Abstract
Background
Proseal Laryngeal mask airway(PLMA), a modification of classical LMA, is safe and effective alternative airway device to endotracheal intubation. PLMA incorporates a drain tube ending at the tip so that there are less chances of aspiration. Use of muscle relaxant is not a must for PLMA insertion.
Methods
100 patients of ASA grade I/II divided in two groups (50 in each group). Group A received inj. midazolam 0.03mg kg-1IV and group B received inj.dexmedetomidine0.4mcg kg-1.Induction was done with inj. propofol 2.5 mg/kg IV. Ease of PLMA insertion without using muscle relaxant was studded. Time taken and number of insertion attempts, intraoperative haemodynamic parameters and complications were recorded.
Results
The resistance to mouth opening was significantly less(p=0.003) in the group B(significant resistance encountered in 2% cases) in compare togroup A (14% cases).The PLMA insertion conditions were better in group B compared to the group A (p<0.05). Time taken (11.48±3.34 sec)and number of attempts in PLMA insertion were significantly less (p<0.05) in group B when compare to group A (11.48±3.34 sec) without significant intraoperative haemodynamic changes except at 5th min post-insertion.
Conclusion
Midazolam and dexmedetomidine both are acceptable in PLMA insertion. Dexmedetomidine produces better conditions for insertion of PLMA with greater haemodynamic stability and less postoperative complications as compared to midazolam.
Keywords
proseal laryngeal mask airway, midazolam, dexmedetomidine, propofol
Introduction
The laryngeal mask airway (LMA)[1] has gained widespread popularity for airway management during surgery. Proseal Laryngeal mask airway(PLMA) is a modification of the classic laryngeal mask airway(CLMA) that incorporates a drain tube ending at the tip of the mask so that there are less chances of aspiration[2]. Use of muscle relaxant is not a must for PLMA insertion although a certain degree of jaw relaxation and depth of anaesthesia is required[3]. PLMA can be used as a safe and effective alternative airway device to endotracheal intubation [4].
Propofol is a useful agent for PLMA insertion because of its good jaw relaxation and suppression of the airway reflexes [5].
When used alone, the dose of propofol often exceeds 2.5mg/kg IV and easy insertion was seen only in about 62% of patients, and undesired side effects like drop in blood pressure, coughing, laryngospasm and body movement may occur [6]. We need an ideal agent or near ideal agent to overcome these side effects. A variety of adjuvant have been tried which can ease LMA insertion e.g. fentanyl [7], intravenous lignocaine[8], muscle relaxants [9] but none have been found to be ideal.
However, propofol is expensive so dexmedetomidine or midazolam used as anadjuvants to propofol may decrease the incidence of adverse responses to insertion of the LMA and cost. We considered that either of these drugs given before propofol may obtund airway reflexes sufficiently to allow satisfactory insertion of LMA at a lesser cost.
Midazolam and propofol both are known to act synergistically on gamma aminobutyric acid-A (GABA-A)recepters[10] and also reduces dose requirement[11].
Dexmedetomidine is a potent and highly selective α2adrenoreceptor agonist with a selectivity ratio of 1600:1(α2:α1) and its premedication dose 0.33to 0.67 mcg kg-1 IV seems to be efficaciousand can be used as premedicationin LMA insertion [12-14].
The aim of this study was to compare Propofol plus Midazolam orDexmedetomidine as an adjuvant for the ease of PLMA insertion.
Methods
After institutional ethical committee approval a prospective randomized double blinded comparative study was conducted in Dr. S.N. Medical college and attached hospitals on 100 patients of 18-60 years age, 45-80 kg weight, BMI <25 and ASA I & II status who were scheduled to undergo elective surgery. Patient having increased risk of aspiration (e.g. Gastro-oesophageal reflux disease, pregnancy), known or anticipated difficult airway, any history of reactive airway disease, surgery of the head and neck and allergy to any of the study drugs were excluded.
