand Jancke L, Music and the heart. Eur Heart J. [Crossref]
- Bradt J, Dileo C, Potvin N (2013) Music for stress and anxiety reduction in coronary heart disease patients. Cochrane database Syst Rev 12: CD006577. [Crossref]
- Mockel M, Rocker L, Storks T, Vollert J, Danne O, et al. (1994) Immediate physiological responses of healthy volunteers to different types of music: cardiovascular, hormonal and mental changes. Eur J Appl Physiol Occup Physiol 69: 274. [Crossref]
- Short AE, Ahern N, Holdgate A, Morris J, Sidhu B (2010) Using Music to Reduce Noise Stress for Patients in the Emergency Department: A Pilot Study. Music Med 2: 201–207.
- Bernardi L, Porta C, Sleight P (2006) Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music in musicians and non-musicians: the importance of silence. Heart 92: 445-452. [Crossref]
- Bernardi L, Porta C, Casucci G, Balsamo R, Bernardi NF, et al. (2009) Dynamic interactions between musical, cardiovascular, and cerebral rhythms in humans. Circulation 119: 3171-3180. [Crossref]
- Trappe HJ (2010) The effects of music on the cardiovascular system and cardiovascular health. Heart 96: 1868-1871. [Crossref]
- Hatem TP, Lira PI, Mattos SS (2006) The therapeutic effects of music in children following cardiac surgery. J Pediatr (Rio J) 82: 186-192. [Crossref]
- Sleight P (2013) Cardiovascular effects of music by entraining cardiovascular autonomic rhythms music therapy update: tailored to each person, or does one size fit all? Neth Heart J 21: 99-100. [Crossref]
- Khalfa S, Bella SD, Roy M, Peretz I, Lupien SJ (2003) Effects of relaxing music on salivary cortisol level after psychological stress. Ann N Y Acad Sci 999: 374-376. [Crossref]
- White JM1 (1999) Effects of relaxing music on cardiac autonomic balance and anxiety after acute myocardial infarction. Am J Crit Care 8: 220-230. [Crossref]
- Trappe HJ1 (2012) Role of music in intensive care medicine. Int J Crit Illn Inj Sci 2: 27-31. [Crossref]
- Uchiyama M, Jin X, Zhang Q, Hirai T, Amano A, et al. (2012) Auditory stimulation of opera music induced prolongation of murine cardiac allograft survival and maintained generation of regulatory CD4+CD25+ cells. J Cardiothorac Surg 7: 26. [Crossref]
- Brigati C, Saccuman MC, Banelli B, Di Vinci A, Casciano I, et al. (2012) Toward an epigenetic view of our musical mind. Front Genet 2: 111. [Crossref]
- Al-Qahtani NH1 (2005) Foetal response to music and voice. Aust N Z J Obstet Gynaecol 45: 414-417. [Crossref]
- Miller M, Mangano CC, Beach V, Kop WJ, Vogel RA (2010) Divergent effects of joyful and anxiety-provoking music on endothelial vasoreactivity. Psychosom Med 72: 354-356. [Crossref]
- Bittman B, Croft DT Jr, Brinker J, van Laar R, Vernalis MN, et al. (2013) Recreational Music-Making alters gene expression pathways in patients with coronary heart disease. Med Sci Monit 19: 139-147. [Crossref]
- Bittman B, Berk L, Shannon M, Sharaf M, Westengard J, et al. (2005) Recreational music-making modulates the human stress response: a preliminary individualized gene expression strategy. Med Sci Monit 11: BR31-40. [Crossref]
- LeBlanc AJ, Cumpston JL, Chen BT, Frazer D, Castranova V, et al. (2009) Nanoparticle inhalation impairs endothelium-dependent vasodilation in subepicardial arterioles. J Toxicol Environ HealthA 72: 1576–1584. [Crossref]
- Takahashi K, Otsuki T, Mase A, Kawado T, Kotani M, et al. (2008) Negatively-charged air conditions and responses of the human psycho-neuro-endocrino-immune network. Environ Int 34: 765-772. [Crossref]
- Yi TC, Li JP (2014) [Adverse effects of ultrafine particles on the cardiovascular system and its mechanisms]. Beijing Da Xue Xue Bao 46: 996-1000. [Crossref]