A detailed pre-anaesthetic check-up (PAC) including history, physical examination, detailed airway examination and routine investigations were carried out.
Patients were allocated into two groups by randomization using chit in box method. An anaesthetist who was not involved in PLMA insertion or assessment looked up the group assigned and prepared the drugs. The study groups were:
- Group A (n=50): Inj.Propofol 2.5 mg kg-1IV with Inj.Midazolam 0.03mg kg-1 IV
- Group B(n=50): Inj.Propofol 2.5 mg kg-1IV with Inj. Dexmedetomidine 0.4mcg kg-1 IV
After checking fasting status and written informed consent, an IV line secured with 18G cannula, all monitoring (ECG,pulse oximeter,Noninvasive arterial BP) attached and inj. Ringer Lactate started. Injglycopyrrolate 0.2mg IV was given 10 min before induction. The head was kept in sniffing position by using a firm 10 cm pillow. Patients were pre-oxygenated for 3 mins then given the study drug. Group A recievedInj. dexmedetomidine 0.4mcg kg-1 IV diluted in 20 ml normal saline over 5 min followed by NS 0.03ml/kgIV stat and Group B given 20 ml NS over 5 min followed by Inj.Midazolam 0.03mg kg-1IV stat. After 2 min. inj. propofol 2.5 mg/kg IV administered over 60 seconds. To reduce pain on propofol administration 1ml of 1% lidocaine was added per 100 mg of propofol. If required further rescue doses of propofol 0.5mg/kg IV were given every 30 seconds until loss of verbal response and consciousness then PLMA was inserted after 60 sec of inj. Propofol. PLMA insertion was donebyexperienced anaesthetist.The sizes of PLMA were selected according to the patient weight. The PLMA was inserted according to standard protocol using the introducer tool technique.PLMA insertion conditions were assessed using six variables on a 3 point scaleas used by Singh R, et al. [15]as follows:
- Resistance to mouth opening
- Resistance to insertion
- Swallowing
- Coughing and gagging
- Head and body movement
- Laryngospasm (defined as a partial or complete obstruction with an apparently correctly placed PLMA)
Scoring system (Table 1) is a modification of muzi’s score [16]. A score of ≤12 in total ( or ≤2 for each variable) were considered optimum for LMA insertion.
|
|
3 Point Scale
|
|
Variable
|
1
|
2
|
3
|
|
Resistance to mouth opening
|
Nil
|
Significant
|
Undue force required
|
|
Resistance to insertion
|
Nil
|
Significant
|
Undue force required
|
|
Swallowing
|
Nil
|
Significant
|
Undue force required
|
|
Coughing and gagging
|
Nil
|
Significant
|
Undue force required
|
|
Head and body movement
|
Nil
|
Significant
|
Undue force required
|
|
Laryngospasm
|
Nil
|
Significant
|
Undue force required
|
|
Total of all six variables
|
Range- min score 6 to max score 18
|
Table 1. Scoring system(muzi’s score).
The time taken for insertion was recorded from picking up the PLMA to the connection of breathing circuit. If the airway was found to be obstructed,PLMA was removed and another dose of propofol 0.5mg/kg was given, followed by another attempt of PLMA insertion 60 sec later.
A failed attempt was defined as removal of PLMA from the mouth. A maximum of two attempts were allowed and the number of attempts were recorded. After two failed attempts the study protocol was discontinued and the patient’s airway was managed according to standard protocols.
The PLMA placement was assessedby feeling the resistance at the end of device insertion, assessment of appropriate length of airway tube outside the mouth, outward movement of device on cuff inflation, neck bulge on cuff inflation, adequacy of manual ventilation, passage of gastric tube and supra-sternal notch test. No muscle relaxant is used in our study still if the patient remained apnoeic for more than 30 sec after PLMA insertion the lungs were manually ventilated until spontaneous ventilation returns.
After PLMA was successfully inserted, anaesthesiawas maintained with 1 vol%isoflurane and 60% N2O with 40% O2 and the end tidal CO2was maintained between 35-40 mmHg.
Each patient’s blood pressure and heart rate was recorded before and after giving the adjuvant drug and 1minute after induction with propofol and one minute after PLMA insertion and thereafter every minute till 5minutes post device insertion.
Any complication of device insertion like trauma to lip/tongue/oral mucosa, presence of blood on device, sore throat and difficulty on swallowing and pain on phonation after 1 hr post operatively was recorded.
Statistical analysis – Values are presented as mean (SD or range) or number (%). Hemodynamic data were analyzed using 2 tailed student's ‘t’test for intergroup comparison and paired ‘t’ test for intragroup comparison. Ordinal categorical data such as LMA insertion conditions and number of attempts were analysed with the Chi Square Test. Nominal categorical data such as gender was also analysed with the Chi Square test. A p value < 0.05 was accepted as statistically significant.The statistical analysis was done using statistical package for the social sciences (SPSS) software version 17.0.
Results
All the data is expressed as mean and standard deviation. Demographic and airway examination variables were comparable and not significant in both groups. (p>0.05)(Table 2).
|
Variable
|
Group A
(Mean ± SD)
|
Group B (Mean ± SD)
|
P Value
|
Significance
|
|
Age Distribution
|
34.56 ± 10.09
|
38.16 ± 11.41
|
0.12
|
NS
|
|
Sex Distribution
|
M-40%
F-60%
|
M-42%,
F-58%
|
0.83
|
NS
|
|
Body Mass Index (BMI)
|
21.97 ± 0.54
|
21.98 ± 0.55
|
0.98
|
NS
|
|
ASA Status
|
ASA-I 76%
ASA-II 24%
|
ASA-I 70%
ASA-II 30%
|
0.54
|
NS
|
|
Modified Mallampatti
Grading
|
I- 46%
II-50%
III-4%
|
I-48%
II-52%
III-0%
|
0.55
|
NS
|
|
Inter-incisor distance assessment
|
4.2 ± 0.63
|
4.24 ± 0.57
|
0.76
|
NS
|
|
Baseline heart rate
|
89.52 ± 16.23
|
91.86 ± 14.79
|
0.48
|
NS
|
|
Baseline mean arterial pressure
|
90.71 ± 9.57
|
88.63 ± 6.89
|
0.31
|
NS
|
Table2.Demographic data and airway assessment.
Table 3 show LMA insertion conditions. The resistance to mouth opening was significantly more in group A with significant resistance in 14% cases (p=0.003) in compare to the group B (2%) and 98% had fully relaxed jaw in group B.
|
|
Group A
|
Group B
|
P value
|
Significance
|
|
Grading
Variable
|
Nil (%)
|
Significant (%)
|
Undue force required(%)
|
Nil (%)
|
Significant(%)
|
Undue force required(%)
|
|
|
|
Resistance to mouth opening
|
86
|
14
|
0
|
98
|
2
|
0
|
0.003
|
S
|
|
Resistance to PLMA insertion
|
94
|
6
|
0
|
94
|
6
|
0
|
0.65
|
S
|
|
Swallowing grading
|
84
|
16
|
0
|
92
|
8
|
0
|
0.36
|
NS
|
|
Grading of coughing and gagging
|
70
|
30
|
0
|
88
|
12
|
0
|
0.84
|
NS
|
|
Grading of head and body movement
|
56
|
42
|
2
|
86
|
14
|
0
|
0.02
|
S
|
|
Laryngospasm grading
|
100
|
0
|
0
|
100
|
0
|
0
|
|
|
Table3.LMA insertion conditions.
The incidence of head and body movement was significantly more in group A (p=0.02). Twenty one patients (42%) in group A had significant head and body movements in compare to only 7 patients (14%) in group B.
Although the incidence of swallowing in group A (16%) was more than group B (8%) but statistically insignificant.Similarly there was no significant difference among both groups in the incidence of resistance to PLMA insertion (p=0.65), incidence of swallowing (p=0.36), coughing and gagging (p=0.84) or laryngospasm (p=NA), but the incidence of all the above parameters is less in group B.