- Peters A, von Klot S, Heier M, Trentinaglia I, Hörmann A, et al. (2004) Exposure to traffic and the onset of myocardial infarction. N Engl J Med 351: 1721-1730. [Crossref]
- Li Q, Kawada T (2011) Effect of forest therapy on the human psycho-neuro-endocrino-immune network. Nihon Eiseigaku Zasshi 66: 645-650. [Crossref]
- Lee J, Park BJ, Tsunetsugu Y, Kagawa T, Miyazaki Y (2011) Physiological benefits of forest environment: based on field research at 4 sites. Nihon Eiseigaku Zasshi 66: 663-669. [Crossref]
- Park BJ, Tsunetsugu Y, Morikawa T, Kagawa T, Lee J, et al. (2014) Physiological and psychological effects of walking in stay-in forest therapy. Nihon Eiseigaku Zasshi 69: 98-103. [Crossref]
- Ikei H, Song C, Kagawa T, Miyazaki Y (2014) Physiological and psychological effects of viewing forest landscapes in a seated position in one-day forest therapy experimental model. Nihon Eiseigaku Zasshi 69: 104–10. [Crossref]
- Li Q, Kawada T (2014) Possibility of clinical applications of forest medicine. Nihon Eiseigaku Zasshi 69: 117-121. [Crossref]
- Men T, Brennan P, Boffetta P, Zaridze D (2003) Russian mortality trends for 1991-2001: analysis by cause and region. BMJ 327: 964. [Crossref]
- Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, et al. (2009) Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: an update. Eur J Cardiovasc Prev Rehabil 16: 333-350. [Crossref]
- Moser KA, Fox AJ, Jones DR (1984) Unemployment and mortality in the OPCS Longitudinal Study. Lancet 2: 1324-1329. [Crossref]
- Moser KA, Fox AJ, Goldblatt PO, Jones DR (1986) Stress and heart disease: evidence of associations between unemployment and heart disease from the OPCS Longitudinal Study. Postgrad Med J 62: 797-799. [Crossref]
- Gafarov VV, Panov DO, Gromova EA, Gagulin IV, Gafarova AV (2013) The influence of social support on risk of acute cardiovascular diseases in female population aged 25-64 in Russia. Int J Circumpolar Health 72. [Crossref]
- Hendrickson CM, Neylan TC, Na B, Regan M, Zhang Q, et al (2013) Cohen BE. Lifetime trauma exposure and prospective cardiovascular events and all-cause mortality: Findings from the Heart and Soul Study. Psychosom Med 75: 849–855. [Crossref]
- Mostofsky E, Penner EA, Mittleman MA (2014) Outbursts of anger as a trigger of acute cardiovascular events: a systematic review and meta-analysis. Eur Heart J 35: 1404–1410. [Crossref]
- Mostofsky E, Maclure M, Tofler GH, Muller JE, Mittleman MA (2013) Relation of outbursts of anger and risk of acute myocardial infarction. Am J Cardiol 112: 343-348. [Crossref]
- Redmond N, Richman J, Gamboa CM, Albert MA, Sims M,et al.(2013) Perceived stress is associated with incident coronary heart disease and all-cause mortality in low- but not high-income participants in the reasons for geographic and racial differences in stroke study. J Am Heart Assoc 2: e000447. [Crossref]
- Nabi H, Singh-Manoux A, Shipley M, Gimeno D, Marmot MG, et al. (2008) Do psychological factors affect inflammation and incident coronary heart disease: the Whitehall II Study. Arterioscler Thromb Vasc Biol 28: 1398-1406. [Crossref]
- Pretty J, Barton J, Pervez Bharucha Z, Bragg R, Pencheon D, et al. (2015) Improving health and well-being independently of GDP: dividends of greener and prosocial economies. Int J Environ Health Res. [Crossref]
- Fani Marvasti F, Stafford RS (2012) From sick care to health care--reengineering prevention into the U.S. system. N Engl J Med 367: 889-891. [Crossref]
- Bell IR, Caspi O, Schwartz GE, Grant KL, Gaudet TW, et al. (2002) Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Arch Intern Med 162: 133-140. [Crossref]
- Koike MK, Cardoso R (2014) Meditation can produce beneficial effects to prevent cardiovascular disease. Horm Mol Biol Clin Investig 18: 137-143. [Crossref]