Table 4 show mean insertion score(Muzi’s score).There were statistically significant better PLMA insertion conditions in group B compared to the group A when mean of all the six parameters(muzi’s score) were taken into consideration (p<0.05).
|
Muzi’s score
|
Group A
(Mean ± SD)
|
Group B
(Mean ± SD)
|
P value
|
Significance
|
|
Mean insertion score of 6 parameters
|
7.04 ± 1.08
|
6.38 ± 0.69
|
0.005
|
S
|
Table 4.Mean insertion score.
Table 5show ease of insertion.Time taken in PLMA insertion was significantly less (p<0.05) in group B (11.48±3.34 sec)when compare to group A (11.48±3.34 sec). Number of attempts to insert PLMA in group B were significantly less than groupA (p=0.02)
|
Variable
|
Group A Mean± SD
|
Group B Mean± SD
|
P Value
|
Significance
|
|
Time taken (in seconds) for PLMA insertion
|
14.86 ± 4.46
|
11.48 ± 3.34
|
0.003
|
S
|
|
Number of attempts
|
ONE- 84%
TWO-16%
|
ONE-98%
TWO-2%
|
0.02
|
S
|
|
Incidence of failure
|
12%
|
0%
|
0.54
|
NS
|
|
Contact with secretions of patient.
|
0%
|
0%
|
NA
|
NS
|
Table5.Ease of insertion.
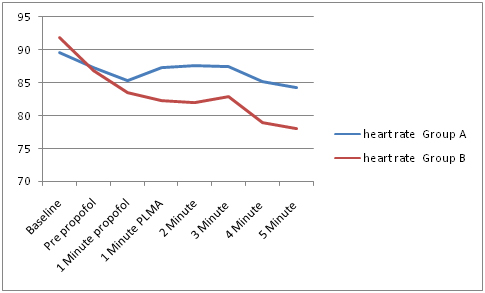
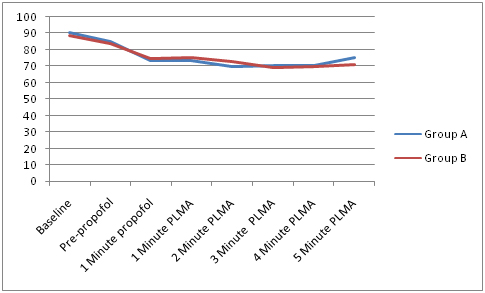
Haemodynamicpapameters (Heart rate and MAP) at Pre-propofol, 1min after propofol,1 min, 2 min, 3 min, 4 min after PLMA were comparable in both groups (Figure 1 and 2). But significant reduction in HR and MAP at 5 min after PLMAinsertion as shown in table6.
|
Variable
|
Group A Mean ± SD
|
Group B Mean± SD
|
P Value
|
Significance
|
|
Heart Rate
|
84.26 ± 14.74
|
78.06 ± 13.42
|
0.04
|
S
|
|
MAP
|
75.69 ± 9.22
|
71.28 ± 9.65
|
0.02
|
S
|
Table 6.Haemodynamic parameter at 5th min after PLMA.
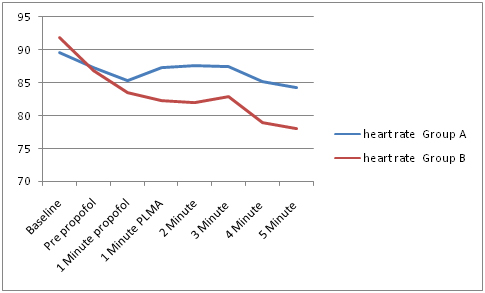
Figure 1. Heart rate distribution.