- Carluccio MA, Massaro M, Bonfrate C, Siculella L, Maffia M, et al. (1999) Oleic acid inhibits endothelial activation?: A direct vascular antiatherogenic mechanism of a nutritional component in the mediterranean diet. Arterioscler Thromb Vasc Biol 19: 220–228. [Crossref]
- Christon RA (2003) Mechanisms of action of dietary fatty acids in regulating the activation of vascular endothelial cells during atherogenesis. Nutr Rev 61: 272-279. [Crossref]
- Nader T, Rothenberg S, Averbach R, Charles B, Fields JZ, et al. (2000) Improvements in chronic diseases with a comprehensive natural medicine approach: a review and case series. Behav Med 26: 34-46. [Crossref]
- Shiina Y, Funabashi N, Lee K, Toyoda T, Sekine T, Honjo S, et al. (2008) Relaxation effects of lavender aromatherapy improve coronary flow velocity reserve in healthy men evaluated by transthoracic Doppler echocardiography. Int J Cardiol 129: 193–197. [Crossref]
- Maizes V, Silverman H, Lebensohn P, Koithan M, Kligler B, et al. (2006) The integrative family medicine program: an innovation in residency education. Acad Med 81: 583-589. [Crossref]
- Maizes V, Rakel D, Niemiec C (2009) Integrative medicine and patient-centered care. Explore (NY) 5: 277-289. [Crossref]
- Bell IR, Caspi O, Schwartz GE, Grant KL, Gaudet TW, et al. (2002) Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Arch Intern Med 162: 133-140. [Crossref]
- Cramer H, Lauche R, Haller H, Dobos G, Michalsen A (2015) A systematic review of yoga for heart disease. Eur J Prev Cardiol 22: 284-295. [Crossref]
- Rutledge T, Mills P, Schneider R (2014) Meditation intervention reviews. JAMA Intern Med 174: 1193. [Crossref]
- Singh RH (2010) Exploring issues in the development of Ayurvedic research methodology. J Ayurveda Integr Med 1: 91-95. [Crossref]
- Fani Marvasti F, Stafford RS (2012) From sick care to health care--reengineering prevention into the U.S. system. N Engl J Med 367: 889-891. [Crossref]
- FrancesAJ. Antidepressant Use Has Gone Crazy: Bad News From the CDC | Psychiatric Times. Psychiatr Times October 28, 2011.
- Tuffs A (2002) Three out of four Germans have used complementary or natural remedies. BMJ 325: 990. [Crossref]
- Moses H 3rd, Dorsey ER, Matheson DH, Thier SO (2005) Financial anatomy of biomedical research. JAMA 294: 1333-1342. [Crossref]
- AngellM. The Truth About the Drug Companies. The New York Review of Books. July 15, 2004.
- RyanTJ (2005) Dr Jerome Kassirer’s Book on the take: how medicine's complicity with big business can endanger your health: worthy of comment. Circulation 111: 2552–2554.
- Hutchins R, Viera AJ, Sheridan SL, Pignone MP (2015) Quantifying the utility of taking pills for cardiovascular prevention. Circ Cardiovasc Qual Outcomes 8: 155-163. [Crossref]
- Spoladore P (205) Vita da vita. Riflessioni sul vangelo. Usiogope srl: 99.
- Bobbio M, Abrignani MG, Caldarola P, Casolo G, Fattirolli F, et al. (2014) Choosing wisely: the Top 5 list of the Italian Association of Hospital Cardiologists (ANMCO). G Ital Cardiol (Rome) 15: 244-252. [Crossref]
- Golden RL (1999) William Osler at 150: an overview of a life. JAMA 282: 2252-2258. [Crossref]
- Matsumoto Y, Mishima K, Satoh K, Tozawa T, Mishima Y, et al. (2001) Total sleep deprivation induces an acute and transient increase in NK cell activity in healthy young volunteers. Sleep 24: 804-809. [Crossref]
- Basner M, Rao H, Goel N, Dinges DF (2013) Sleep deprivation and neurobehavioral dynamics. Curr Opin Neurobiol 23: 854-863. [Crossref]
- Tijunelis MA, Fitzsullivan E, Henderson SO (2005) Noise in the ED. Am J Emerg Med 23: 332-335. [Crossref]
- Short AE, Short KT, Holdgate A, Ahern N, Morris J (2011) Noise levels in an Australian emergency department. Australas Emerg Nurs J 14: 26–31.
- Trappe H-J (2012) The Effect of Music on Human Physiology and Pathophysiology. Music Med 4: 100–5.
- Berkman LF, Syme SL (1979) Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 109: 186-204. [Crossref]
- Pinquart M, Duberstein PR (2010) Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol 75: 122-137. [Crossref]
- Berkman L. Social intergration, social networks, social support and health. In: Glass T. Social Epidemiology. New York: Oxford University Press; 2000: 137–173.
- O’Connor TG, Hetherington EM, Reiss D (1998) Family systems and adolescent development: shared and nonshared risk and protective factors in nondivorced and remarried families. Dev Psychopathol 10: 353–75. [Crossref]
- Costa G, Segnan N (1987) Unemployment and mortality. Br Med J (Clin Res Ed) 294: 1550-1551. [Crossref]
- Moser KA, Fox AJ, Jones DR (1984) Unemployment and mortality in the OPCS Longitudinal Study. Lancet 2: 1324-1329. [Crossref]
- Martikainen PT, Valkonen T (1996) Excess mortality of unemployed men and women during a period of rapidly increasing unemployment. Lancet 348: 909-912. [Crossref]
- Roelfs DJ, Shor E, Davidson KW, Schwartz JE (2011) Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med 72: 840-854. [Crossref]
- Marmot M (1999) Epidemiology of socioeconomic status and health: are determinants within countries the same as between countries? Ann N Y Acad Sci 896: 16-29. [Crossref]
- Elovainio M, Ferrie JE, Singh-Manoux A, Shipley M, Batty GD, et al. (2011) Socioeconomic differences in cardiometabolic factors: Social causation or health-related selection? Evidence from the whitehall II cohort study, 1991-2004. Am J Epidemiol 174: 779–89. [Crossref]
- Steptoe A, Shamaei-Tousi A, Gylfe A, Henderson B, Bergström S, et al. (2007) Socioeconomic status, pathogen burden and cardiovascular disease risk. Heart 93: 1567-1570. [Crossref]
- Demakakos P, Nazroo J, Breeze E, Marmot M (2008) Socioeconomic status and health: the role of subjective social status. Soc Sci Med 67: 330-340. [Crossref]
- Sapolsky RM1 (2005) The influence of social hierarchy on primate health. Science 308: 648-652. [Crossref]
- Dauncey MJ (2013) Genomic and epigenomic insights into nutrition and brain disorders. Nutrients: 887–914. [Crossref]
- Gershon MD1 (2003) Serotonin and its implication for the management of irritable bowel syndrome. Rev Gastroenterol Disord 3 Suppl 2: S25-34. [Crossref]
- Glaeser BS, Maher TJ, Wurtman RJ (1983) Changes in brain levels of acidic, basic, and neutral amino acids after consumption of single meals containing various proportions of protein. J Neurochem 41: 1016–1021. [Crossref]
- Peet M, Horrobin DF (2001) A dose-ranging study of ethyl-eicosapentonoate in treatment-unresponsive depression. J Psychopharmacol 15: 12.