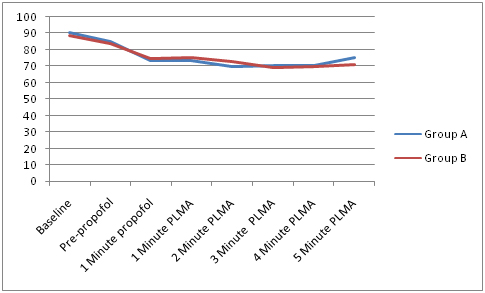
Figure 2. mean arterial pressure distribution.
None of the patients showed any complication in group B and in group A one patient showed blood on PLMA and two patient complained sore throat (Table 7).
|
|
Group A
|
Group B
|
P value
|
|
Trauma n(%)
|
1(2)
|
0
|
NA
|
|
Blood on device n(%)
|
1(2)
|
0
|
NA
|
|
Sore throat n(%)
|
2021 Copyright OAT. All rights reserv
2(4)
|
0
|
NA
|
|
Difficulty swallowing n(%)
|
0
|
0
|
NA
|
Table7.Complications.
Discussion
LMA allows unobstructed airway and ventilation without the need to hold facemask or intubations.Classical LMA has certain advantages compared to endotracheal intubation such as haemodynamic stability at induction and emergence, reduced anaesthetic requirements for airway tolerance, lower frequency of coughing during emergence and a lower incidence of sore throat. The limitations are increased risk of gastric insufflation, gastro-oesophageal reflux and risk of aspiration of regurgitated gastric contents when using the CLMA [18,19].
Propofol is routinely used induction drug in the doses of 2 to 3 mg kg-1. Apart from adequate depth of anaesthesia, factors which affect LMA insertion are mouth opening, MMP grade of the patient, jaw relaxation and coughing.
Masahiroet al.[17] found that propofol alone at clinical dosage did not completely control responses to LMA insertion. Adjuvants like midazolam[11] or Dexmedetomidine[12] facilitate the insertion.
In our study both the groups were comparable with respect to the age(p=0.12), sex(p=0.83), BMI(p=0.98), and ASA grading(p=0.54), inter-incisor distance (p=0.76) and modified Mallampatti classification(p=0.55) and baseline hemodynamics.
Patel MG et al.[4] found full jaw relaxation in 93.3% of cases of PLMA insertion in unparalyzed patients using sevoflurane and oral midazolam in children. In our study group B had more number of fully relaxed jaw (98%) when compared to group A (84%).The result of six parameters of PLMA insertion in our study were similar to that found by HanciV et al.[26]although they studied the drugs for endotracheal intubation without muscle relaxant.
In our study mean score of all six variables was found to be significantly low (p<0.05) in group B (6.38±0.69) when compared to group A (7.04±1.08) which indicates that dexmedetomidine with propofol produced a significant improvement in PLMA insertion conditions.
The subjective smoothness of PLMA insertion was assessed either to be easy or difficult.The time taken for PLMA insertion and the number of attempts has been used as a parameter assessing the ease of PLMA insertion.Many investigators have studied the ease of insertion of LMA when using neuromuscular blockers[19,20,21]but our study was done without neuromuscular blockers.Brimacombeet al.[21]showed no difference between the two techniques. However, it cannot be assumed that use of muscle relaxants has no influence on the ease of insertion.
Lopez-Gil et al.[15] Brimacombeet al.[16]reported PLMA insertion time of 33 sec using propofol induction along with remifentanil with either digital or introducer tool technique. The mean time taken for PLMA insertion was significantly less (p=0.003) in group B (11.48±3.34sec) compared to group A (14.86±4.46sec) in our study. The time taken depends upon the criteria defining time interval, the operator, as well as the placement technique.
Evans et al.[22] have not shown significant differences in insertion success between digital and introducer techniques[21,22]. The introducer technique was chosen in all the patients included in our study for uniformity.
Brimacombe, Kelleret al.[23] found that using the insertion tool may require less time (15sec)to place PLMA with insertion tool in compare to digital insertion(23 sec) in study using neuromuscular blocker.