- El-Osta A, Brasacchio D, Yao D, Pocai A, Jones PL, et al. (2008) Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J Exp Med 205: 2409–2417. [Crossref]
- Freeman MP, Hibbeln JR, Wisner KL, Davis JM, Mischoulon D, et al. (2006) Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry 67: 1954-1967. [Crossref]
- Freeman JM, Kossoff EH, Hartman AL (2007) The ketogenic diet: one decade later. Pediatrics 119: 535-543. [Crossref]
- Kossoff EH1 (2004) More fat and fewer seizures: dietary therapies for epilepsy. Lancet Neurol 3: 415-420. [Crossref]
- Lefevre F, Aronson N (2000) Ketogenic diet for the treatment of refractory epilepsy in children: A systematic review of efficacy. Pediatrics 105: E46. [Crossref]
- Kjeldsen-Kragh J, Haugen M, Borchgrevink CF, Laerum E, Eek M, et al. (1991) Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. Lancet 338: 899-902. [Crossref]
- Fontana L, Meyer TE, Klein S, Holloszy JO (2004) Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A 101: 6659-6663. [Crossref]
- Cotman CW, Berchtold NC (2002) Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci 25: 295-301. [Crossref]
- Martin B, Pearson M, Brenneman R, Golden E, Keselman A, et al. (2008) Conserved and differential effects of dietary energy intake on the hippocampal transcriptomes of females and males. PLoS One 3: e2398. [Crossref]
- Carro E, Nuñez A, Busiguina S, Torres-Aleman I (2000) Circulating insulin-like growth factor I mediates effects of exercise on the brain. J Neurosci 20: 2926-2933. [Crossref]
- Sparling PB, Giuffrida A, Piomelli D, Rosskopf L, Dietrich A (2003) Exercise activates the endocannabinoid system. Neuroreport 14: 2209-2211. [Crossref]
- Teri L, Gibbons LE, McCurry SM, Logsdon RG, Buchner DM, et al. (2003) Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 290: 2015-2022. [Crossref]
- Gloaguen V, Cottraux J, Cucherat M, Blackburn IM (1998) A meta-analysis of the effects of cognitive therapy in depressed patients. J Affect Disord 49: 59-72. [Crossref]
- Fava GA, Rafanelli C, Grandi S, Conti S, Belluardo P (1998) Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Arch Gen Psychiatry 55: 816-820. [Crossref]
- Littrell JL (2012) Taking the Perspective that a Depressive State Reflects Inflammation: Implications for the Use of Antidepressants. Front Psychol 3:297. [Crossref]
- Wei W, Sambamoorthi U, Olfson M, Walkup JT, Crystal S (2005) Use of psychotherapy for depression in older adults. Am J Psychiatry 162: 711-717. [Crossref]
- Quandt SA, Chen H, Grzywacz JG, Bell RA, Lang W, et al. (2005) Use of complementary and alternative medicine by persons with arthritis: results of the National Health Interview Survey. Arthritis Rheum 53: 748-755. [Crossref]
- Anbar RD (2001) Self-hypnosis for management of chronic dyspnea in pediatric patients. Pediatrics 107: E21. [Crossref]
- Anbar RD (2002) Hypnosis in pediatrics: applications at a pediatric pulmonary center. BMC Pediatr 2: 11. [Crossref]
- Anbar RD, Geisler SC (2005) Identification of children who may benefit from self-hypnosis at a pediatric pulmonary center. BMC Pediatr 5: 6. [Crossref]
- Langewitz W, Izakovic J, Wyler J, Schindler C, Kiss A, et al. (2005) Effect of self-hypnosis on hay fever symptoms - a randomised controlled intervention study. Psychother Psychosom 74: 165-172. [Crossref]
- Zachariae R, Jørgensen MM, Egekvist H, Bjerring P (2001) Skin reactions to histamine of healthy subjects after hypnotically induced emotions of sadness, anger, and happiness. Allergy 56:734–740. [Crossref]
- Kjaer TW, Bertelsen C, Piccini P, Brooks D, Alving J, et al. (2002) Increased dopamine tone during meditation-induced change of consciousness. Brain Res Cogn Brain Res 13: 255-259. [Crossref]
- Dodds SE, Herman PM, Sechrest L, Abraham I, Logue MD, et al. (2013) When a whole practice model is the intervention: Developing fidelity evaluation components using program theory-driven science for an integrative medicine primary care clinic. Evidence-based Complement Altern Med: 652047. [Crossref]
- Schneider RH, Alexander CN, Staggers F, Orme-Johnson DW, Rainforth M, et al. (2005) A randomized controlled trial of stress reduction in African Americans treated for hypertension for over one year. Am J Hypertens 18: 88-98. [Crossref]
- Fields JZ, Walton KG, Schneider RH, Nidich S, Pomerantz R, et al. (2002) Effect of a multimodality natural medicine program on carotid atherosclerosis in older subjects: A pilot trial of Maharishi Vedic Medicine. Am J Cardiol 89: 952–958. [Crossref]
- Keefer L, Blanchard EB (2002) A one year follow-up of relaxation response meditation as a treatment for irritable bowel syndrome. Behav Res Ther 40: 541-546. [Crossref]
- Yoshihara K, Hiramoto T, Sudo N, Kubo C (2011) Profile of mood states and stress-related biochemical indices in long-term yoga practitioners. Biopsychosoc Med 5: 6. [Crossref]
- Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, et al. (2007) Meditation practices for health: state of the research. Evid Rep Technol Assess (Full Rep): 1-263. [Crossref]
- Perez-De-Albeniz A, Holmes J (2000) Meditation: Concepts, effects and uses in therapy. Int J Psychother 5: 49–58.
- Watkins LR, Maier SF (2002) Beyond neurons: evidence that immune and glial cells contribute to pathological pain states. Physiol Rev 82: 981-1011. [Crossref]
- Biella G, Sotgiu ML, Pellegata G, Paulesu E, Castiglioni I, et al. (2001) Acupuncture produces central activations in pain regions. Neuroimage 14: 60-66. [Crossref]
- Shen YF, Younger J, Goddard G, Mackey S (2009) Randomized clinical trial of acupuncture for myofascial pain of the jaw muscles. J Orofac Pain 23: 353-359. [Crossref]
- Langevin HM, Churchill DL, Cipolla MJ (2001) Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB J 15: 2275-2282. [Crossref]
- Hutchinson AJ, Ball S, Andrews JC, Jones GG (2012) The effectiveness of acupuncture in treating chronic non-specific low back pain: a systematic review of the literature. J Orthop Surg Res 7: 36. [Crossref]
- Youngwanichsetha S, Phumdoung S, Ingkathawornwong T (2013) The effects of tai chi qigong exercise on plasma glucose levels and health status of postpartum Thai women with type 2 diabetes. Focus Altern Complement Ther 18: 182–7.
- Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, et al. (2004) Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med 117: 541-548. [Crossref]
- Yeh GY, Roberts DH, Wayne PM, Davis RB, Quilty MT, et al. (2010) Tai chi exercise for patients with chronic obstructive pulmonary disease: a pilot study. Respir Care 55: 1475-1482 [Crossref]
- Morgan N, Irwin MR, Chung M, and Wang C (2014) The effects of mind-body therapies on the immune system: meta-analysis. PLoS One 9: e100903. [Crossref]
- Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, et al. (2004) Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc 52: 892-900. [Crossref]
- Manheimer E, Cheng K, Wieland LS, Min LS, Shen X, et al. (2012) Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst Rev 5: CD005111. [Crossref]
- Barrett B (2003) Medicinal properties of Echinacea: a critical review. Phytomedicine 10: 66-86. [Crossref]
- Pittler MH, Ernst E (2003) Kava extract for treating anxiety. Cochrane Database Syst Rev : CD003383. [Crossref]
- Craig WJ (2009) Health effects of vegan diets. Am J Clin Nutr 89: 1627S-1633S. [Crossref]
- Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, et al. (2015) J.Harrison's Principles of Internal Medicine 19 Ed. McGraw Hill: 1-3000.