Brimacombeet al.[23] found that the first time success rate of PLMA insertion was 98% when using muscle relaxant. In our study the incidence of successful insertion of PLMA in the first attempt was 84% in group A and 98% in group B. However this difference was not statistically significant. In our study, there was no failure in group B, whereas there were four failures in group A. this might be due to the better ease of insertion seen in the group B but the result was statistically not significant.
Two manoeuvres were used in this study head tilt- chin lift and up-down manoeuvres. However, Jun et al.[24] found that the head position had no influence on the ease of PLMA insertion instead the head position can be selected according to individual patient’s position.
The baseline HR and MAP were comparable. Intraoperatively HR and MAP were comparable in both groups except at 5 minutes Post PLMA value where HR and MAP were significantly low in groupB (p<0.05). Similarly, Evanset al.[22] found a small reduction in heart rate at 5 min after PLMA insertion and significant decreases in mean arterial pressure at 1 and 5 min after PLMA insertion
None of the patients showed any postoperative complication in group B and in group A one patient showed blood on PLMA and two patient complained Sore throat. Cook et al.[25] found that the commonest complication was the presence of blood on PLMA on removal.
Conclusion
We conclude that:
Both the drugs are acceptable for insertion of PLMA.
Use of dexmedetomidine (at dose of 0.04 mcg kg-1)produces better conditions for insertion of PLMA as compared to midazolam (at dose of 0.003 mg kg-1)
The sympathetic response to PLMA insertion is much low in patients who receiveddexmedetomidine-propofol in comparison with respect to patients whoreceived midazolam-propofol suggesting greater haemodynamic stability
Less incidence of post-operative complications in patients received dexmedetomidine.
References
- Brain AI, McGhee TD, McAteer EJ, Thomas A, Abu Saad MA, et al. (1985)The laryngeal mask airway. Development and preliminary trials of a new type of airway. Anaesthesia 40:356-357. [Crossref]
- Mark DA (2003) Protection from aspiration with the LMA-ProSeal after vomiting: a case report.Can J Anaesth50:78-80. [Crossref]
- Na, Hyo-Seok et al. (2016) Effect of Paralysis at the Time of ProSeal Laryngeal Mask Airway Insertion on Pharyngolaryngeal Morbidities. A Randomized Trial. Ed. Scott M. Langevin. PLoS ONE 10.8: e0134130.
- Patel MG, Swadia VN, Bansal G (2010) Prospective randomized comparative study of use of PLMA and ET tube for airway management in children under general anaesthesia. Indian J Anaesth 54:109-115. [Crossref]
- Sengupta J, Sengupta M, Nag T (2014) Agents for facilitation of laryngeal mask airway insertion: A comparative study between thiopentone sodium and propofol. Ann Afr Med 13:124-129. [Crossref]
- Chan A, Nickoll E, Thornton C, DoréC, Newton DEF (1996) Spontaneous movement after injection of propofol. Anaesthesia51: 663–666. [Crossref]
- Joshi GP, Kamali A, Meng J, Rosero E, Gasanova I (2014) Effects of fentanyl administration before induction of anesthesia and placement of the Laryngeal Mask Airway: a randomized, placebo-controlled trial. J ClinAnesthesia 26: 136.[Crossref]
- Baik HJ, Kim YJ, Kim JH (2009)Lidocaine given intravenously improves conditions for laryngeal mask airway insertion during propofol target-controlled infusion.Eur J Anaesthesiol 26:377-381. [Crossref]