- Skinner MK, Manikkam M, Guerrero-Bosagna C (2011) Epigenetic transgenerational actions of endocrine disruptors. Reprod. Toxicol 31: 337–343. [Crossref]
- Chalubinski M, Kowalski ML (2006) Endocrine disrupters--potential modulators of the immune system and allergic response. Allergy 61: 1326-1335. [Crossref]
- Yurino H, Ishikawa S, Sato T, Akadegawa K, Ito T, et al. (2004) Endocrine disruptors (environmental estrogens) enhance autoantibody production by B1 cells. Toxicol Sci 81: 139–47 [Crossref]
- Duramad P, Harley K, Lipsett M, Bradman A, Eskenazi B, et al. (2006) Early environmental exposures and intracellular Th1/Th2 cytokine profiles in 24-month-old children living in an agricultural area. Environ Health Perspect 114: 1916-1922. [Crossref]
- Mutlu GM, Green D, Bellmeyer A, Baker CM, Burgess Z, et al (2007)Ambient particulate matter accelerates coagulation via an IL-6-dependent pathway. J Clin Invest 117: 2952–6.1[Crossref]
- Fountoulakis S, Philippou G, Tsatsoulis A (2007) The role of iodine in the evolution of thyroid disease in Greece: from endemic goiter to thyroid autoimmunity. Hormones (Athens) 6: 25-35. [Crossref]
- Zois C, Stavrou I, Kalogera C, Svarna E, Dimoliatis I, et al. (2003) High prevalence of autoimmune thyroiditis in schoolchildren after elimination of iodine deficiency in northwestern Greece. Thyroid 13: 485-489. [Crossref]
- Fontana L, Meyer TE, Klein S, Holloszy JO (2004) Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A 101: 6659-6663. [Crossref]
- Calder PC (2006) n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am J Clin Nutr 83: 1505S-1519S. [Crossref]
- Dupertuis YM, Benais-Pont G, Buchegger F, Pichard C (2007) Effect of an immunonutrient mix on human colorectal adenocarcinoma cell growth and viability. Nutrition 23: 672-680. [Crossref]
- Berquin IM, Min Y, Wu R, Wu J, Perry D, et al. (2007) Modulation of prostate cancer genetic risk by omega-3 and omega-6 fatty acids. J Clin Invest 117: 1866-1875. [Crossref]
- Wintergerst ES, Maggini S, Hornig DH (2007) Contribution of selected vitamins and trace elements to immune function. Ann Nutr Metab 51: 301-323. [Crossref]
- Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A (2006) Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA 296: 2832-2838. [Crossref]
- Jones G, Strugnell SA, DeLuca HF (1998) Current understanding of the molecular actions of vitamin D. Physiol Rev 78: 1193-1231. [Crossref]
- Cantorna MT, Humpal-Winter J, DeLuca HF (2000) In vivo upregulation of interleukin-4 is one mechanism underlying the immunoregulatory effects of ,25-dihydroxyvitamin D(3). Arch Biochem Biophys 377: 135-138. [Crossref]
- Meydani M (2000) Effect of functional food ingredients: vitamin E modulation of cardiovascular diseases and immune status in the elderly. Am J Clin Nutr 71: 1665S-8S. [Crossref]
- Isolauri E, Sütas Y, Kankaanpää P, Arvilommi H, Salminen S (2001) Probiotics: effects on immunity. Am J Clin Nutr 73: 444S-450S. [Crossref]
- McGowan PO, Meaney MJ, Szyf M.(2008) Diet and the epigenetic (re)programming of phenotypic differences in behavior. Brain Res 1237: 12–24. [Crossref]
- Gapp K, von Ziegler L, Tweedie-Cullen RY, Mansuy IM (2014) Early life epigenetic programming and transmission of stress-induced traits in mammals: how and when can environmental factors influence traits and their transgenerational inheritance? Bioessays 36:491–502
- Yang J, Wang HX, Zhang YJ, Yang YH, Lu ML, et al. (2013) Astragaloside IV attenuates inflammatory cytokines by inhibiting TLR4/NF-kB signaling pathway in isoproterenol-induced myocardial hypertrophy. J Ethnopharmacol 150:1062–70. [Crossref]
- Petersen AM, Pedersen BK (2006) The role of IL-6 in mediating the anti-inflammatory effects of exercise. J Physiol Pharmacol 57 Suppl 10: 43-51. [Crossref]
- Irwin MR, Olmstead R, Oxman MN (2007) Augmenting immune responses to varicella zoster virus in older adults: a randomized, controlled trial of Tai Chi. J Am Geriatr Soc 55: 511-517. [Crossref]
- Meloni M. (2014) The social brain meets the reactive genome: neuroscience, epigenetics and the new social biology. Front Hum Neurosci 8: 309.
- Maslanik T, Mahaffey L, Tannura K, Beninson L, Greenwood BN, et al. (2013) The inflammasome and danger associated molecular patterns (DAMPs) are implicated in cytokine and chemokine responses following stressor exposure. Brain Behav Immun 28: 54–62. [Crossref]
- Latendresse G, Ruiz RJ (2011) Maternal Corticotropin-Releasing Hormone and the Use of Selective Serotonin Reuptake Inhibitors Independently Predict the Occurrence of Preterm Birth. J Midwifery Women’s Heal 56: 118–26. [Crossref]
- Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, et al. (1999) Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosom Med 61: 397-406. [Crossref]
- Capitanio JP, Mendoza SP, Lerche NW, Mason WA (1998) Social stress results in altered glucocorticoid regulation and shorter survival in simian acquired immune deficiency syndrome. Proc Natl Acad Sci U S A 95: 4714–4719. [Crossref]
- Kiecolt-Glaser JK, Marucha PT, Malarkey WB, Mercado AM, Glaser R (1995) Slowing of wound healing by psychological stress. Lancet 346: 1194-1196. [Crossref]
- Gouin JP, Kiecolt-Glaser JK, Malarkey WB, Glaser R (2008) The influence of anger expression on wound healing. Brain Behav Immun 22: 699-708. [Crossref]
- Kimata H (2006) Kissing selectively decreases allergen-specific IgE production in atopic patients. JPsychosom Res 60: 545-547. [Crossref]
- Kimata H (2007) Laughter elevates the levels of breast-milk melatonin. J Psychosom Res 62: 699-702. [Crossref]
- Ishigami S, Nakajima A, Tanno M, Matsuzaki T, Suzuki H, et al. (2005) Effects of mirthful laughter on growth hormone, IGF-1 and substance P in patients with rheumatoid arthritis. Clin Exp Rheumatol 23: 651-657. [Crossref]
- Ostir GV, Berges IM, Ottenbacher ME, Clow A, Ottenbacher KJ (2008) Associations between positive emotion and recovery of functional status following stroke. Psychosom Med 70: 404-409. [Crossref]
- Bartrop RW, Luckhurst E, Lazarus L, Kiloh LG, Penny R (1977) Depressed lymphocyte function after bereavement. Lancet 1: 834-836. [Crossref]
- Kimata H1 (2008) Short-term improvement of erectile dysfunction by viewing humorous films in patients with atopic dermatitis. J Sex Med 5: 2107-2110. [Crossref]
- Rosenkranz MA, Jackson DC, Dalton KM, Dolski I, Ryff CD, et al. (2003) Affective style and in vivo immune response: neurobehavioral mechanisms. Proc Natl Acad Sci U S A 100: 11148-11152. [Crossref]
- Vetreno RP, Crews FT.(2012) Adolescent binge drinking increases expression of the danger signal receptor agonist HMGB1 and Toll-like receptors in the adult prefrontal cortex. Neuroscience 226: 475–488. [Crossref]
- Yin Y, Hou G, Li E, Wang Q, Kang J. Regulation of cigarette smoke-induced toll-like receptor 4 expression by peroxisome proliferator-activated receptor-gamma agonists in bronchial epithelial cells. Respirology18 Suppl 3: 30–39. [Crossref]
- Coleman LG Jr, He J, Lee J, Styner M, Crews FT (2011) Adolescent binge drinking alters adult brain neurotransmitter gene expression, behavior, brain regional volumes, and neurochemistry in mice. Alcohol Clin Exp Res 35: 671-688. [Crossref]
- Davidson RJ, Kabat-Zinn J (2004) ‘Alterations in brain any immune function produced by mindfulness meditation: Three caveats’: Comment Response. Psychosom Med 66: 149–152. [Crossref]
- Cárdenes N, Cáceres E, Romagnoli M, Rojas M (2013) Mesenchymal stem cells: a promising therapy for the acute respiratory distress syndrome. Respiration 85: 267-278. [Crossref]
- FOCUS marzo 2015. Focus Gruner Jahr/Arnoldo Mondadori Ed 2015; 6:31.
- Nabi H, Kivimäki M, Batty GD, Shipley MJ, et al (2013) Increased risk of coronary heart disease among individuals reporting adverse impact of stress on their health: The Whitehall II prospective cohort study. Eur Heart J 34: 2697–705. [Crossref]