- Aghamohammadi, Eydi M, Hosseinzadeh H, AmiriRahimi M, Golzari SE (2013) Assessment of Mini-Dose Succinylcholine Effect on FacilitatingLaryngeal Mask Airway Insertion. JCardiovascThorac Res 5: 17–21. [Crossref]
- Krasowski MD, Hong X, Hopfinger AJ, Harrison NL (2002) 4D-QSAR analysis of a set of propofol analogues: mapping binding sites for an anaesthetic phenol on the GABA(A) receptor. J Med Chem 45:3210-3221. [Crossref]
- Bhaskar P, Malik A, Kapoor R, Kohli M, Agarwal J, et al. (2010) Effect of midazolam premedication on the dose of propofol for laryngeal mask airway insertion in children. JAnaesthesiolClinPharmacol 26:503-506. [Crossref]
- Eren G, Cukurova Z, Demir G, Hergunsel O, Kozanhan B, et al. (2011) Comparison of dexmedetomidine and three different doses of midazolam in preoperative sedation. J AnaesthesiolClinPharmacol 27:367-372. [Crossref]
- Uzümcügil F, Canbay O, Celebi N, Karagoz AH, Ozgen S (2008) Comparison of dexmedetomidine-propofol vs. fentanyl-propofol for laryngeal mask insertion. Eur J Anaesthesiol 25:675-680. [Crossref]
- Ghatak T, Singh D, Kapoor R, Bogra J (2012) Effects of addition of ketamine, fentanyl and saline with Propofol induction on hemodynamics and laryngeal mask airway insertion conditions in oral clonidine premedicatedchildren.Saudi J Anaesth 6:140-144. [Crossref]
- Singh R, Arora M, Vajifdar H (2011) Randomized doubleblind comparison of ketaminepropofol and fentanylpropofol for the insertion of laryngeal mask airway in children.J AnaesthesiolClinPharmacol 27:91-96. [Crossref]
- Muzi M, Robinson BJ, Ebert TJ, O'Brien TJ (1996) Induction of anesthesia and tracheal intubation with sevoflurane in adults.Anesthesiology 85:536-543. [Crossref]
- Kanazawa M, Nitta M, Murata T, Suzuki T (2006) Increased Dosage of Propofol in Anesthesia Induction Cannot Control the Patient’s Responses to Insertion of a Laryngeal Mask Airway.Tokai J ExpClin Med 31: 35-38. [Crossref]
- Lopez-Gil M, Brimacombe J, Garcia G (2005)A randomized non-crossover study comparing the Proseal and Classic laryngeal mask airway in anaesthetized children. Br J Anaesth 95: 827-830. [Crossref]
- Brimacombe J, Kelly C, Berry A (2001) Gastric insufflation with the Proseal laryngeal mask.AnaesthAnalg 92:1614-1615. [Crossref]
- Lee AK, Tey JB, Lim Y, Sia AT (2009) Comparision of the single use LMA supreme with the reusuableProseal LMA for anaesthesia in gynaecologicallaproscopic surgery. Anaesth Intensive Care 37:815-819. [Crossref]
- Brimacombe J, Berry A (1993) Neuromuscular block and insertion of the laryngeal mask airway. Br J anaesth 71:166-167.
- Evans NR, Gardener SV, James MF, King JA, Roux P, et al. (2002)Theproseal laryngeal mask: results of a descriptive trail with experience of 300 cases. Br J Anaesth88:534-539. [Crossref]
- Brimacombe J, Keller C (2000) The Proseal laryngeal mask airway. A randomized, crossover study with the standard laryngeal mask airway in paralyzed, anaesthetized patients. Anaesthesiology 93:104-109. [Crossref]
- Jun JH, Baik HJ, Kim JH, Kim YJ, Chang RN (2011) Comparision of the ease of laryngeal mask airway Proseal insertion and the presence of a difficult airway. Korean J Anaesthesiol 60: 244-249. [Crossref]
- Cook TM, Nolan JP, Verghese C, Strube PJ, Less M, et al. (2002) Randomized crossover comparsion of the Proseal with the classic laryngeal mask airway in unparalyzed anaesthetized patients. Br J Anaesth88:527-533. [Crossref]
- Hancı V, Erdoğan G, Okyay RK, Yurtlu BS, Ayoğlu H, et al. (2010) Effects of fentanyl-lidocaine-propofol and dexmedetomidine-lidocaine-propofol on tracheal intubation without use of muscle relaxants. Kaohsiung J Med Sci26:244-250. [Crossref]